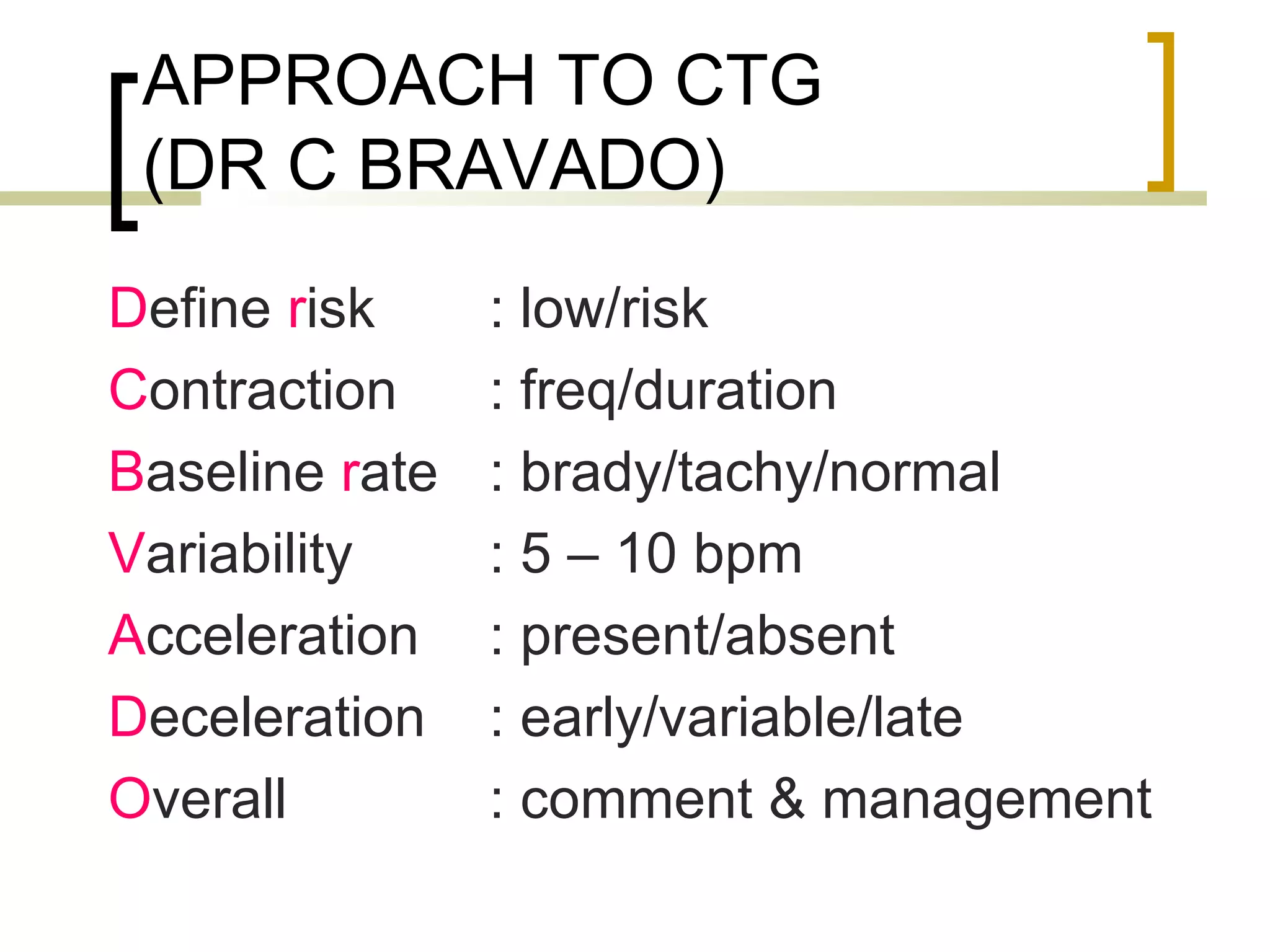
The document provides definitions and descriptions of key terms used in cardiotocography (CTG) including:
