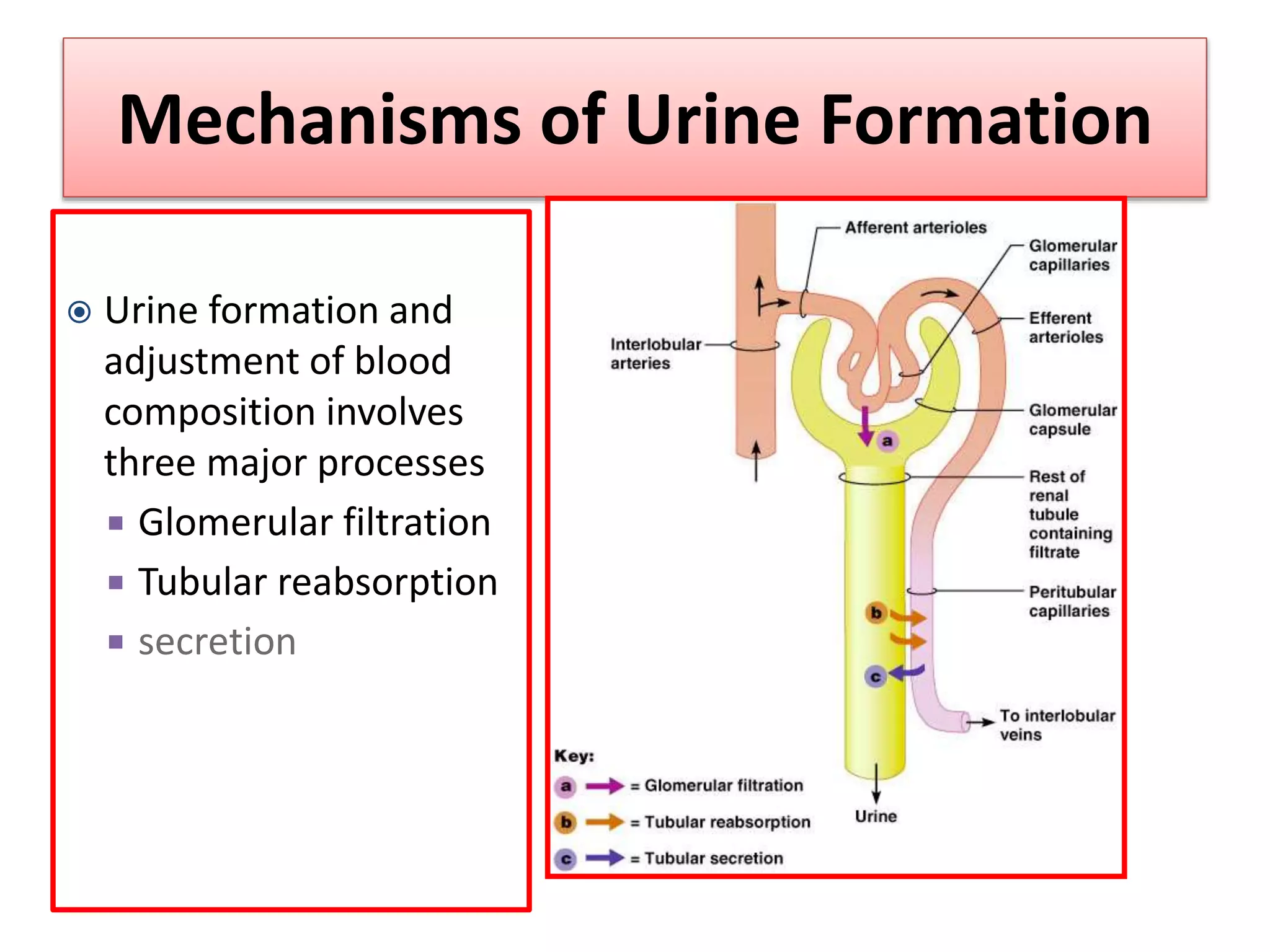
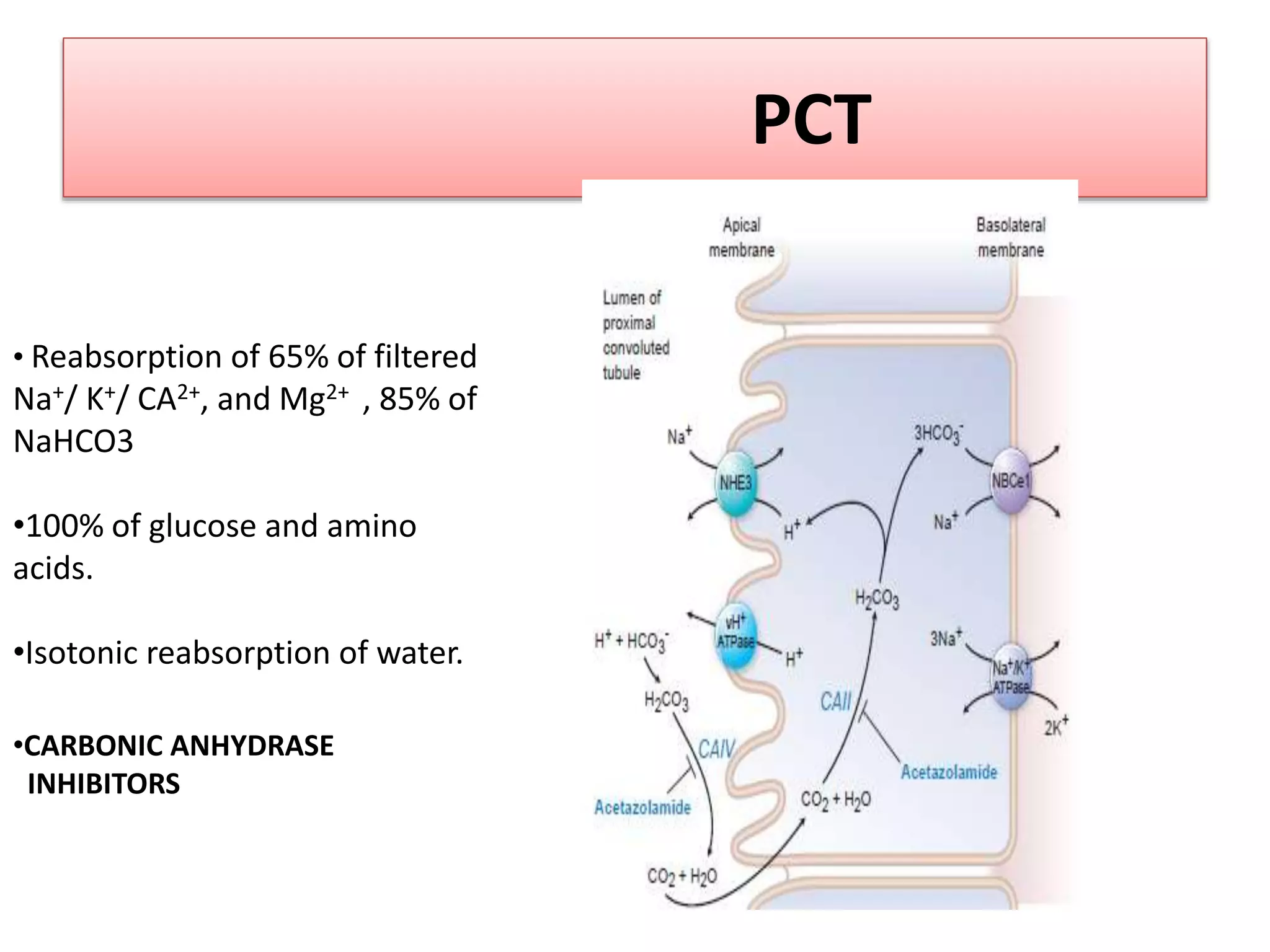
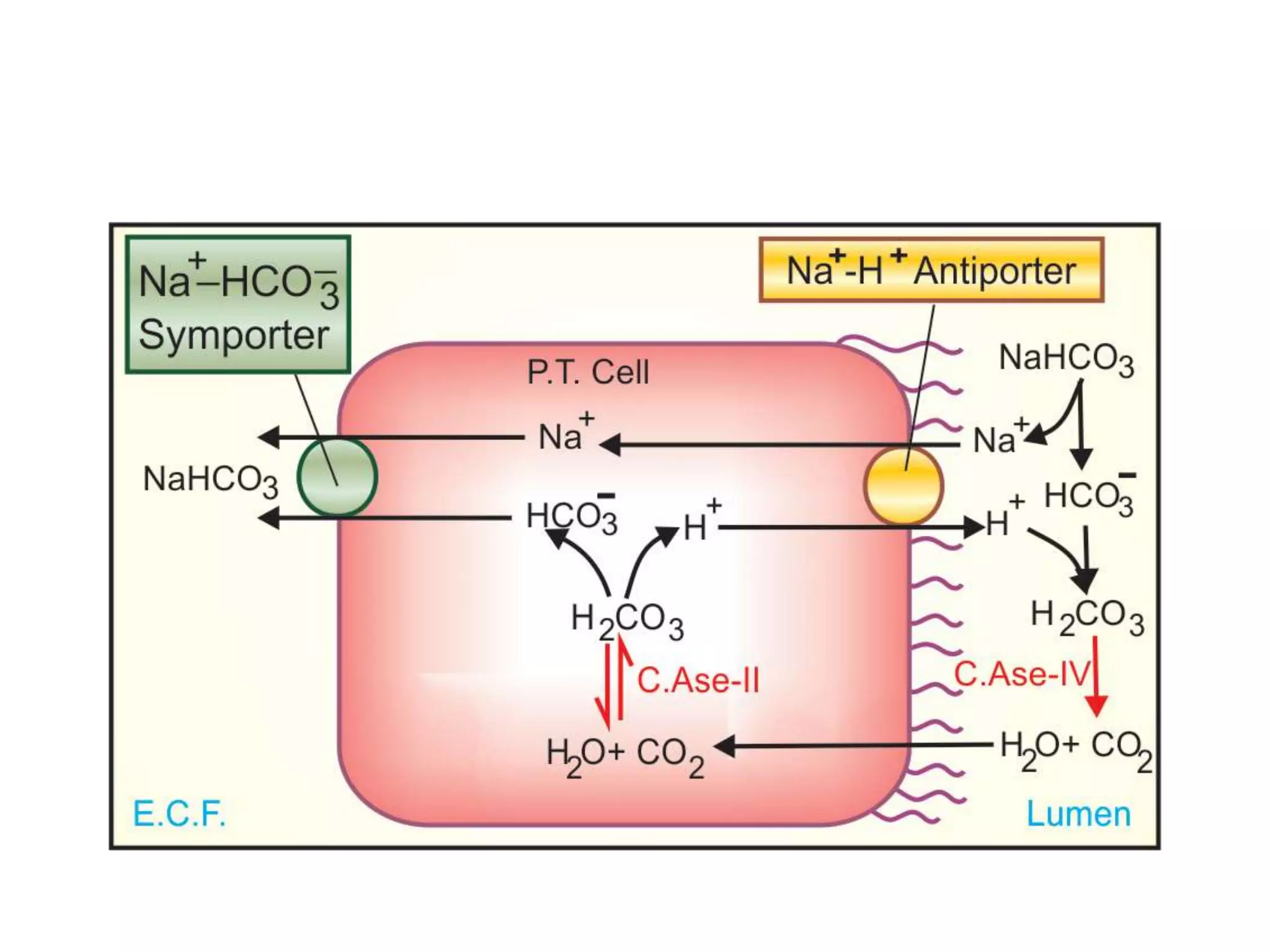
