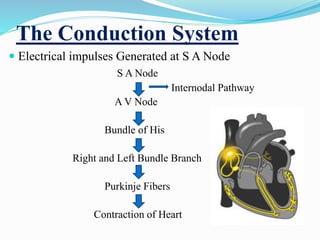
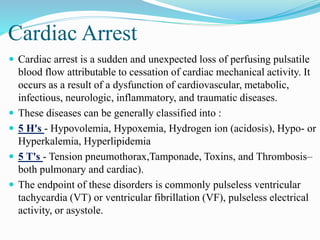
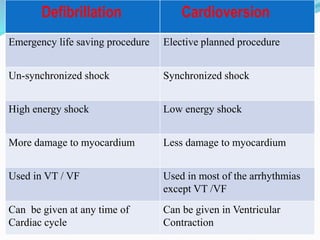
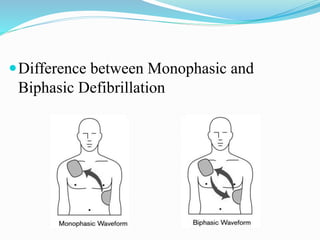
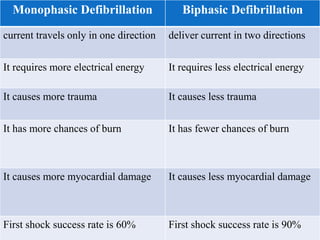
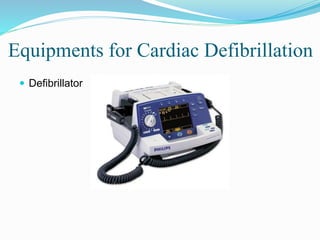
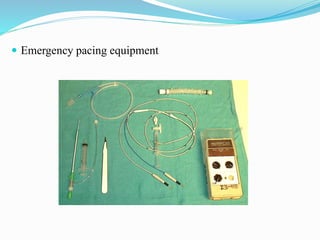
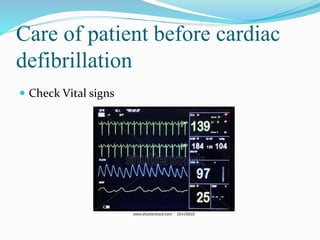
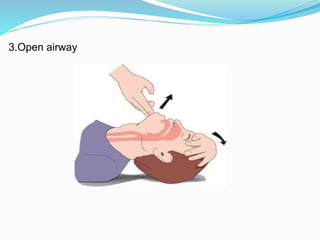
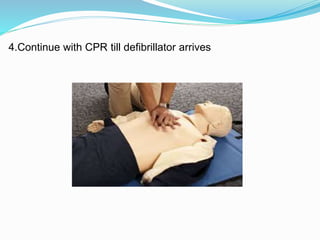
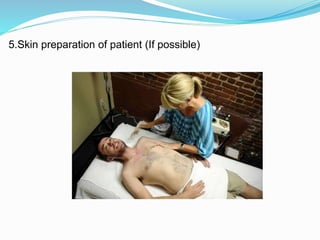
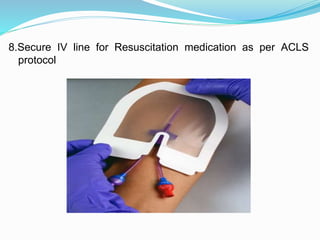
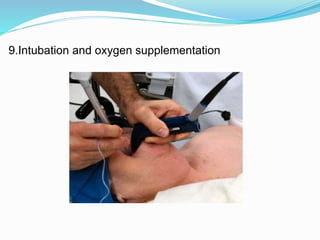
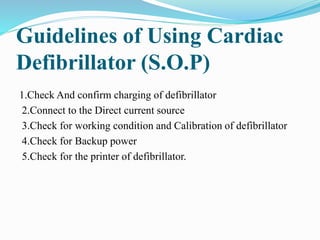
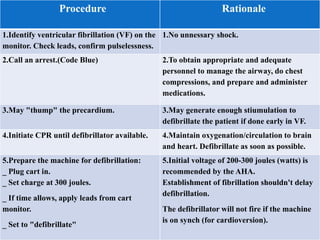
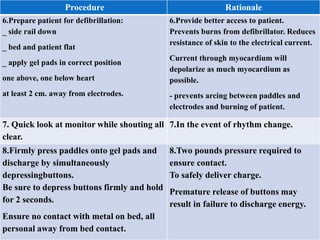
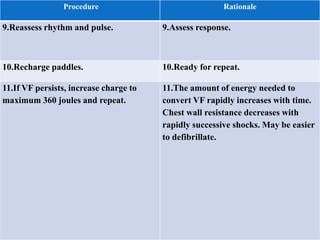
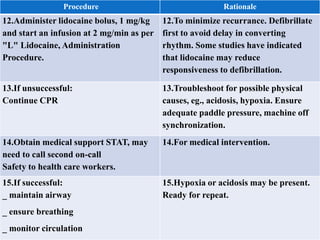
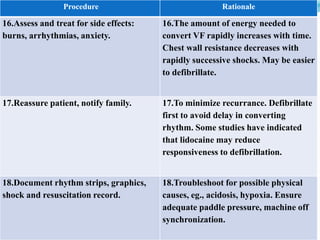
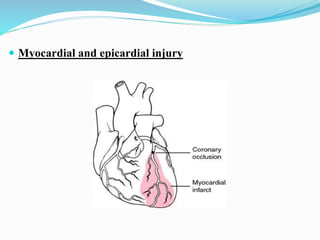
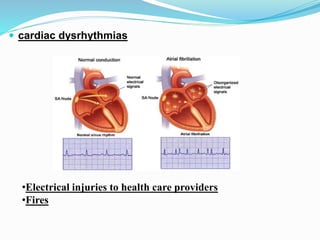
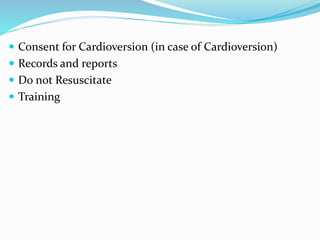
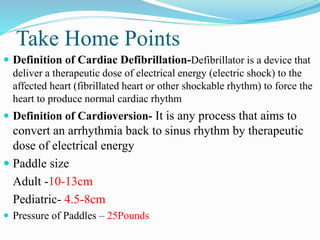
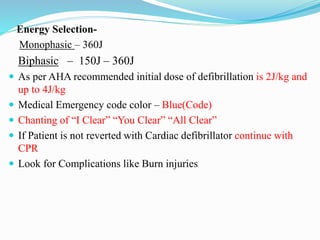
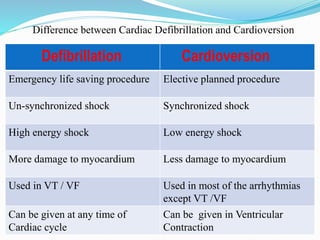
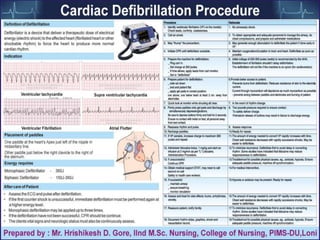
The document outlines the principles and procedures related to cardiac defibrillation, including the anatomy and physiology of the heart, types of defibrillation, and emergency procedures for managing cardiac arrest. Key differences between defibrillation and cardioversion are detailed, highlighting their applications, energy levels, and risks involved. It also covers pre- and post-procedural care, complications, and documentation requirements to ensure comprehensive patient management and legal adherence.