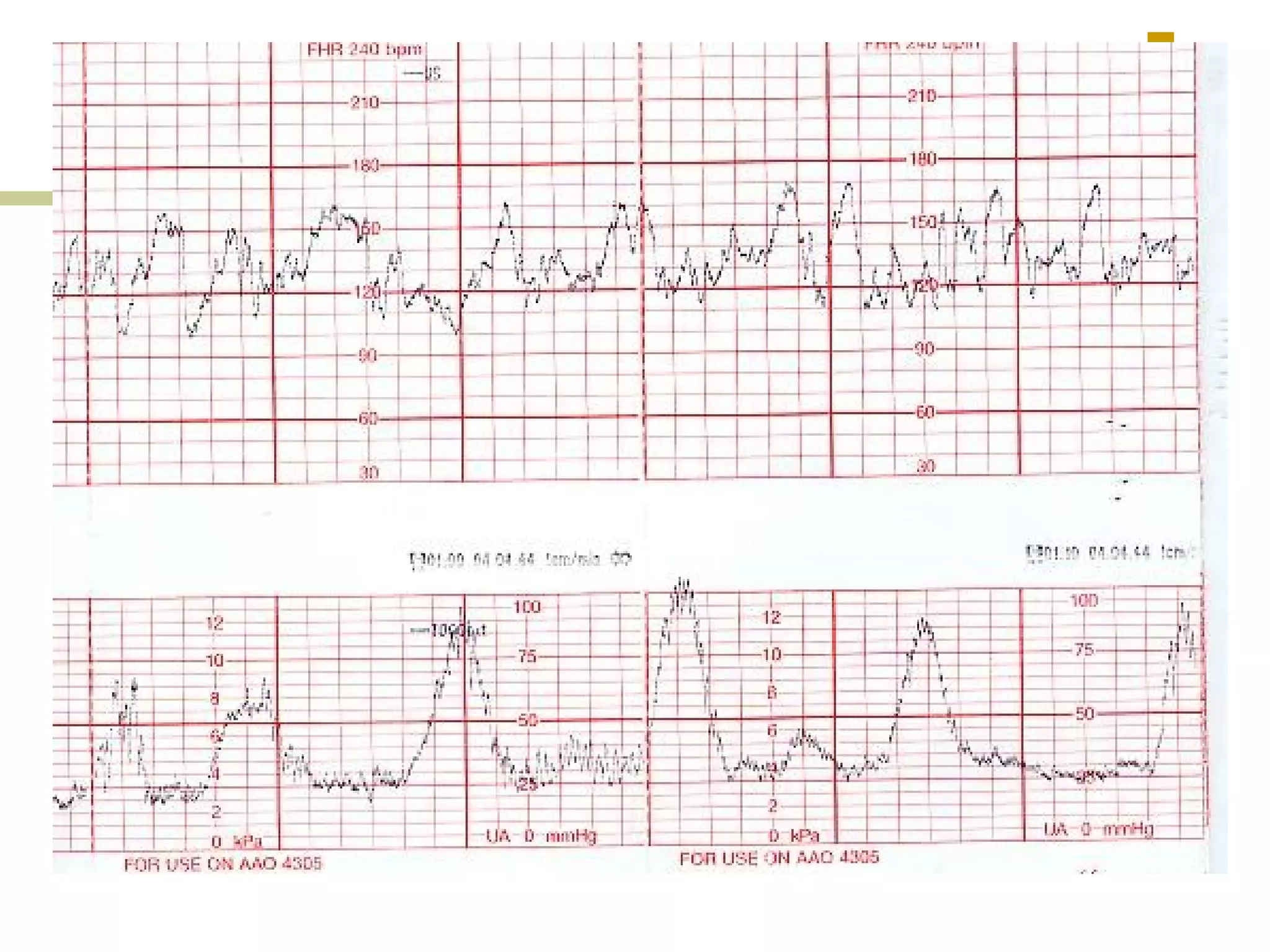
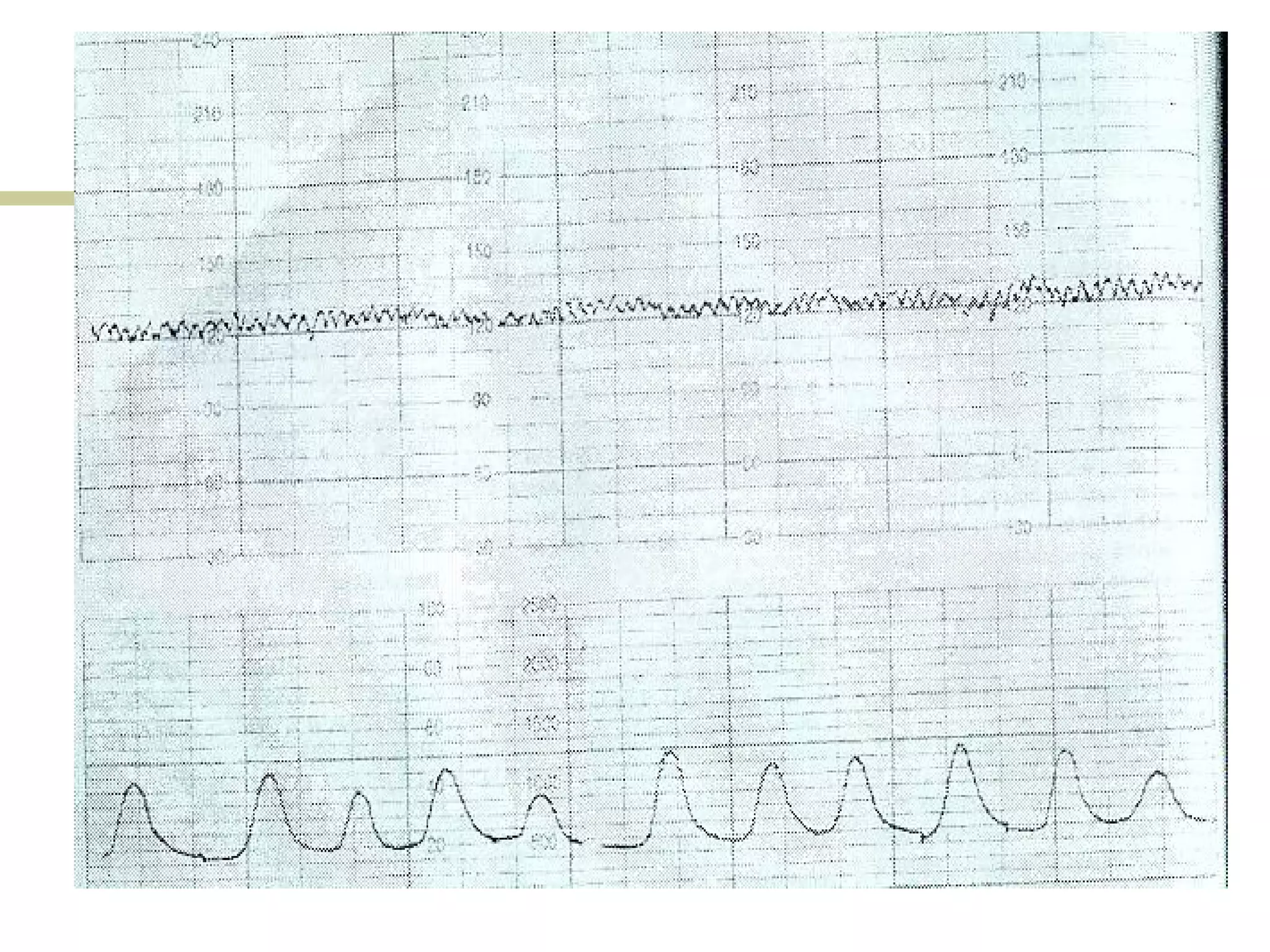
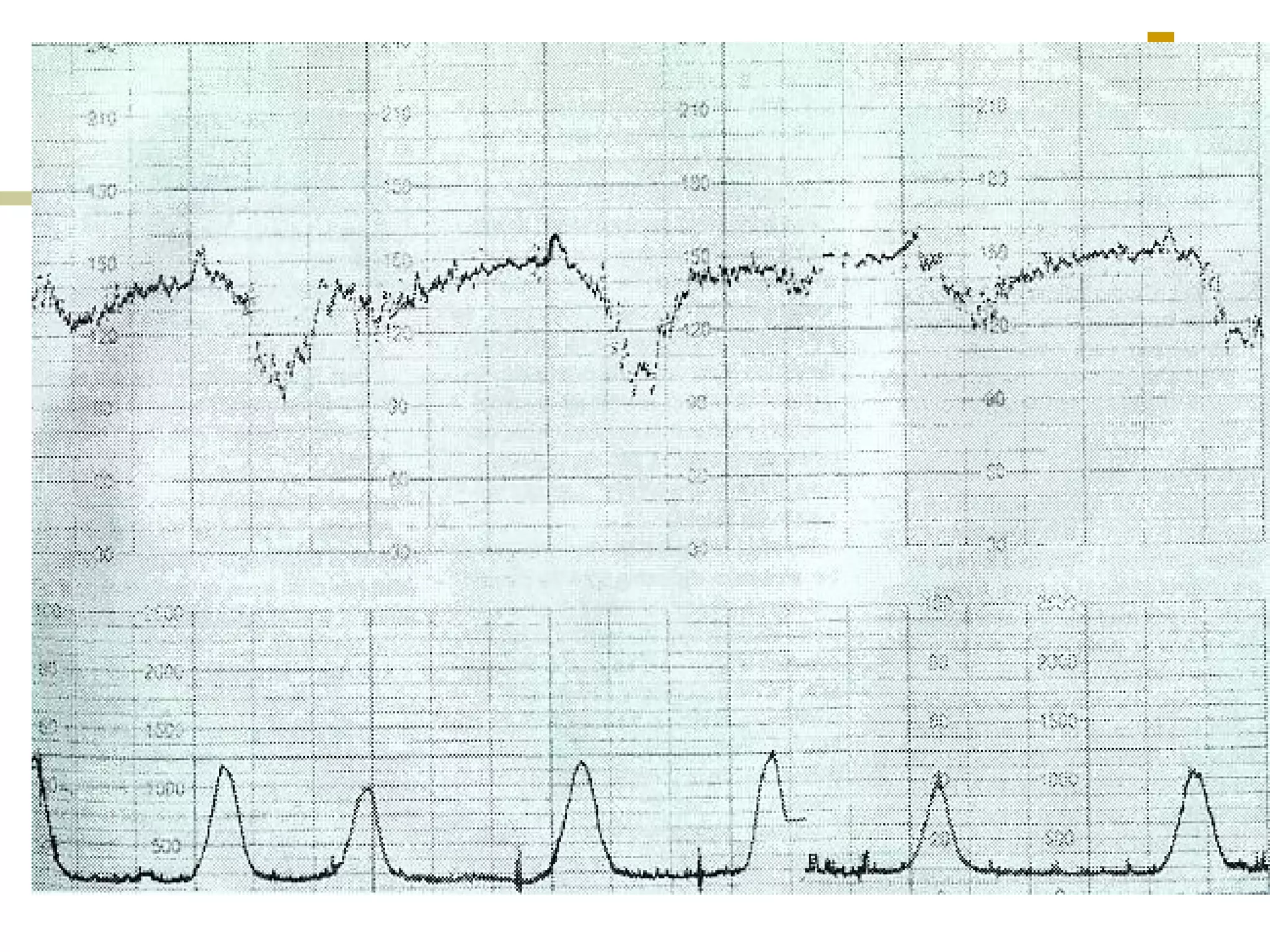
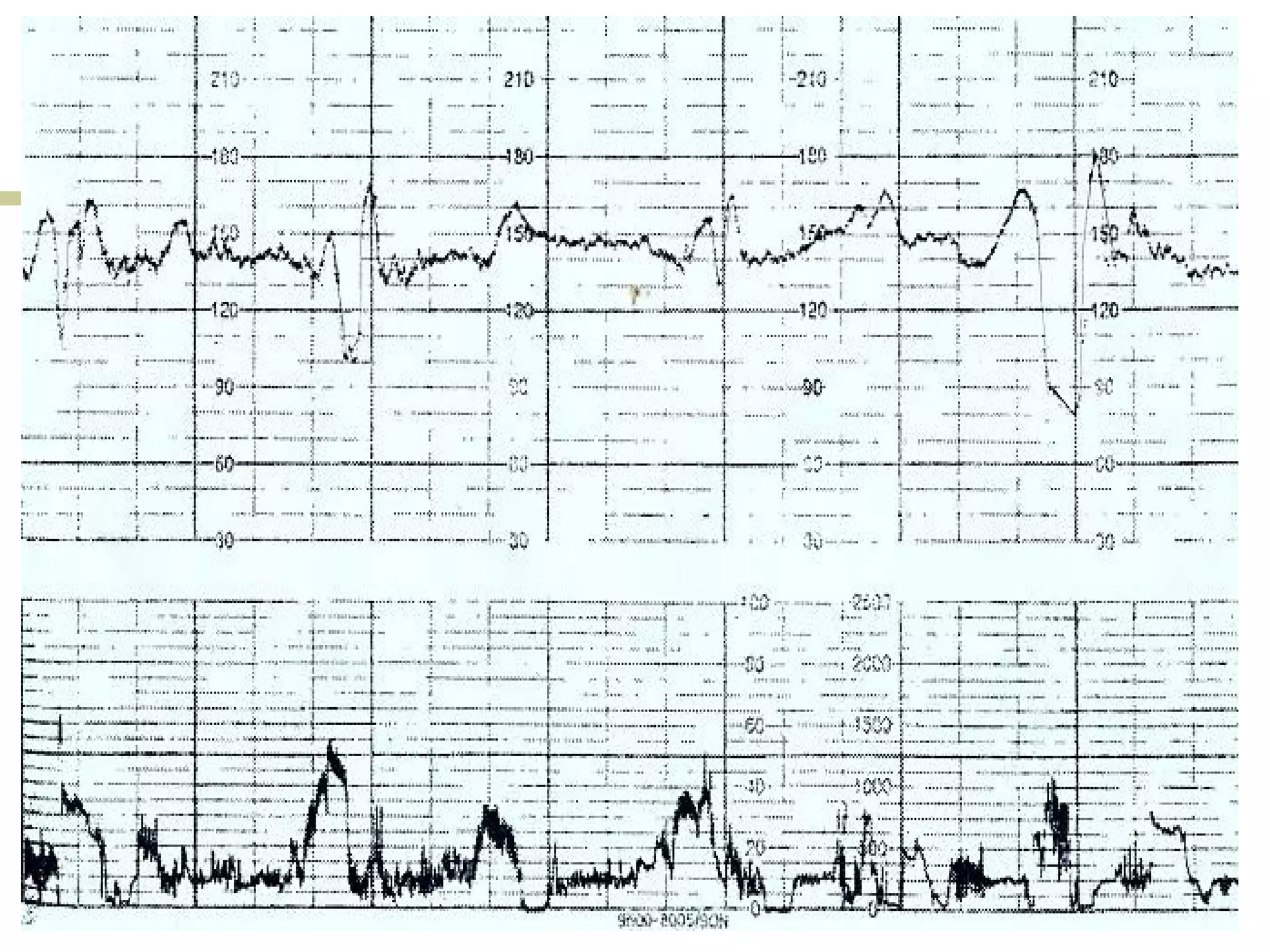
