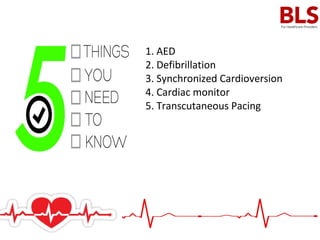
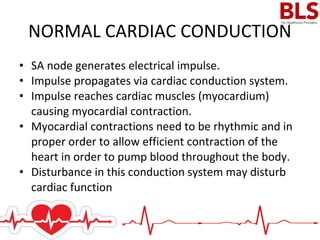
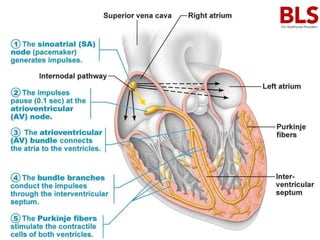
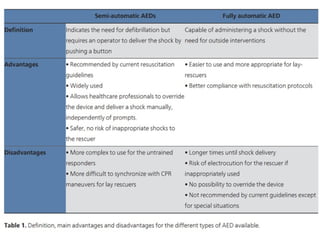
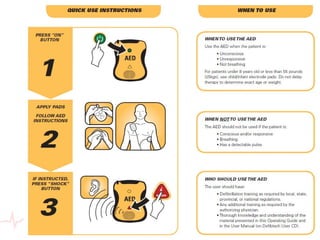
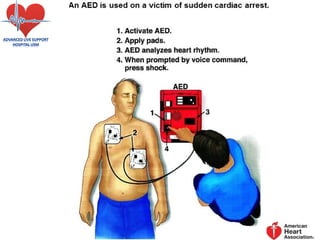
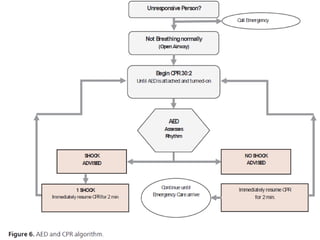
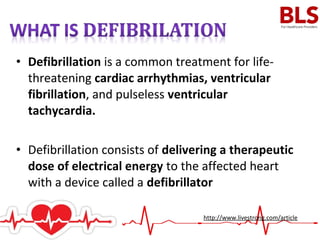
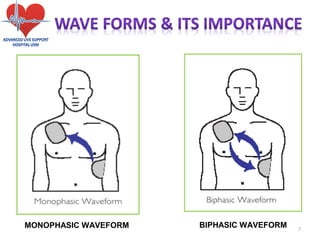
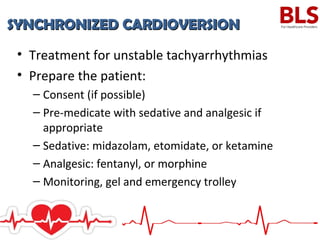
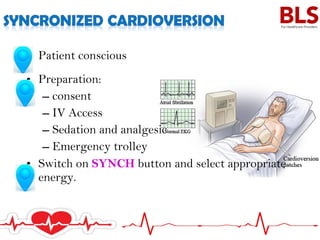
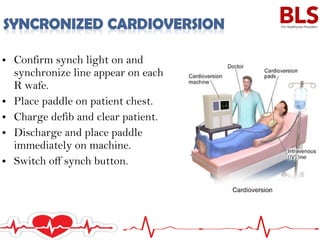
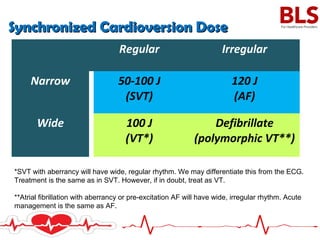
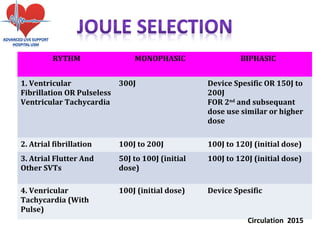
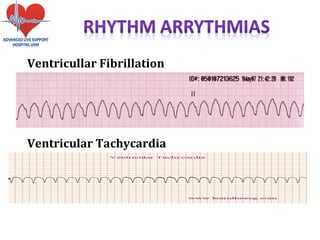
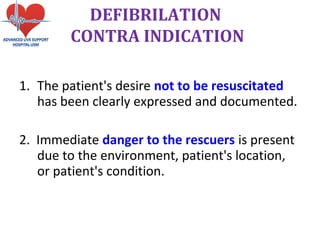
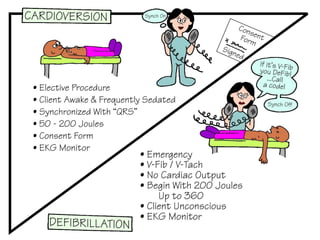
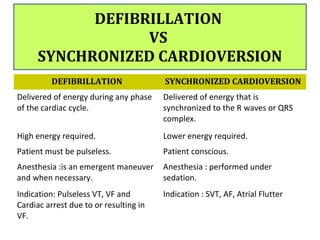
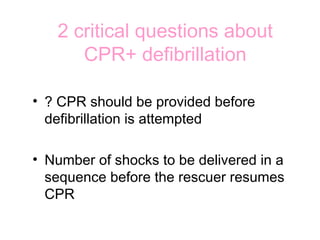
Electrical therapy involves using electrical stimulation through electrodes placed on the skin to strengthen muscles. An automated external defibrillator (AED) analyzes the heart rhythm and delivers an electric shock through pads placed on the chest to restore a normal rhythm during cardiac arrest from ventricular fibrillation or pulseless ventricular tachycardia. Defibrillation is used to treat life-threatening arrhythmias and delivers an electric shock through a defibrillator device to the heart in order to stop chaotic contractions during ventricular fibrillation. Synchronized cardioversion delivers a shock synchronized to the heartbeat to treat unstable tachyarrhythmias in conscious patients.