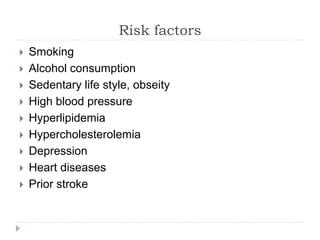
Dementia is a collective term for various medical conditions that result in cognitive decline, impacting daily life and independent functioning, primarily affecting older adults. With approximately 47 million affected globally, this number is projected to rise significantly, particularly in developing countries. The document outlines types, symptoms, risk factors, stages, diagnosis methods, and management strategies for dementia, emphasizing the need for rehabilitation and support.