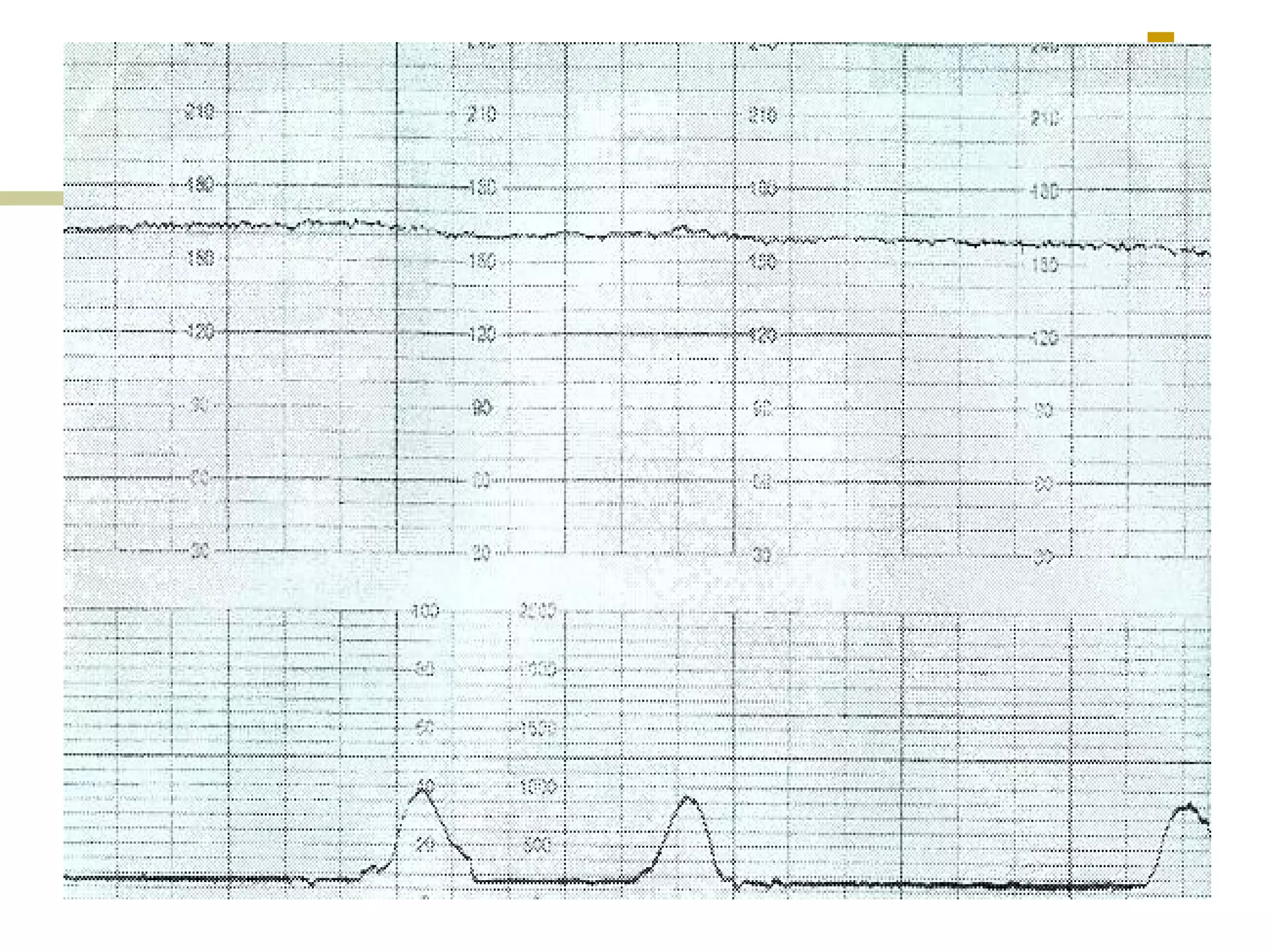
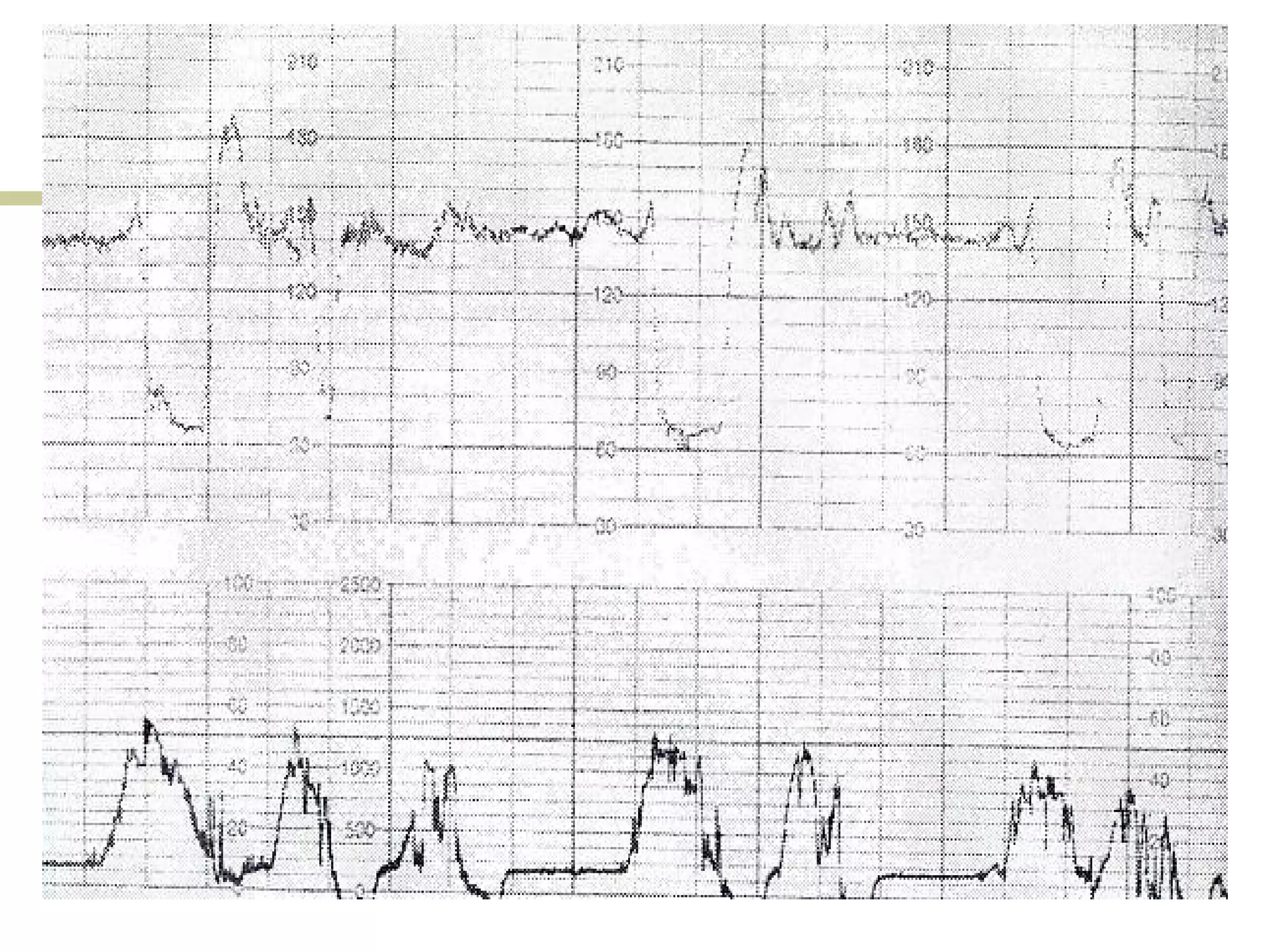
- Baseline heart rate, acceleration, deceleration, variability
- Reactive, bradycardia, tachycardia traces
