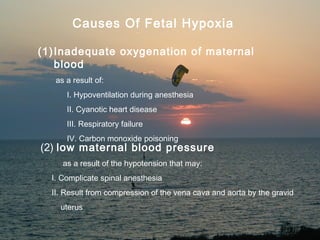
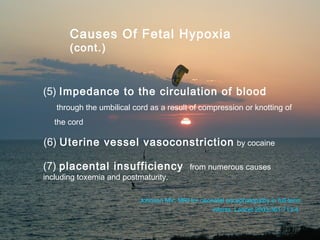
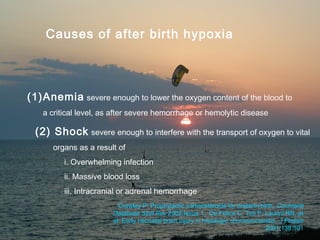
This document discusses hypoxic ischemic encephalopathy (HIE), which is brain damage caused by a lack of oxygen and blood flow around the time of birth. It defines related terms like anoxia and hypoxia. It describes the effects of HIE on different body systems. It outlines the stages of HIE based on clinical signs. It discusses causes of fetal and newborn hypoxia, pathophysiology, treatment involving supportive care and seizure management, and prognosis which depends on factors like gestational age and severity of encephalopathy. Between 15-30% of infants with HIE die or are left with permanent neurological impairments.