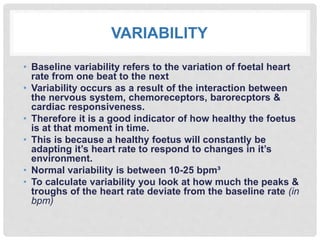
Cardiotocography (CTG) monitors the fetal heart rate and uterine contractions during pregnancy. A CTG involves using ultrasound to record the fetal heart rate and a transducer to monitor uterine contractions. Abnormal CTG results indicate the need for further investigation and may require emergency c-section if fetal distress is detected. To interpret a CTG, clinicians assess characteristics like the baseline heart rate, variability, presence of accelerations or decelerations, and number of contractions over a 10 minute period. This provides insight into fetal well-being and guides medical management during delivery.