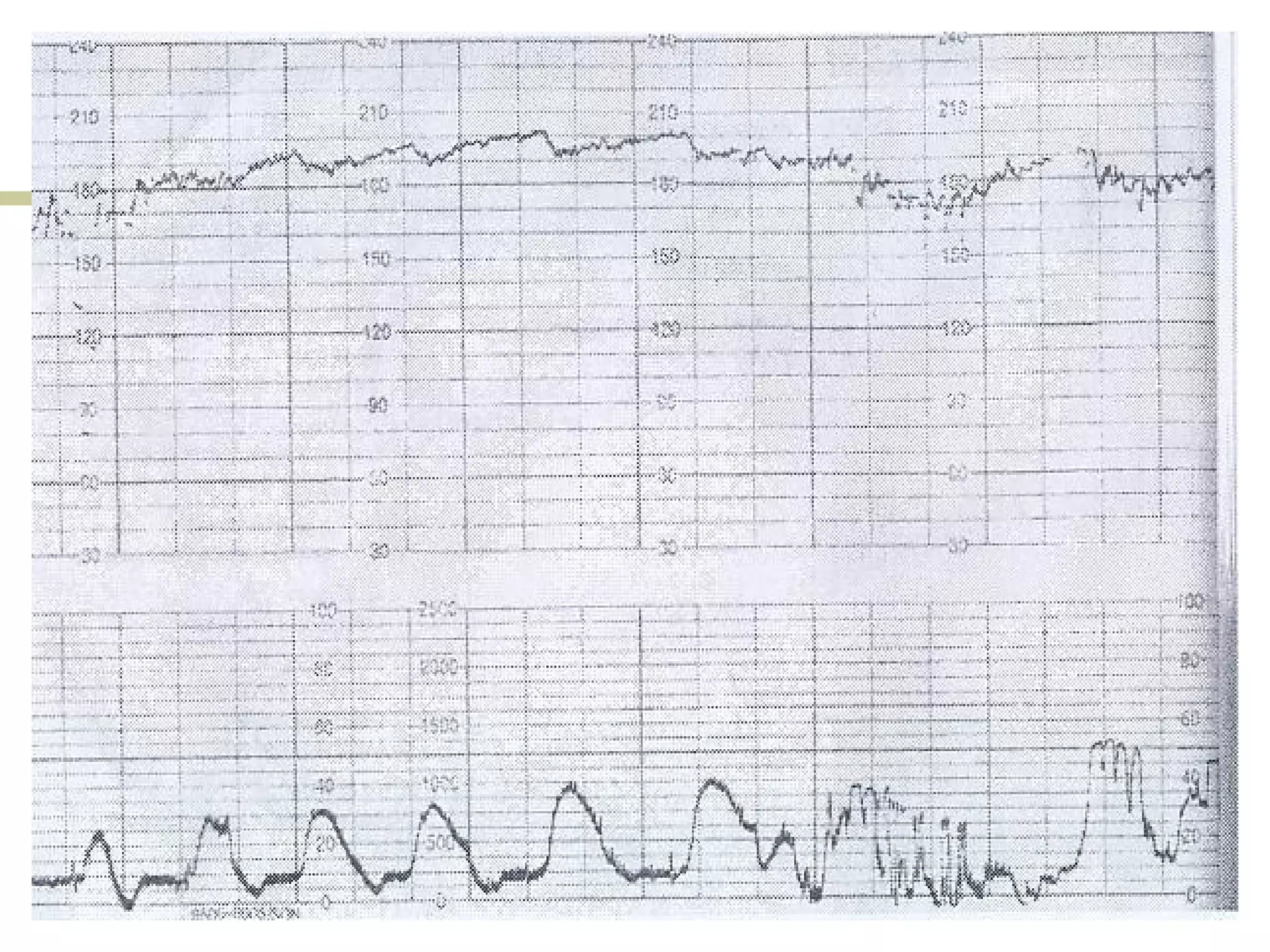
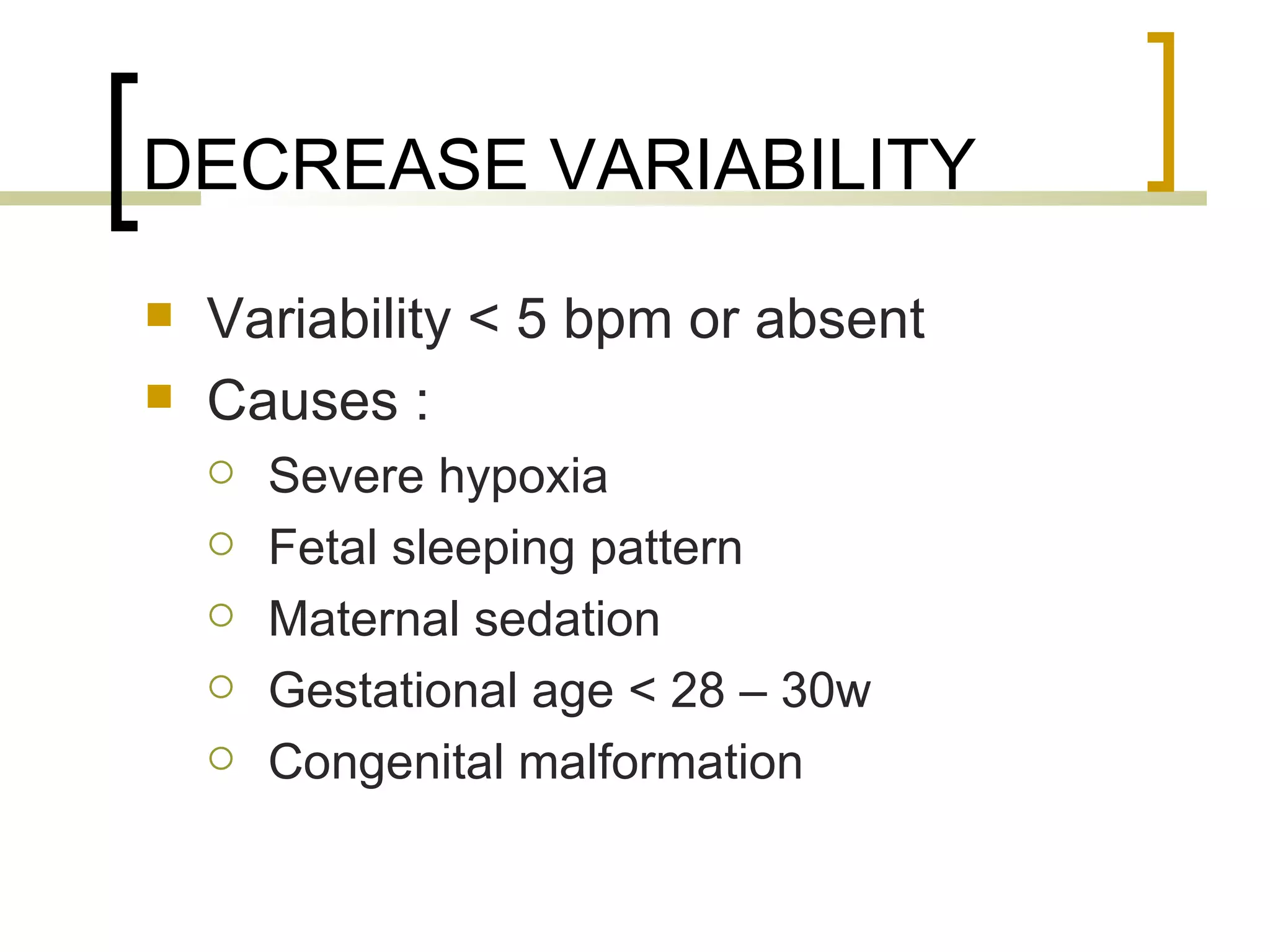
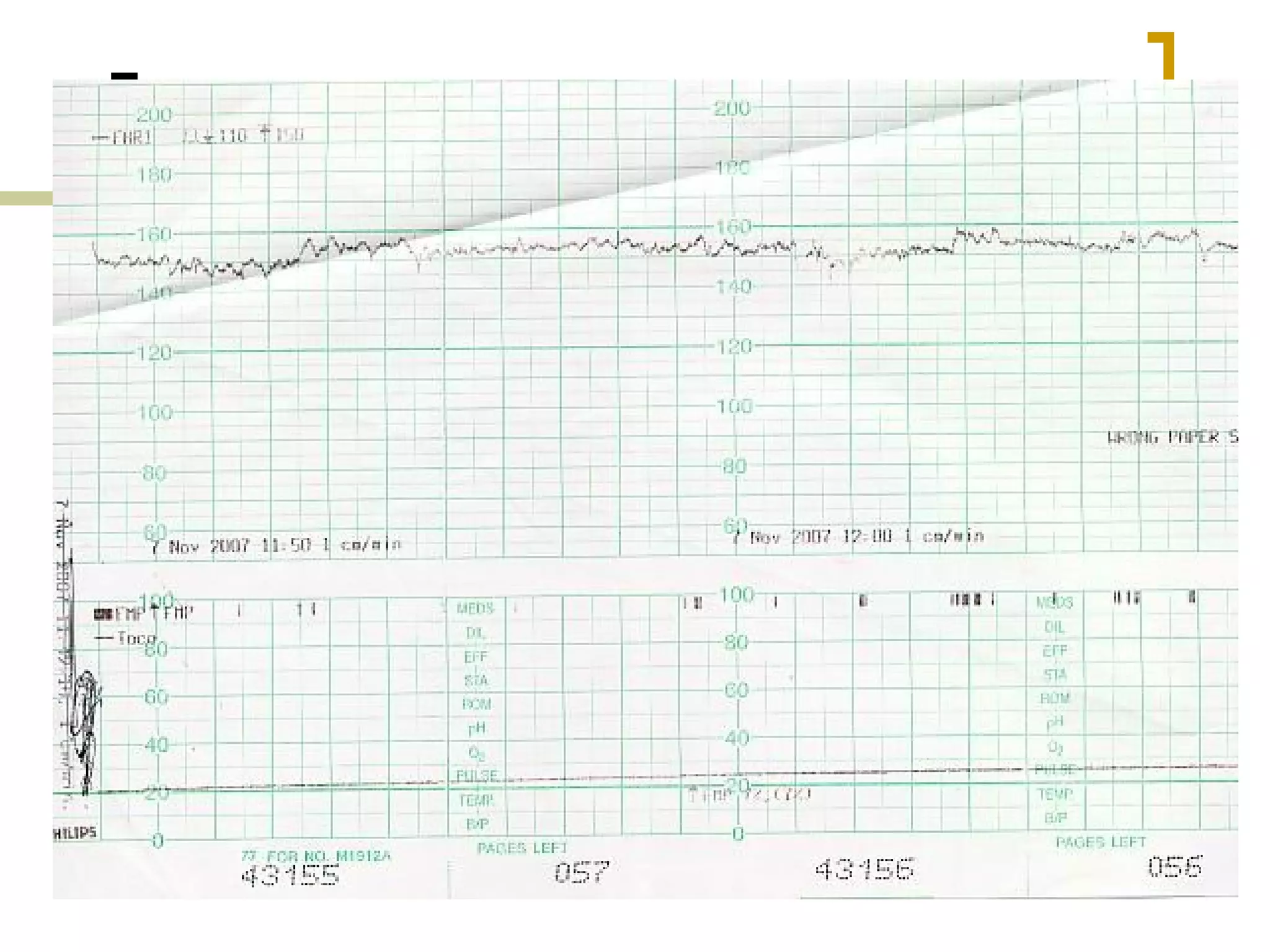
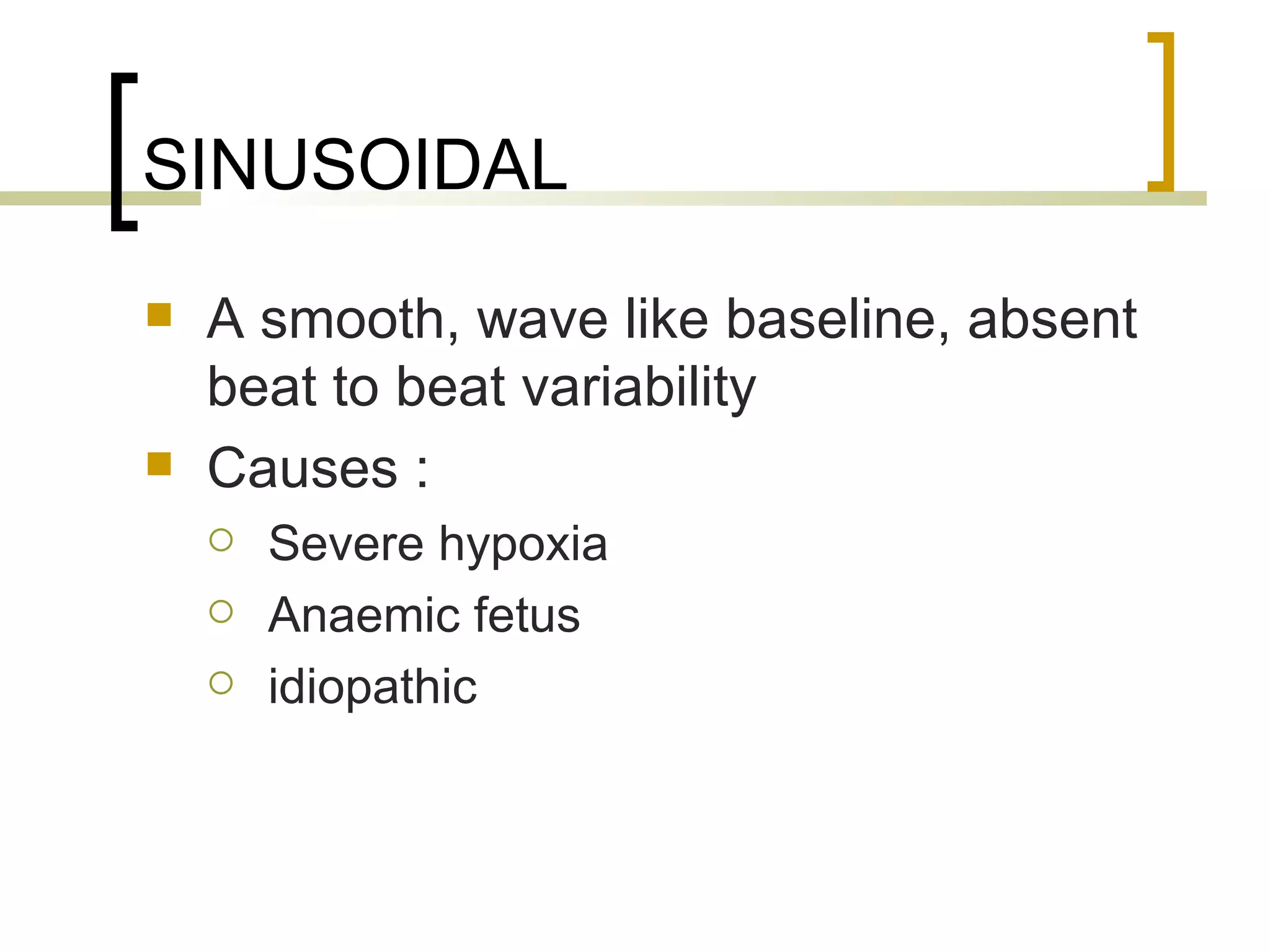
