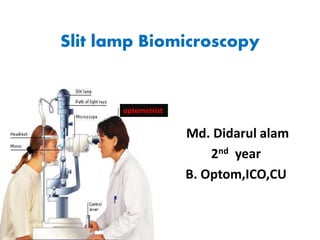
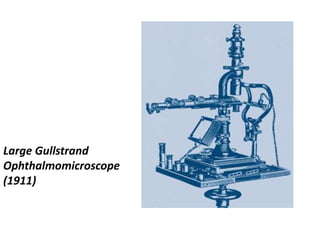
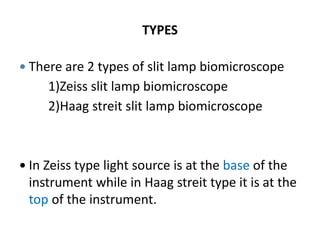
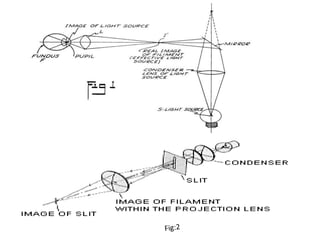
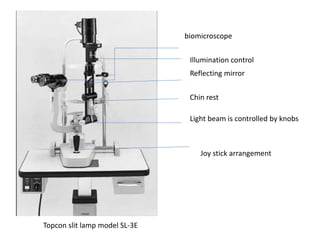
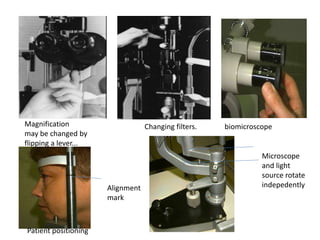
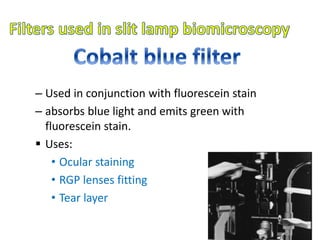
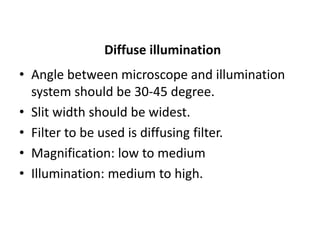
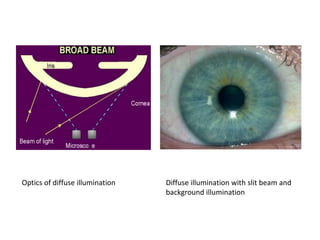
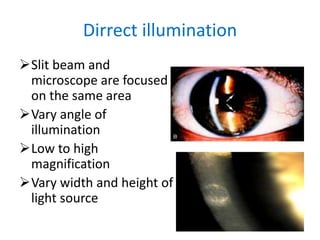
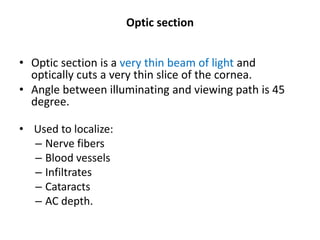
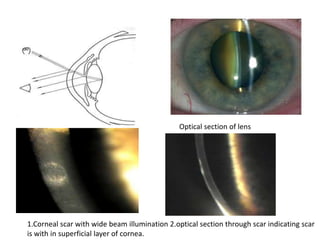
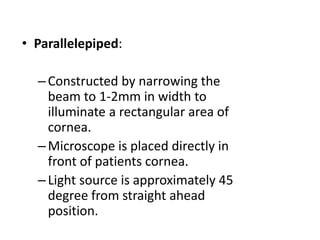
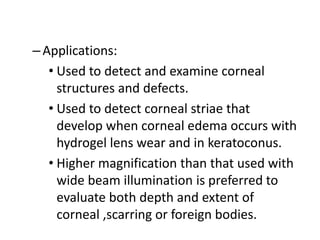
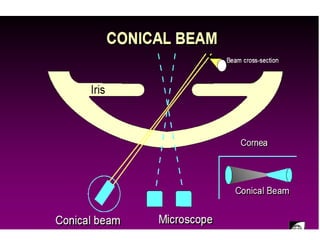
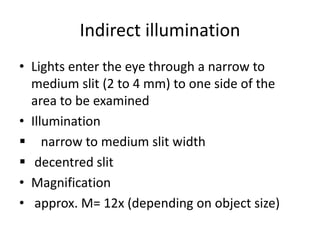
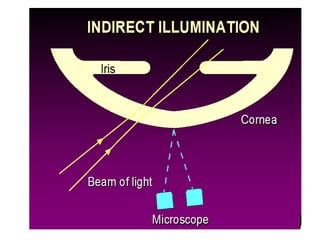
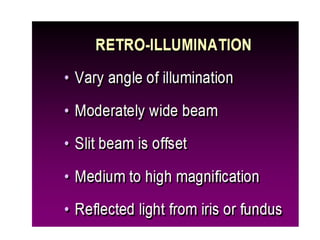
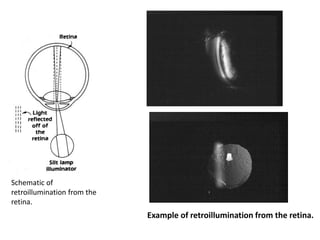
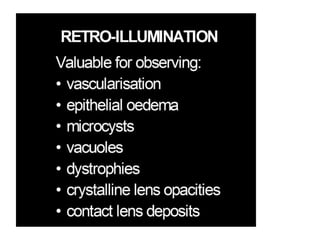
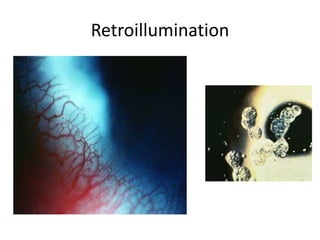
