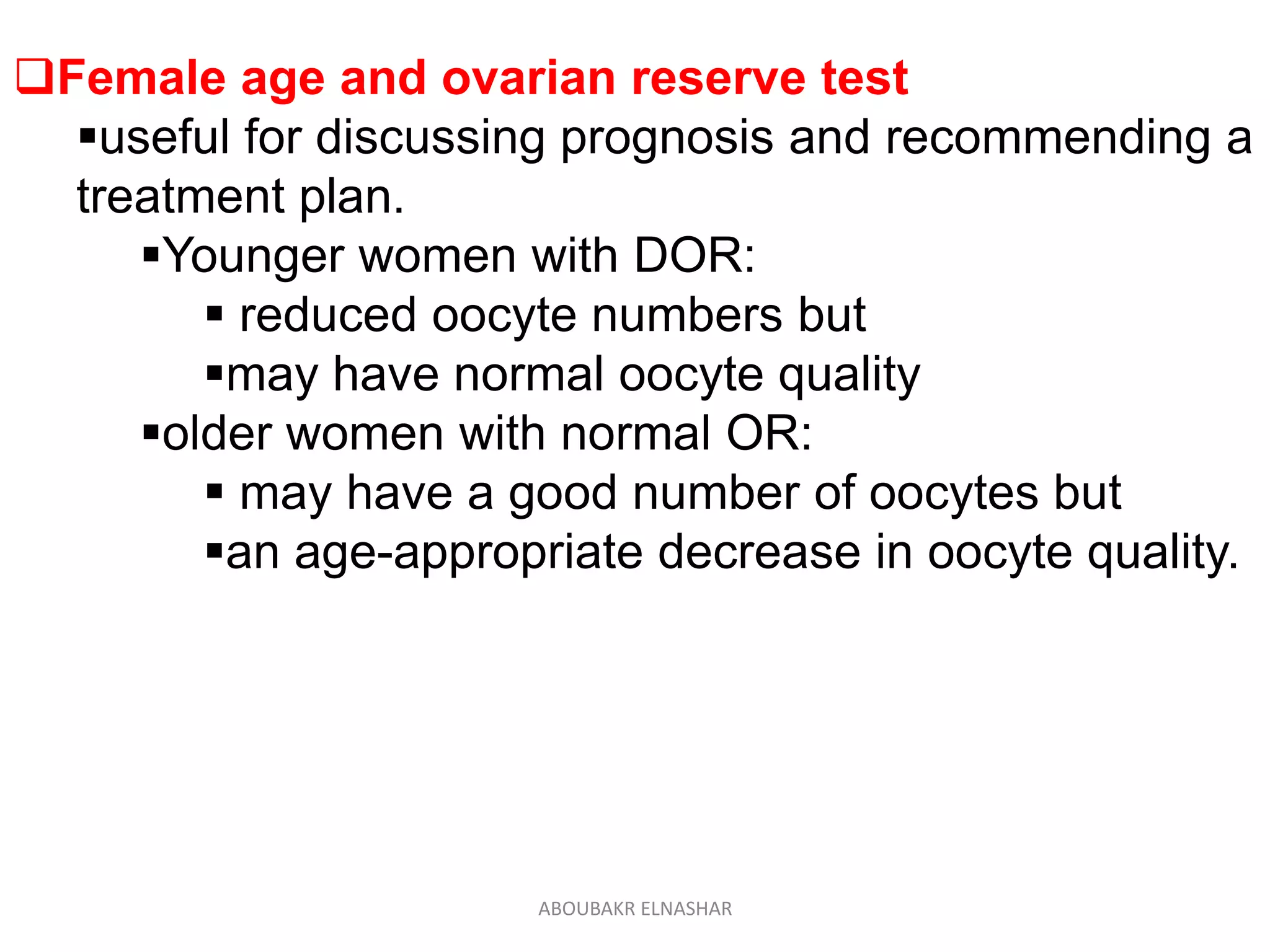
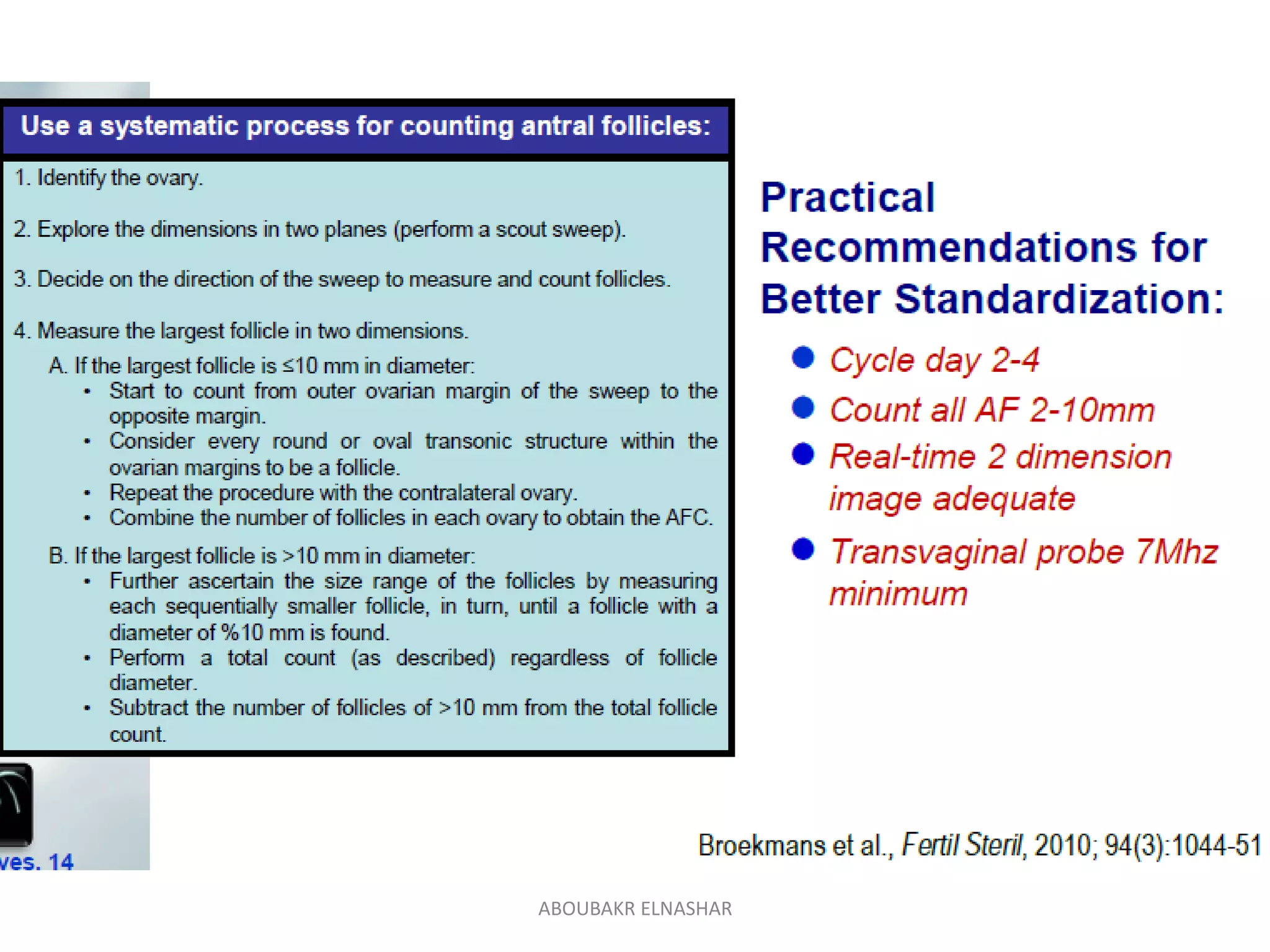
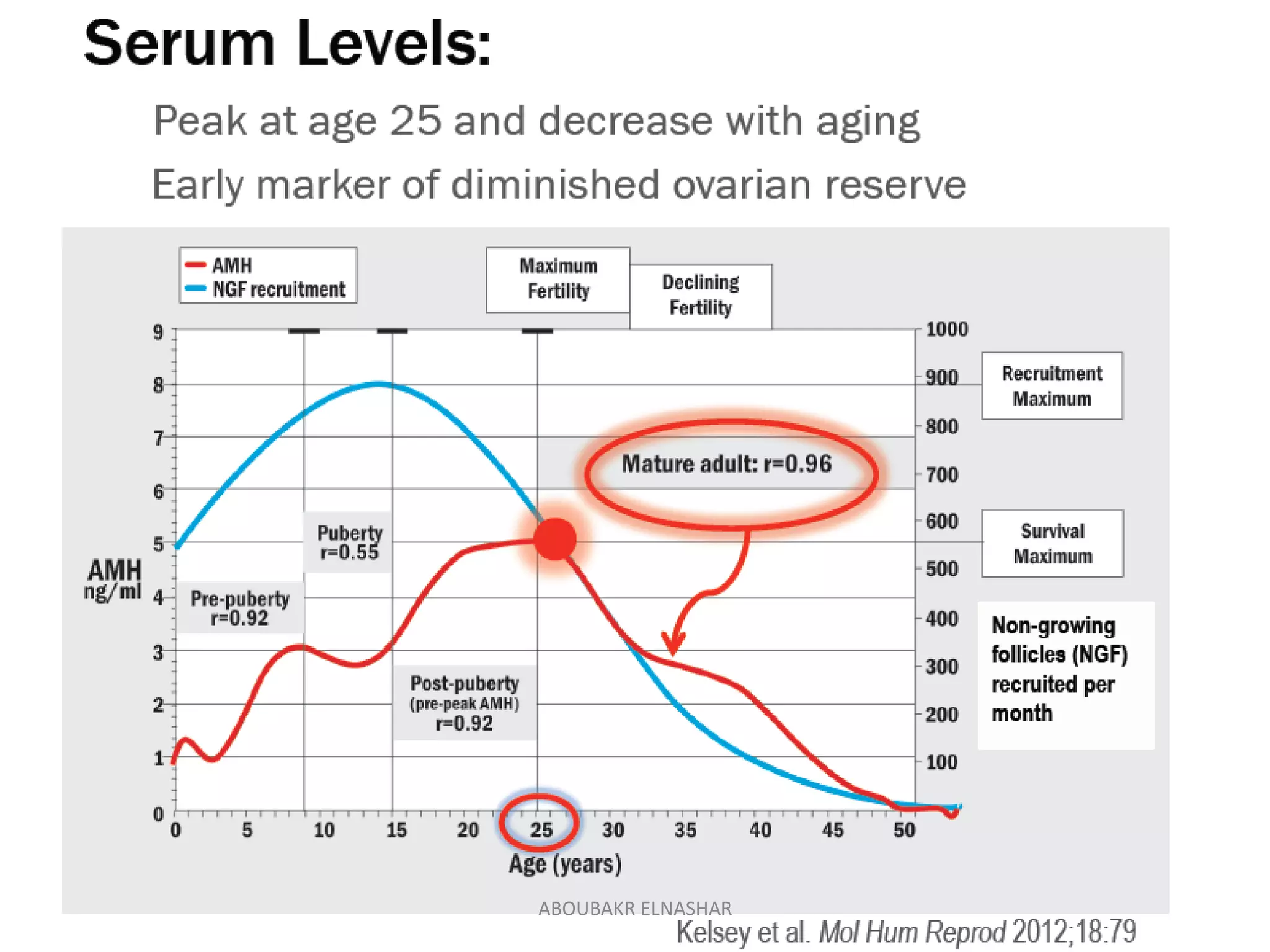
This document discusses ovarian reserve, which refers to a woman's reproductive potential and is a function of the number and quality of her remaining oocytes. It declines with age due to a reduction in both quantity and quality of oocytes. Several tests can assess ovarian reserve, including antral follicle count (AFC), anti-Müllerian hormone (AMH) levels, and follicle-stimulating hormone (FSH) levels. AFC and AMH are currently considered the best tests as they have less variability than FSH. These tests can help predict response to fertility treatments and live birth outcomes. While they provide useful information, age is still the strongest predictor of ovarian reserve and reproductive potential.