- Decreased variability, sinusoidal patterns
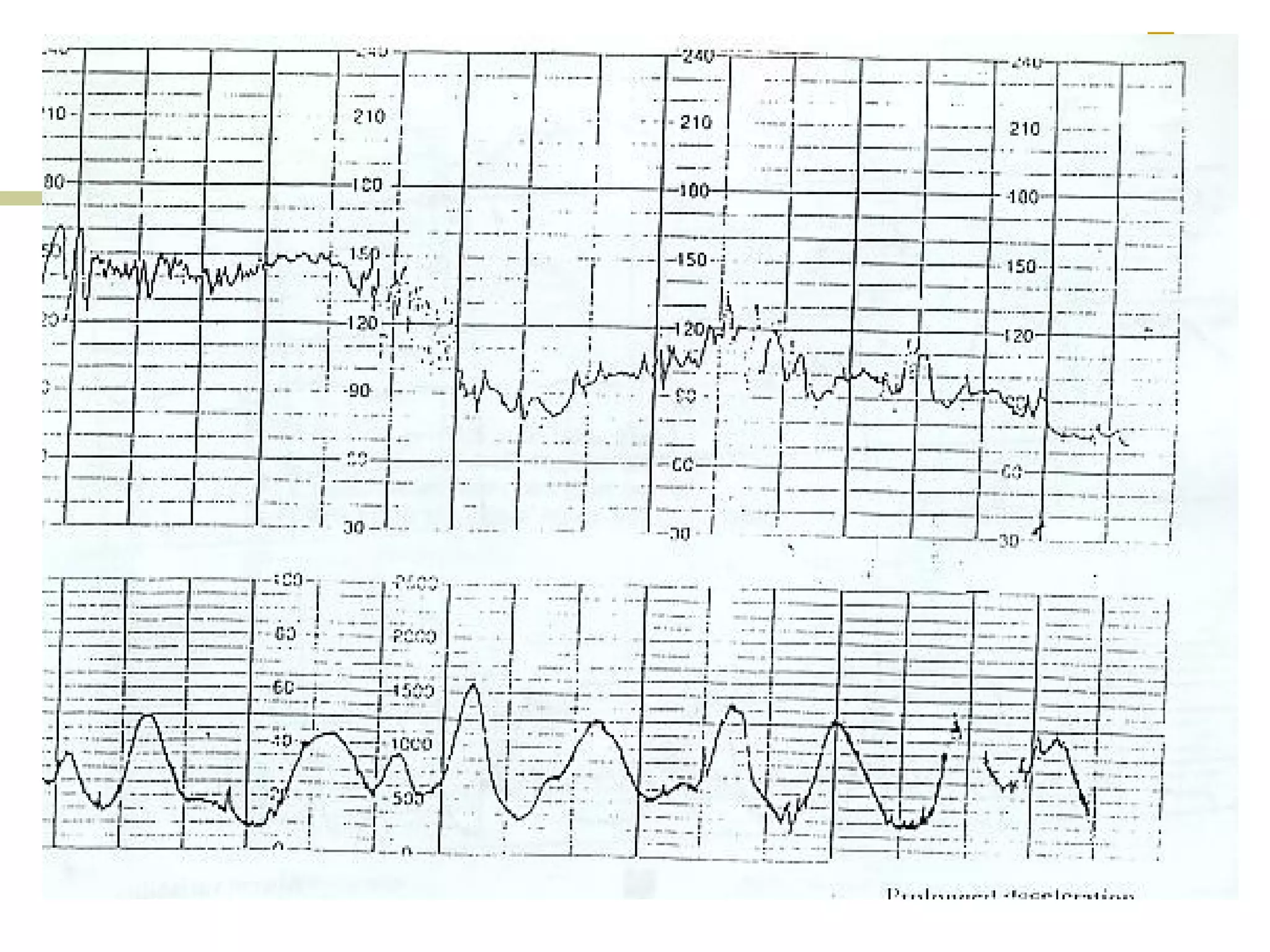
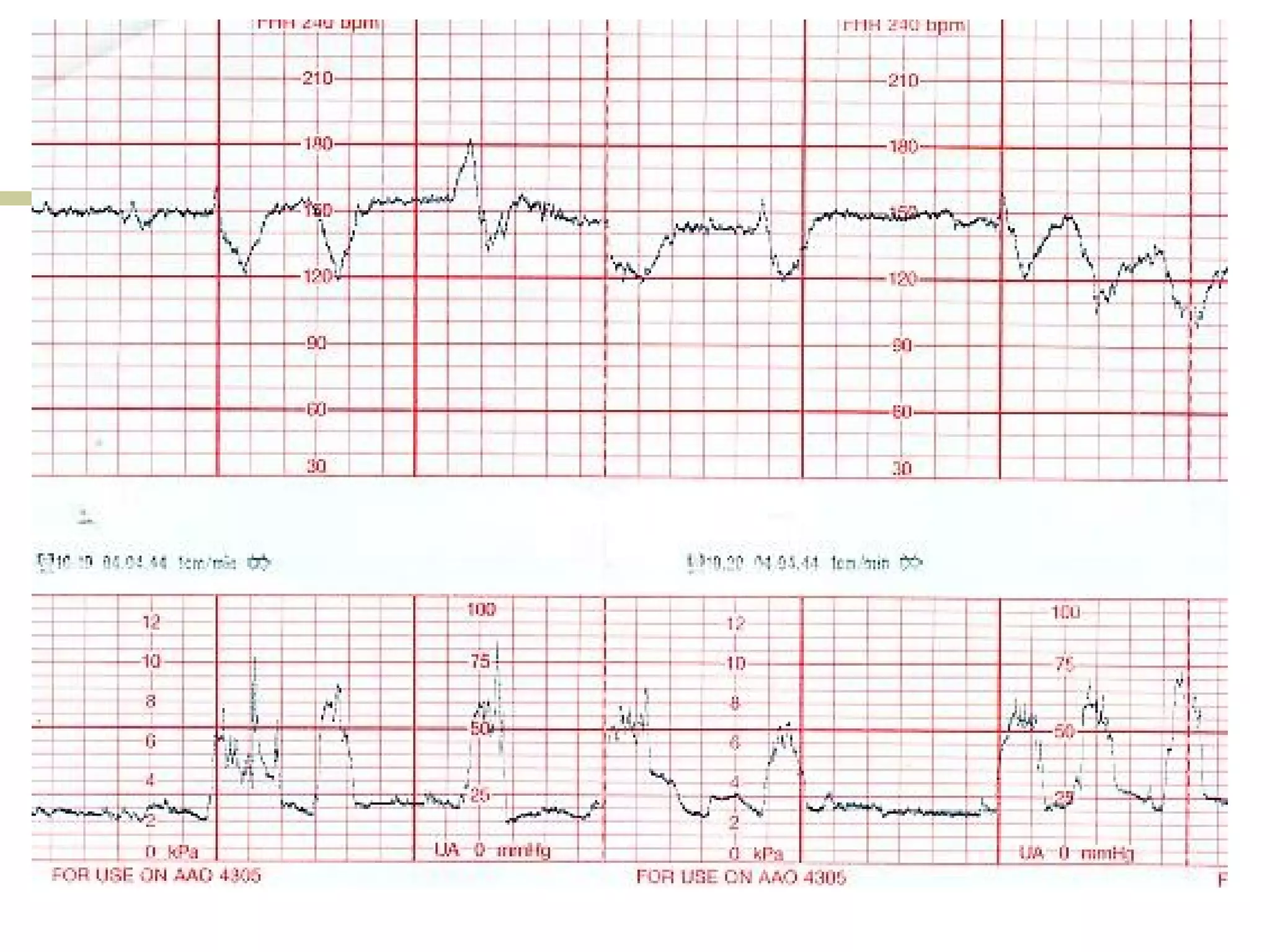
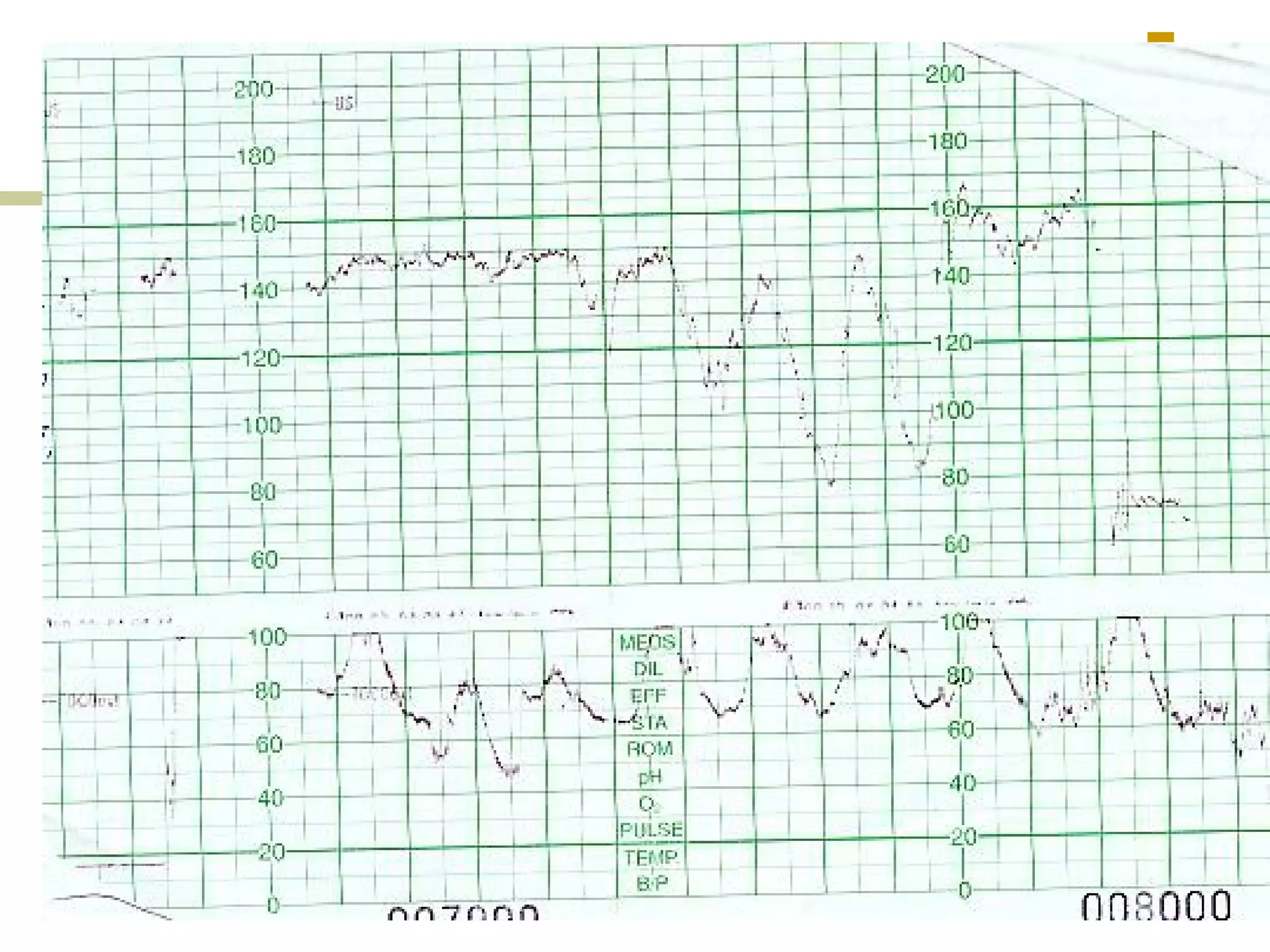
