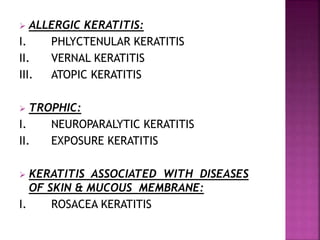
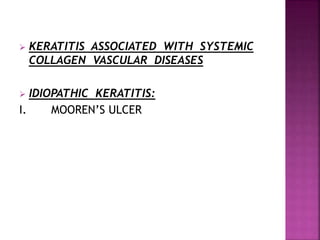
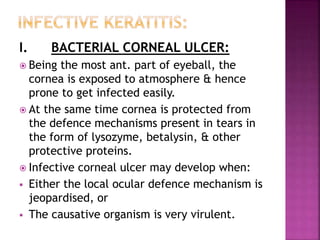
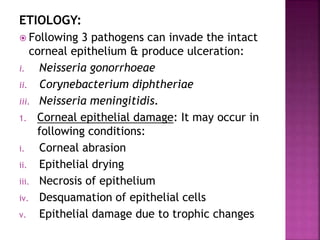
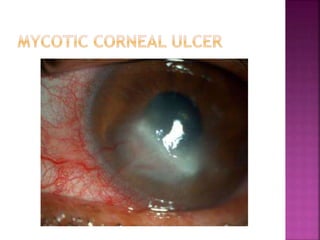
The document outlines various types of keratitis, including infective, allergic, and trophic forms, detailing their subcategories, causes, and clinical features. It emphasizes the significant role of pathogens in infective keratitis and the stages of corneal ulcer progression, alongside common treatments such as antibiotics and topical steroids. Additional insights cover specific conditions like herpes simplex keratitis and acanthamoeba keratitis, highlighting the need for targeted therapeutic approaches.
![Mode Of Infection:
1. HSV-I infection: It is acquired by kissing or
coming in close contact with a patient
suffering from herpes labialis.
2. HSV-II infection: It is transmitted to eyes of
neonates through infected genitalia of the
mother.
Ocular Lesions Of Herpes Simplex:
[A] Primary herpes:
1. Skin lesions
2. Conjunctiva-acute follicular conjunctivitis
3. Cornea](https://image.slidesharecdn.com/cornealulcers-161213145858/85/Corneal-ulcers-30-320.jpg)
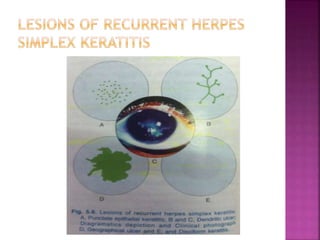
![[B] Recurrent herpes:
1. Epithelial keratitis:
i. Punctuate epithelial keratitis
ii. Dendritic ulcer
iii. Geographical ulcer
2. Stromal keratitis
i. Disciform keratitis
ii. Diffuse stromal necrotic keratitis
3. Metaherpetic keratitis](https://image.slidesharecdn.com/cornealulcers-161213145858/85/Corneal-ulcers-31-320.jpg)
![[A] Primary Ocular Herpes
Primary infection (first attack) involves a
nonimmune person.
It typically occurs in children betn 6 months &
5 yrs & in teenagers.
Clinical Features:
1. Skin lesions: Vesicular lesions may occur
involving skin of lids, periorbital region & the
lid margin.
2. Acute follicular conjunctivitis with regional
lymphadenitis is the usual.
3. Keratitis: Cornea is involved in about 50% of
the cases. The keratitis can occur as a coarse
punctuate or diffuse branching epithelial.](https://image.slidesharecdn.com/cornealulcers-161213145858/85/Corneal-ulcers-32-320.jpg)
![[B] Recurrent Ocular Herpes
The virus which lies dormant in the trigeminal
ganglion, periodically reactivates & causes
recurrent infection.
1. Epithelial keratitis:
i. Punctuate epithelial keratitis:
The initial epithelial lesions of recurrent
herpes resemble those seen in primary herpes
& may be either in the form of fine or coarse
superficial punctuate lesions.
ii. Dendritic ulcer:
Dendritic ulcer is a typical lesion of recurrent
epithelial keratitis.
The ulcer is of an irregular, zigzag linear
branching shape.](https://image.slidesharecdn.com/cornealulcers-161213145858/85/Corneal-ulcers-33-320.jpg)