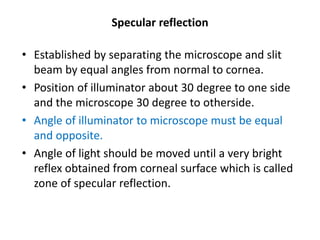
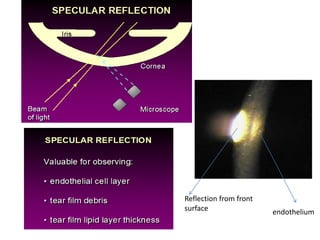
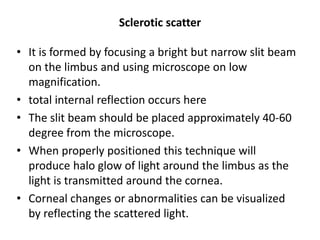
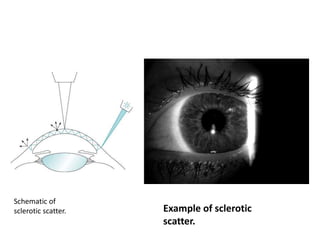
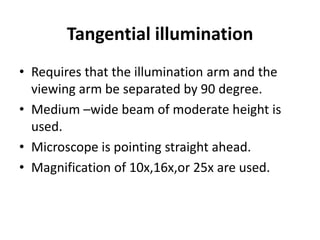
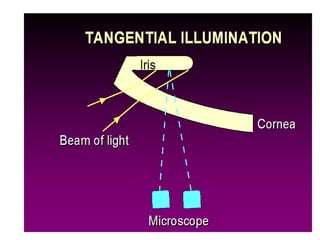
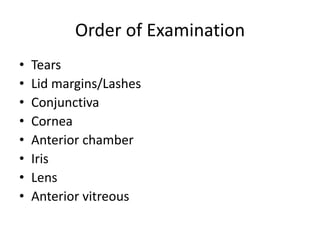
The document discusses the slit lamp biomicroscope, an important tool in optometry. It describes the history and development of the slit lamp, including key contributors. The basic components and functioning of the slit lamp are explained, including the illumination and observation systems. Different types of slit lamps and various illumination techniques used with the slit lamp like diffuse, direct, retro-illumination and their applications are outlined. The document also mentions the clinical uses of the slit lamp for diagnostic and therapeutic purposes.