- Early, late, variable decelerations
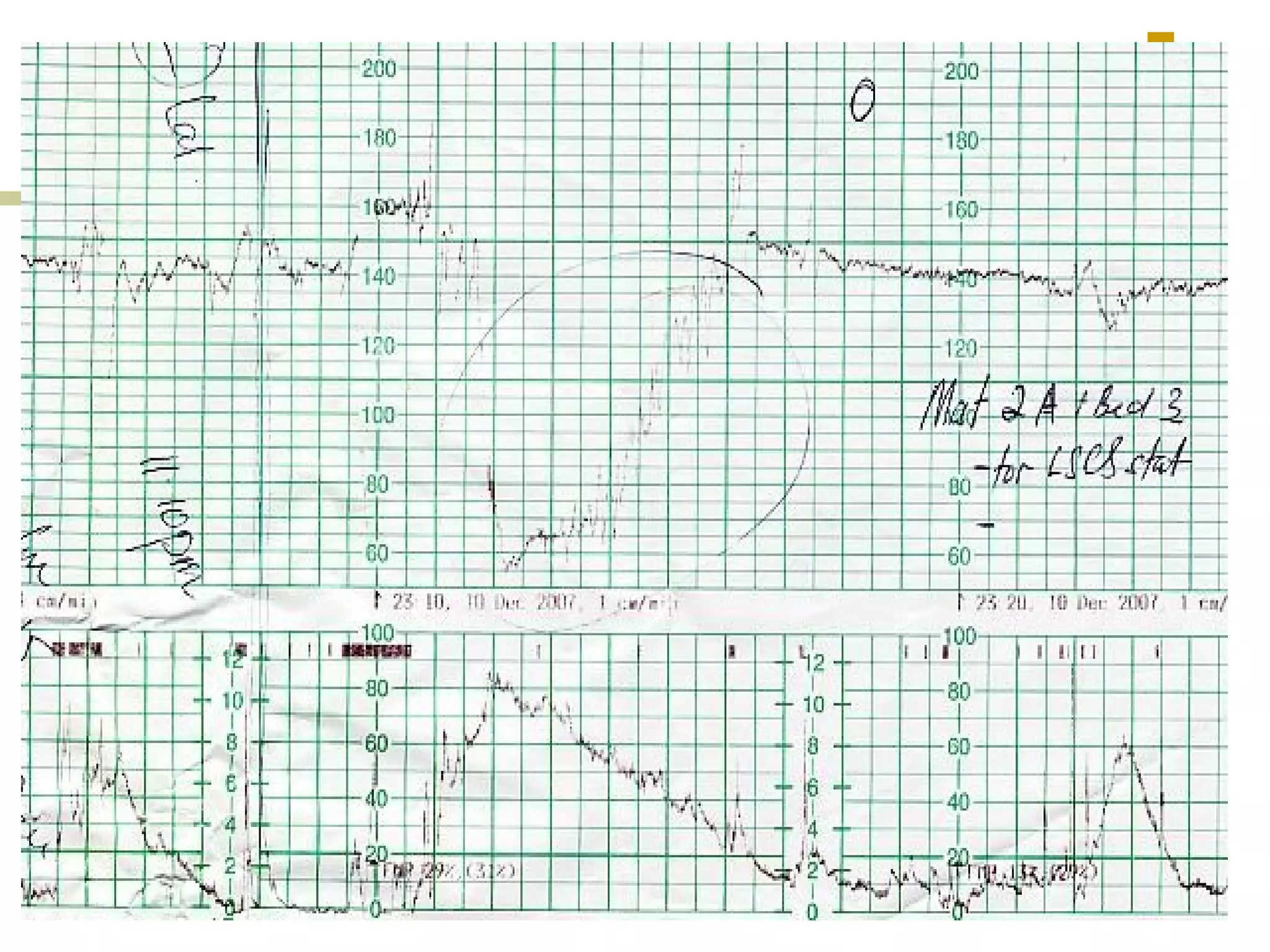
- Prolonged deceleration
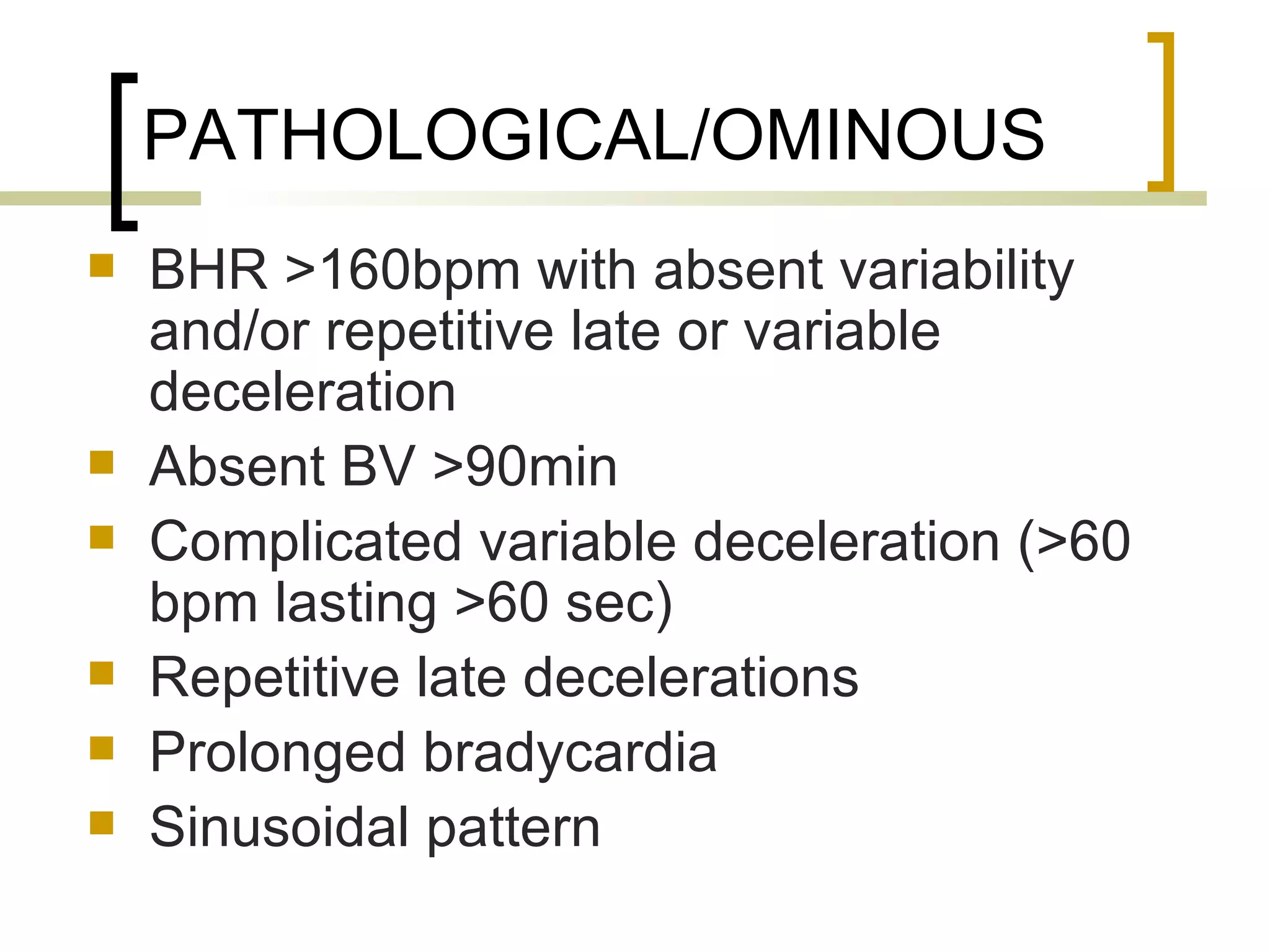
