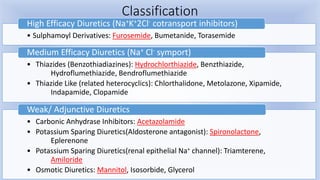
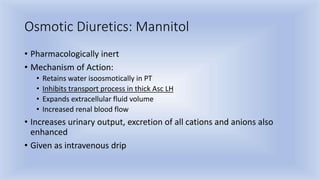
1) Diuretics are drugs that cause net loss of sodium and water in urine. They are classified as loop diuretics, thiazide diuretics, potassium-sparing diuretics, carbonic anhydrase inhibitors, and osmotic diuretics.
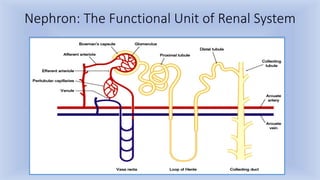
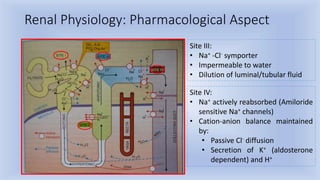
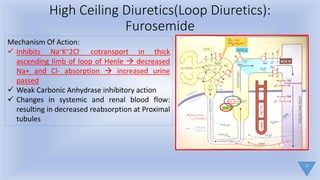
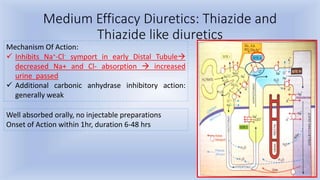
2) Loop diuretics like furosemide work by inhibiting sodium-potassium-chloride reabsorption in the loop of Henle, while thiazide diuretics inhibit sodium-chloride reabsorption in the distal tubule.
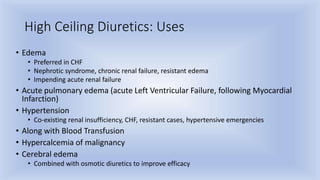
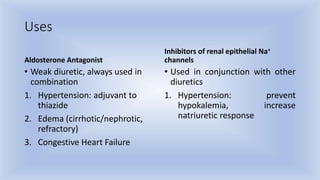
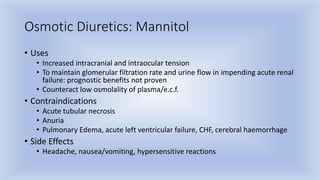
3) Diuretics are used to treat conditions like edema, hypertension, heart failure, nephrotic syndrome, and cerebral edema. Common side effects include