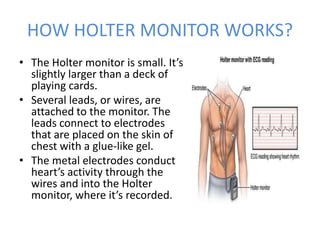
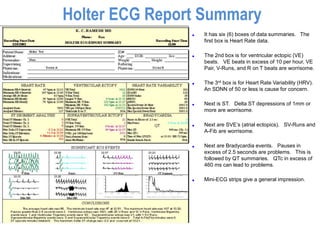
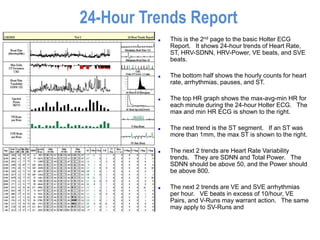
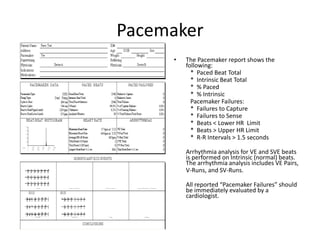
Holter monitoring involves using a portable electrocardiography device to record a patient's heart rhythm over a period of 24 to 72 hours. The device uses electrodes attached to the skin to track the heart's electrical activity. A Holter monitor can detect abnormal heart rhythms and help diagnose conditions like unexplained palpitations, syncope, or evaluate pacemaker function. The report provides summaries of heart rate, arrhythmias detected, heart rate variability, and 24-hour trends to help clinicians identify abnormal rhythms and understand their clinical significance. Holter monitoring can play a role in evaluating patients with known heart disease, suspected ischemia, cryptogenic stroke, and pacemaker function.