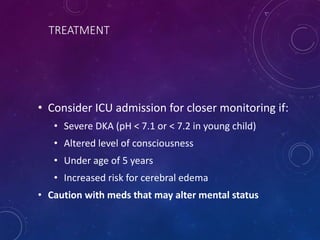
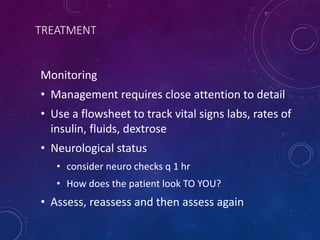
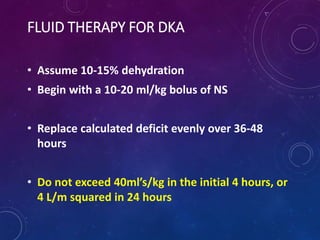
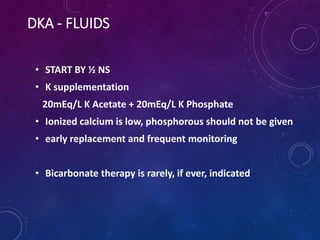
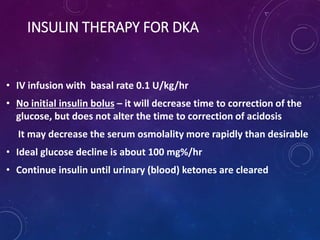
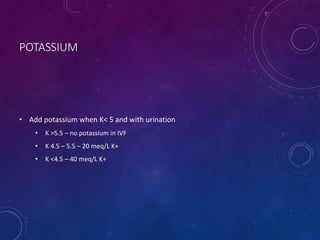
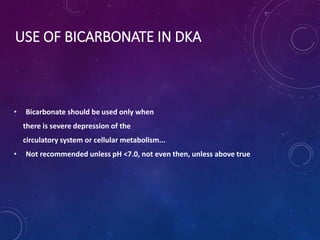
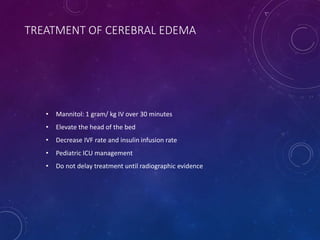
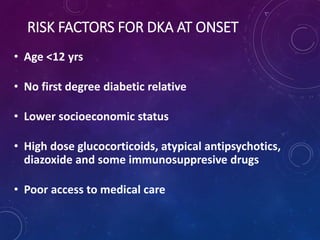
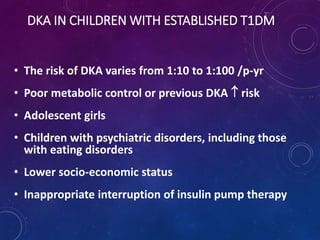
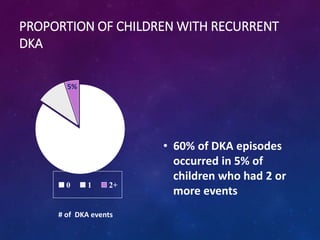
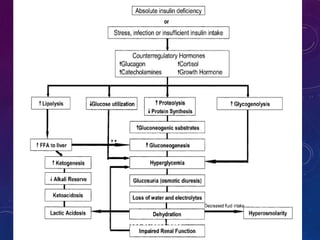
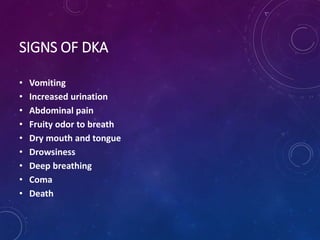
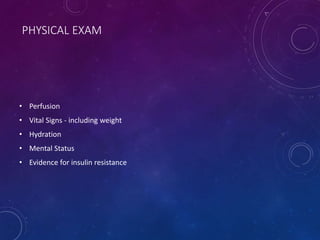
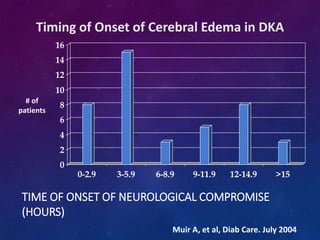
This document defines diabetic ketoacidosis (DKA) and discusses its incidence, risk factors, signs, and treatment in children. DKA is characterized by hyperglycemia, acidosis, and ketosis. The risk of DKA is higher in children under 12, those with lower socioeconomic status or no family history of diabetes. Recurrent DKA occurs in 5% of children and accounts for 60% of DKA cases. Treatment involves fluid resuscitation, insulin therapy, electrolyte replacement, and close monitoring for cerebral edema, with consideration of ICU admission for severe cases. Successful management requires attention to detail, documentation, and repeated patient examination.

![CALCULATIONS
SERUM OSMOLALITY:
2[NA+K]+ (GLUCOSE/18) + BUN/2.8
SERUM NA:
CORRECTED NA =
MEASURED NA + (1.6)(GLUCOSE - 100)/100
ANION GAP:
[NA] – ([CL]+[HCO3])
NORMALLY 12+/-2 MMOL/L](https://image.slidesharecdn.com/dka-200110105109/85/DKA-in-children-12-320.jpg)