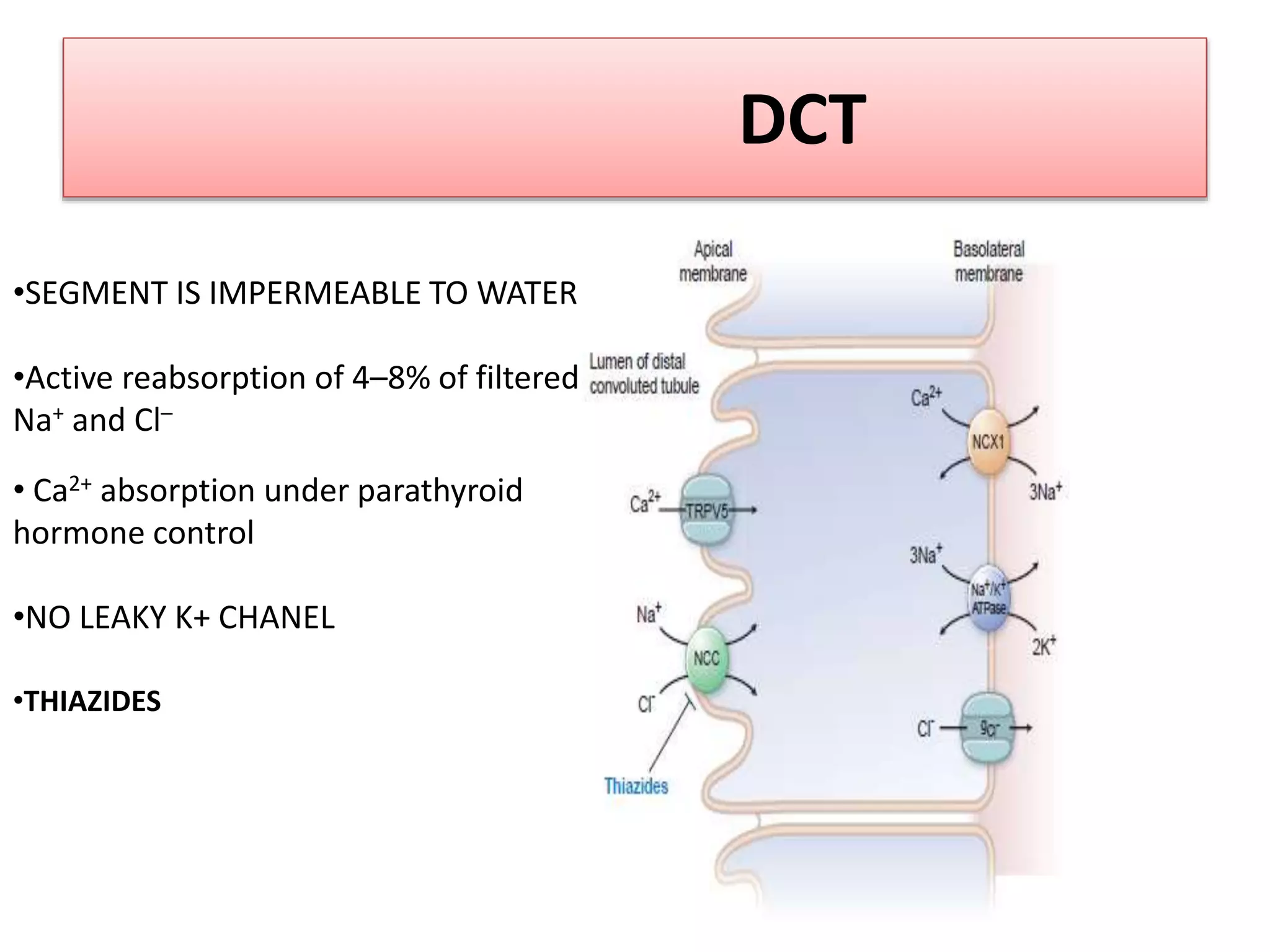
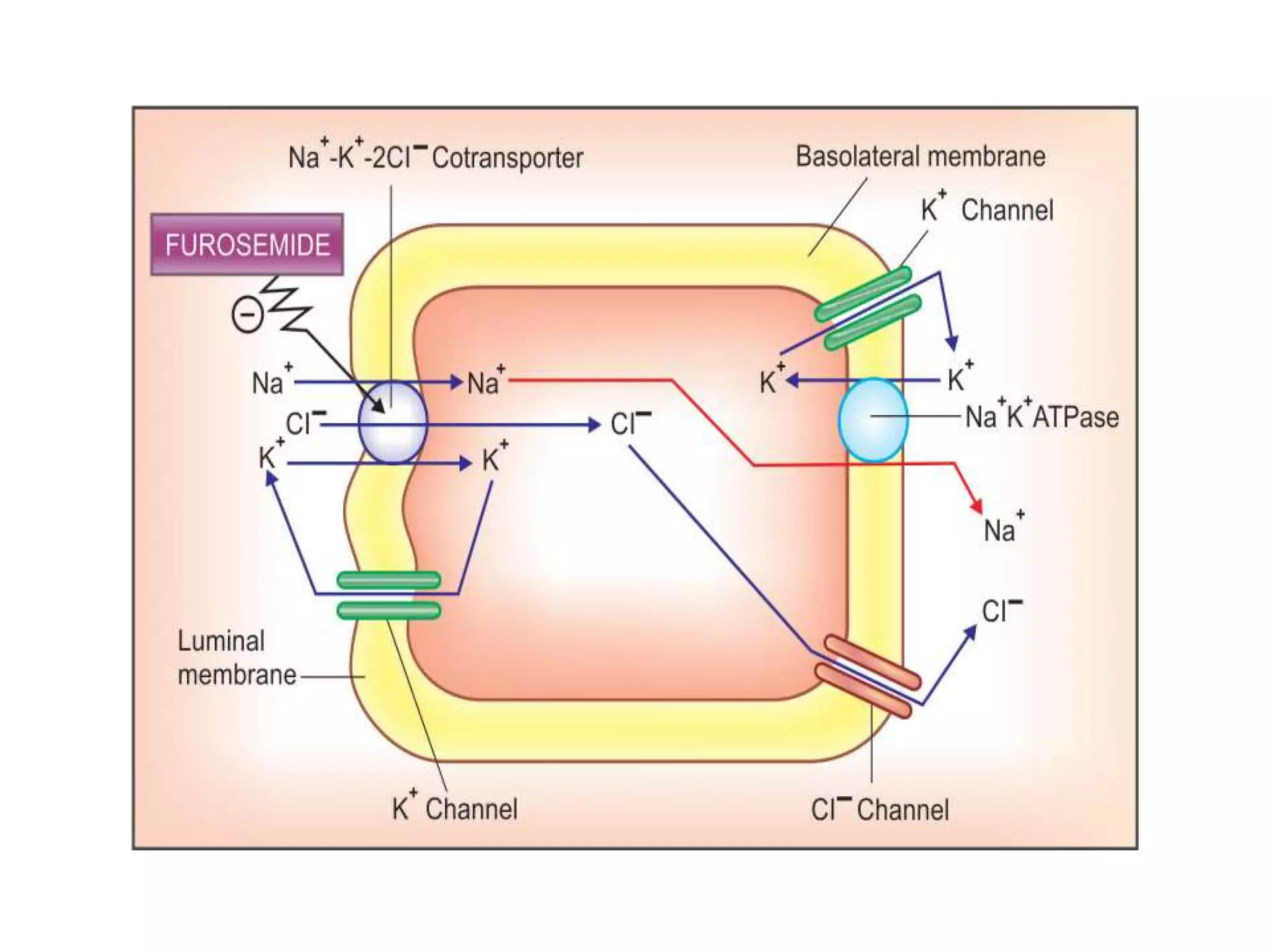
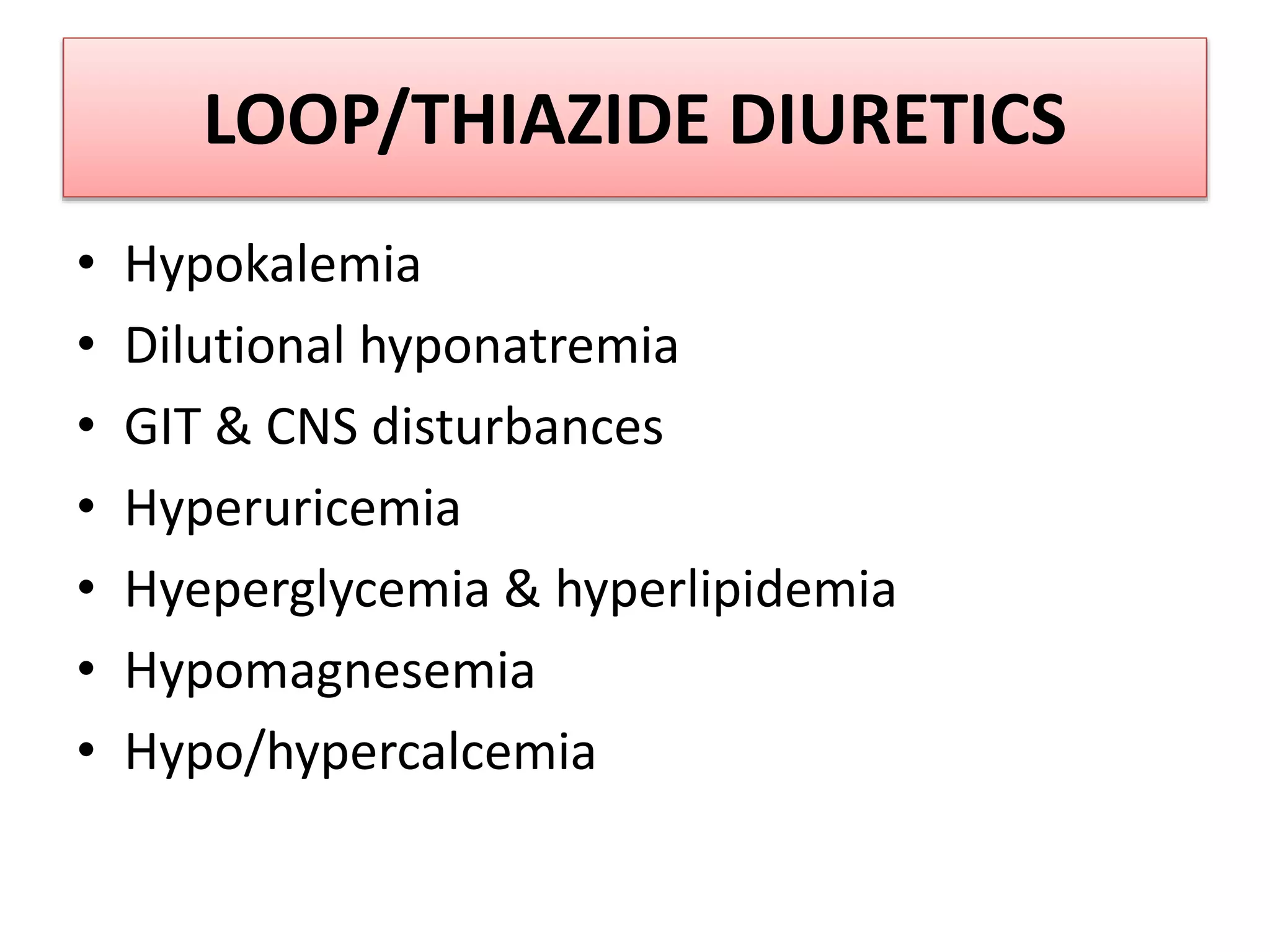
