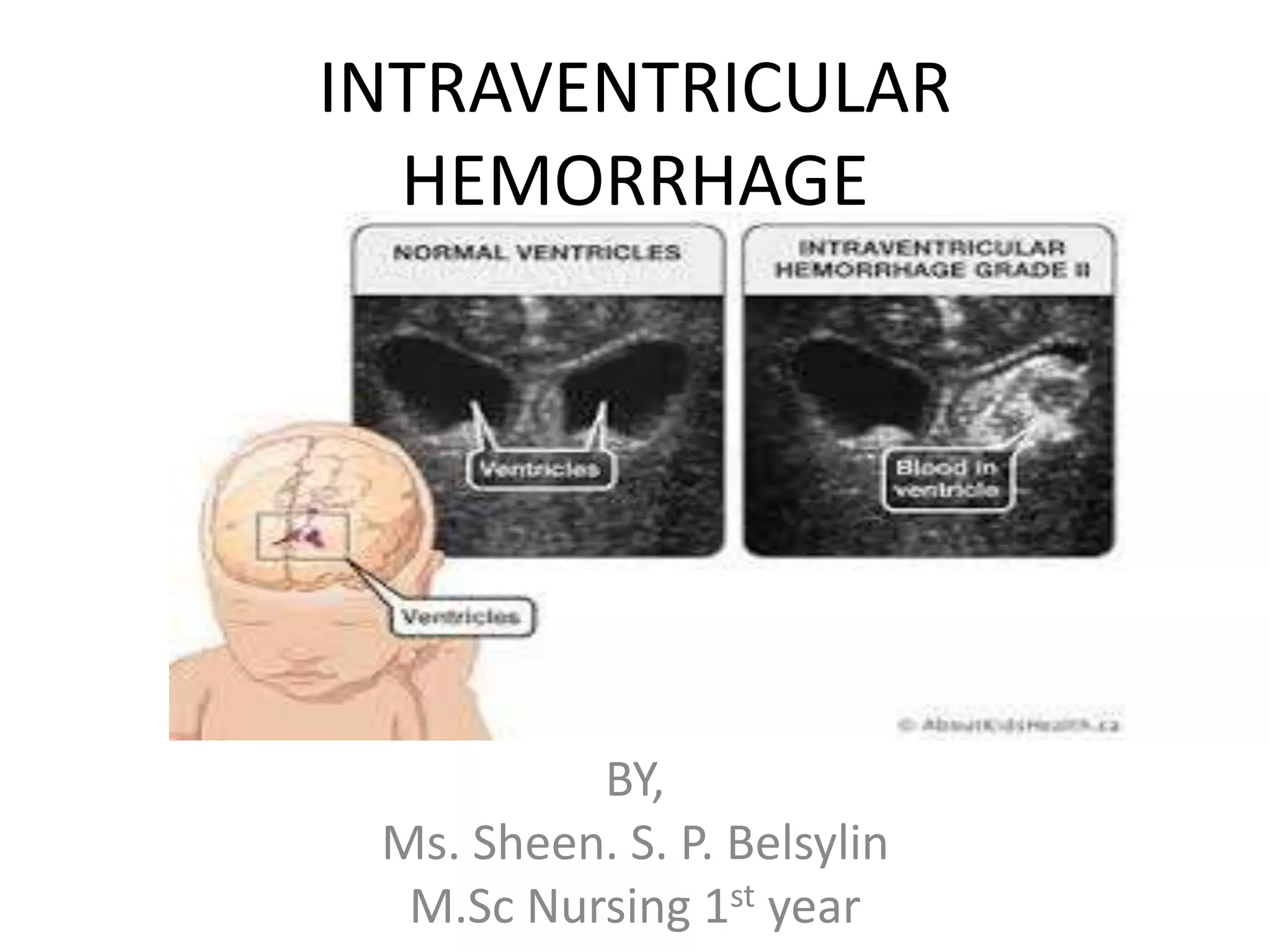
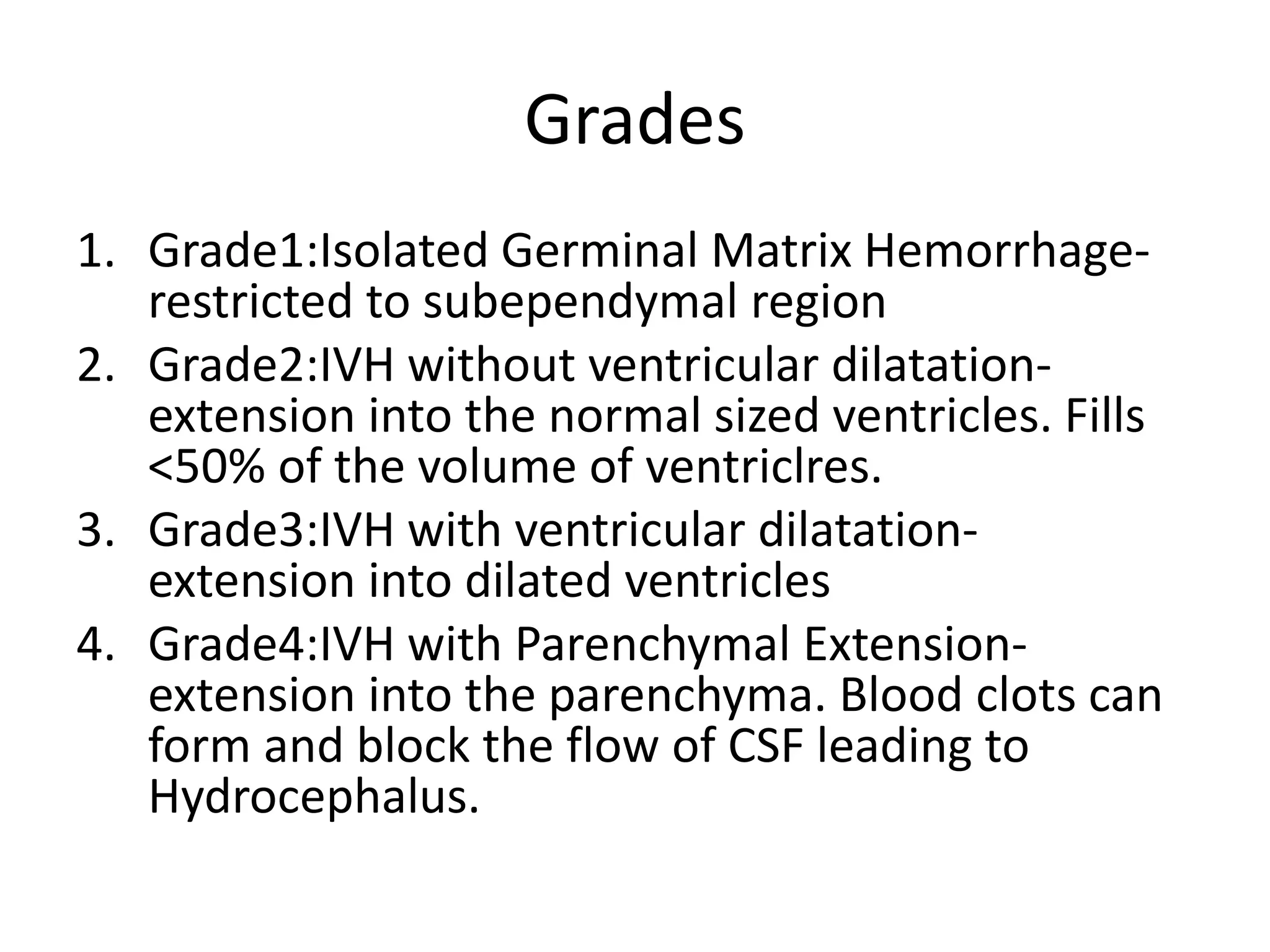
Intraventricular hemorrhage (IVH) is a common condition in premature infants, characterized by bleeding into the brain's ventricles, with higher risks associated with various medical conditions at birth. Diagnosis involves head ultrasounds, particularly for infants born before 30 weeks, while management focuses on stabilizing the infant and addressing symptoms, with no way to prevent the bleeding. Pulmonary hemorrhage, another serious condition, involves significant lung bleeding, primarily in very preterm infants, requiring urgent management to prevent high morbidity and mortality.