- Suspicious/equivocal and pathological/ominous CTG traces
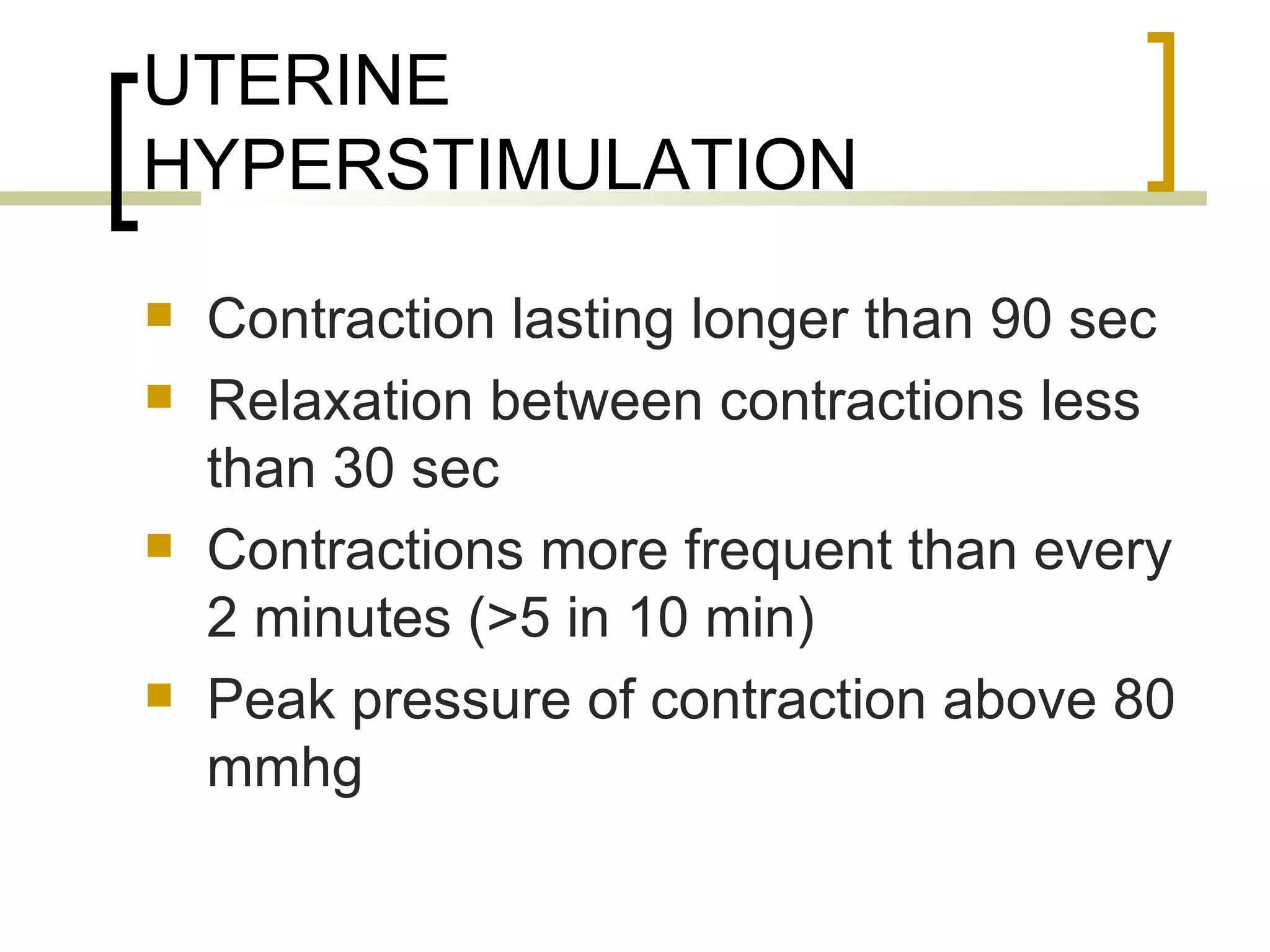
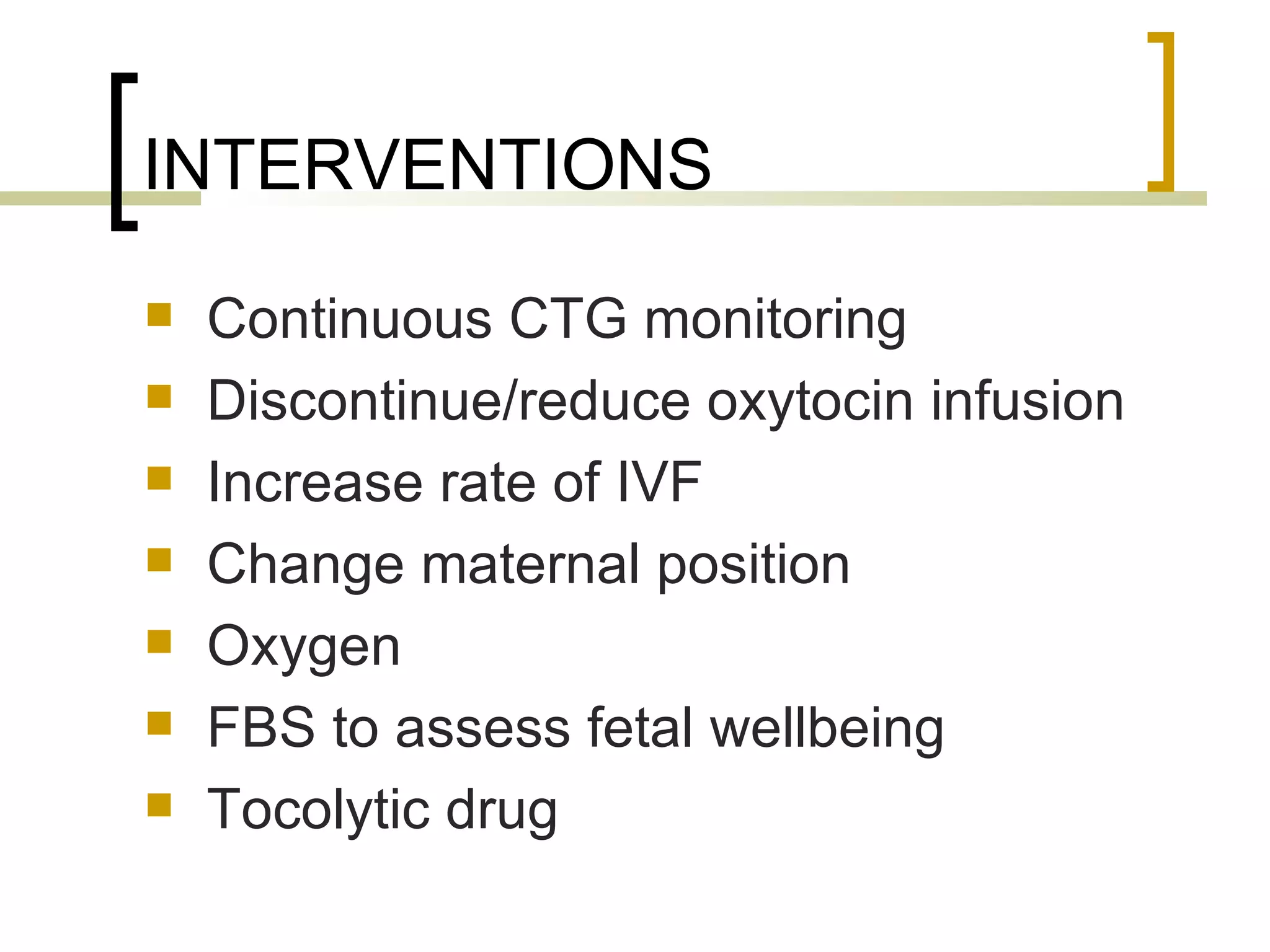
Clinical scenarios are presented involving pregnant women in labor with varying cervical dilation and fetal heart rate patterns on CTG monitoring. Uterine hyperstimulation is also defined.