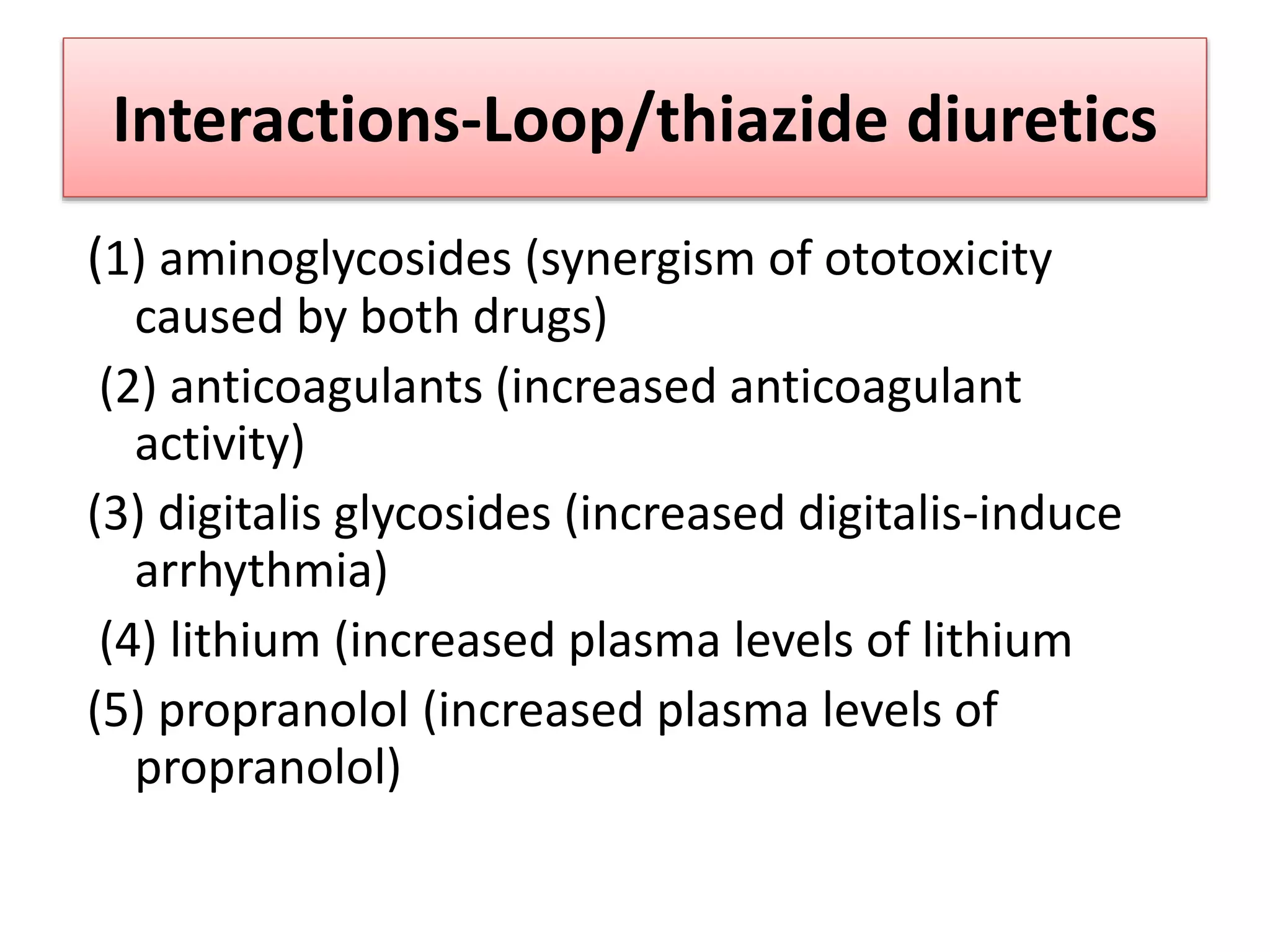
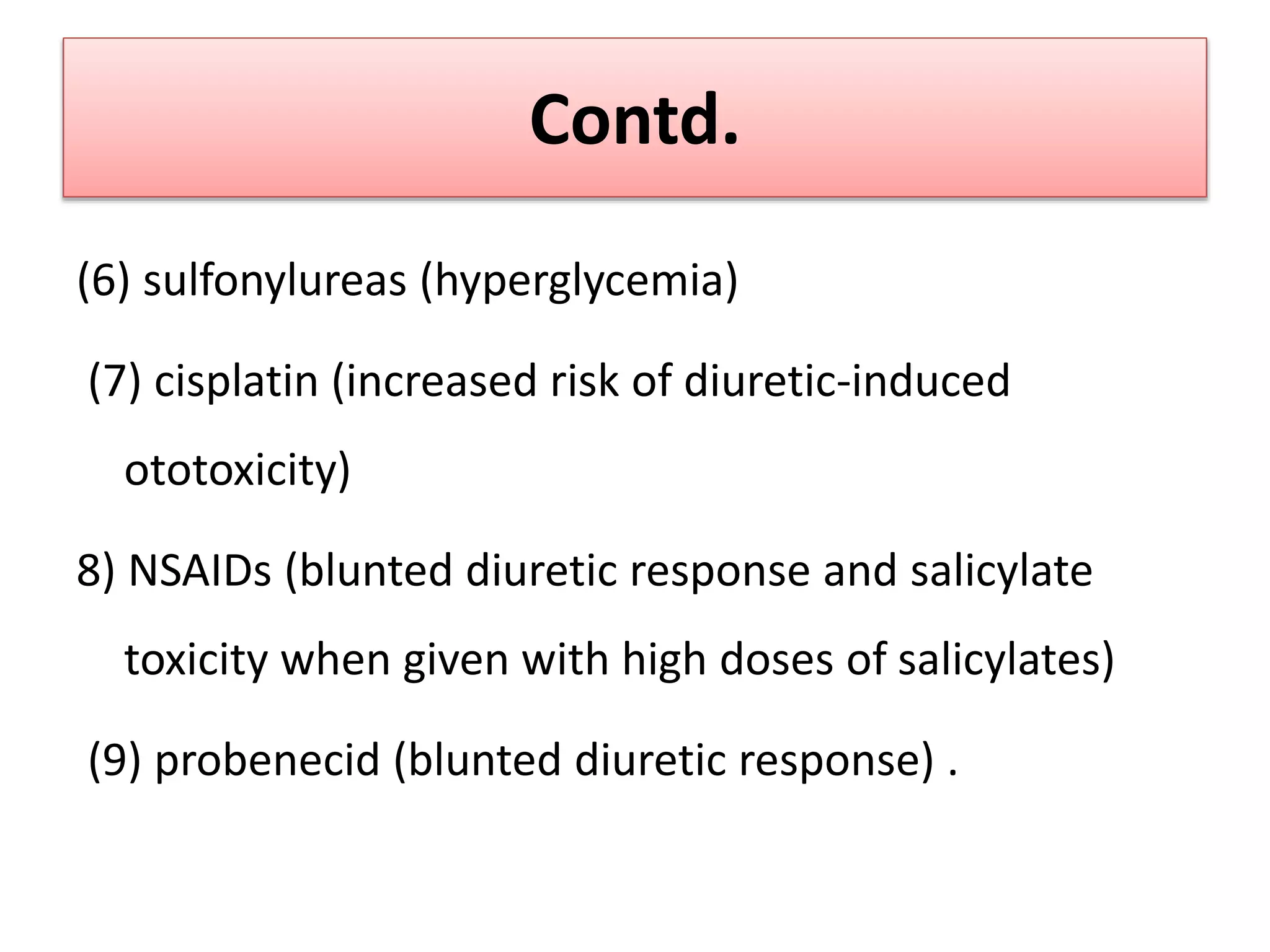
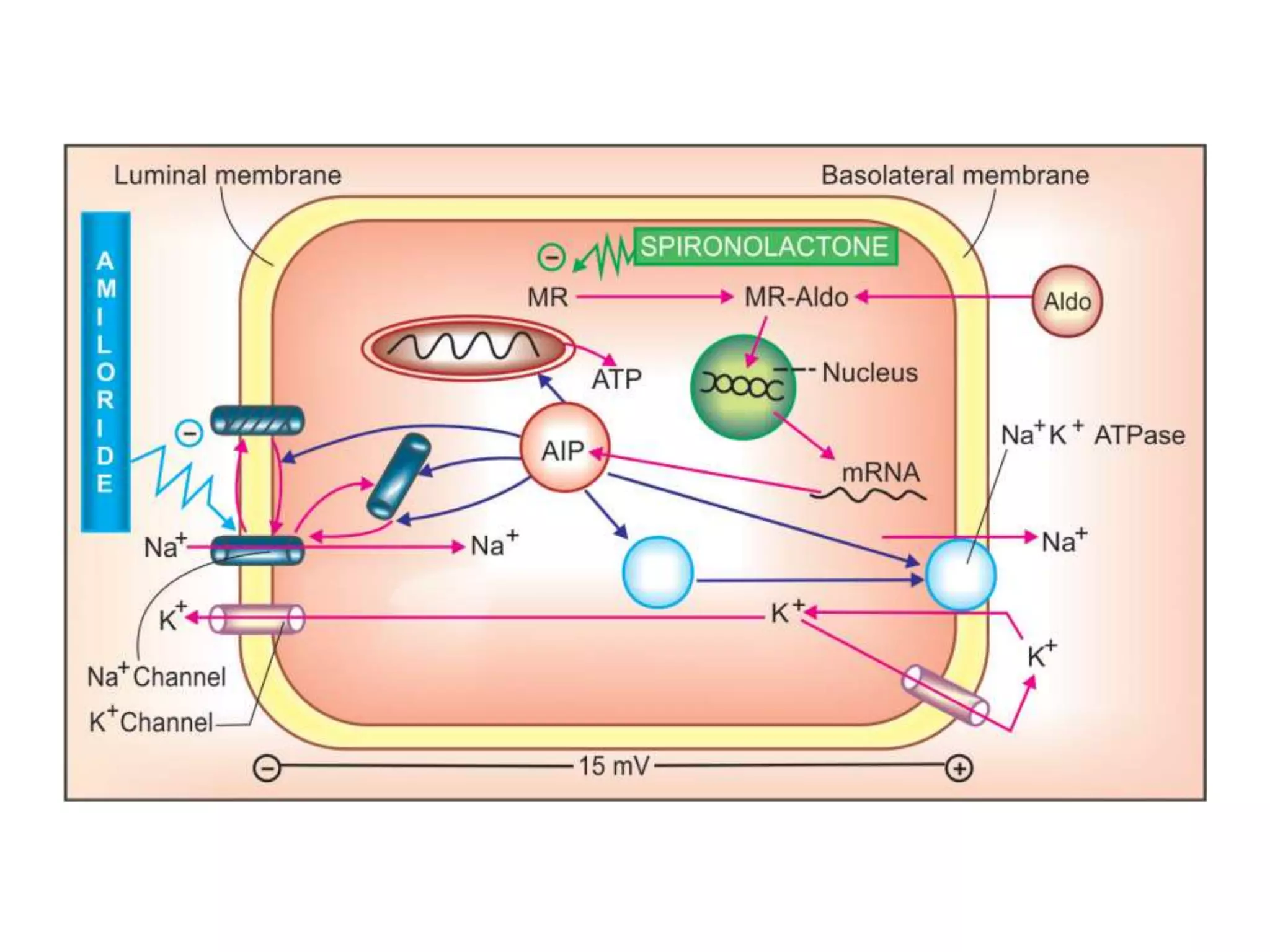
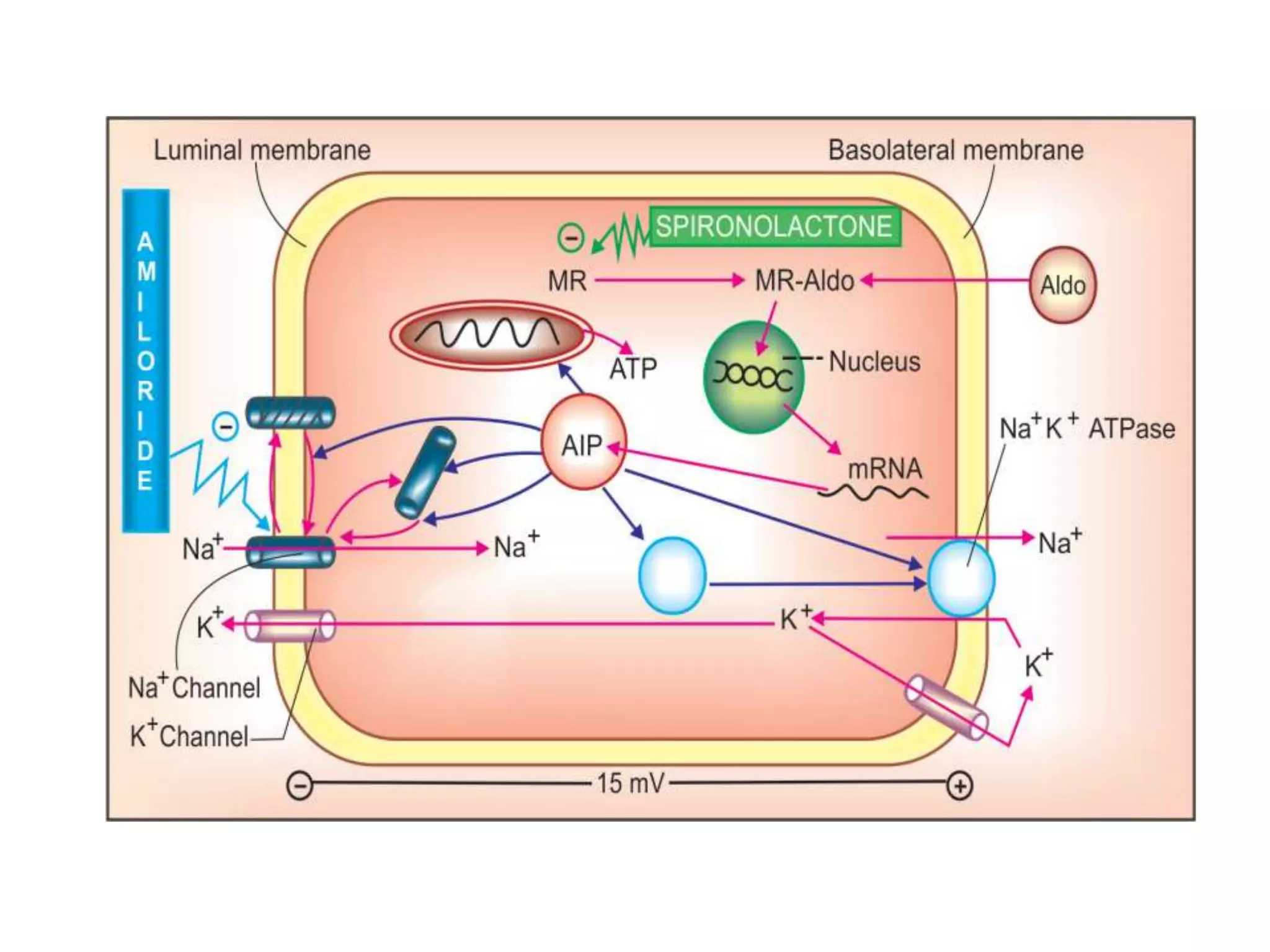
Diuretics are drugs that promote increased production of urine. The main classes of diuretics are loop diuretics, thiazide diuretics, carbonic anhydrase inhibitors, osmotic diuretics, and aldosterone antagonists. Loop diuretics such as furosemide act on the loop of Henle and are highly effective. Thiazide diuretics such as hydrochlorothiazide are commonly used to treat hypertension and edema. Carbonic anhydrase inhibitors reduce fluid production in various tissues. Osmotic diuretics work by increasing osmotic pressure in the kidney tubules. Aldosterone antagonists such as spironolactone counteract sodium retention caused by