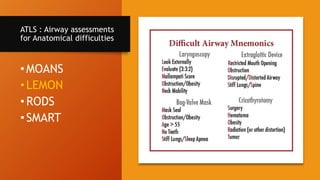
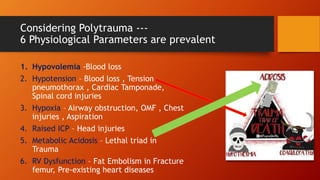
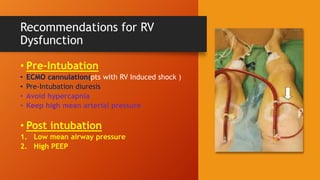
The document discusses the complexities of airway management in polytrauma patients, using a case study of a critically injured 45-year-old man to illustrate difficult airway scenarios. It emphasizes the importance of assessing physiological factors alongside anatomical challenges during intubation to prevent complications. The author advocates for integrating physiological assessments into pre-intubation preparations to enhance patient outcomes.