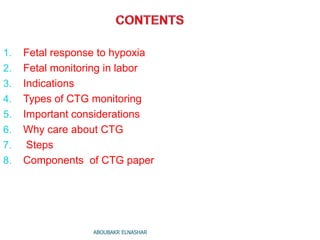
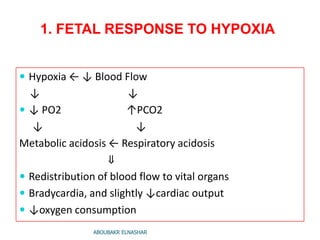
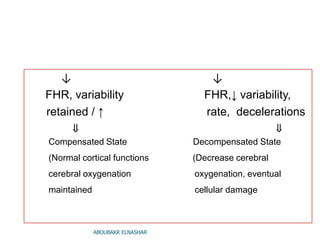
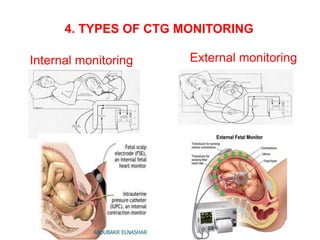
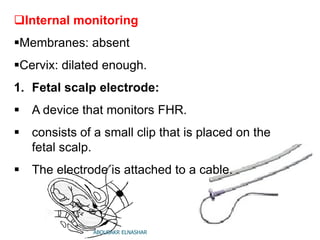
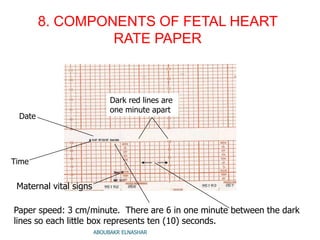
This document provides an overview of cardiotocography (CTG) monitoring during labor. It discusses the fetal response to hypoxia, indications for CTG monitoring such as high-risk pregnancies or when oxytocin is used, and the types of CTG monitoring including external and internal methods. Important considerations for CTG monitoring are highlighted, such as it being a screening rather than diagnostic tool with both high negative but low positive predictive value. The steps of external and internal CTG monitoring are outlined, as are the components of a CTG paper tracing. The document concludes with notes on CTG monitoring for litigation and education/training purposes.