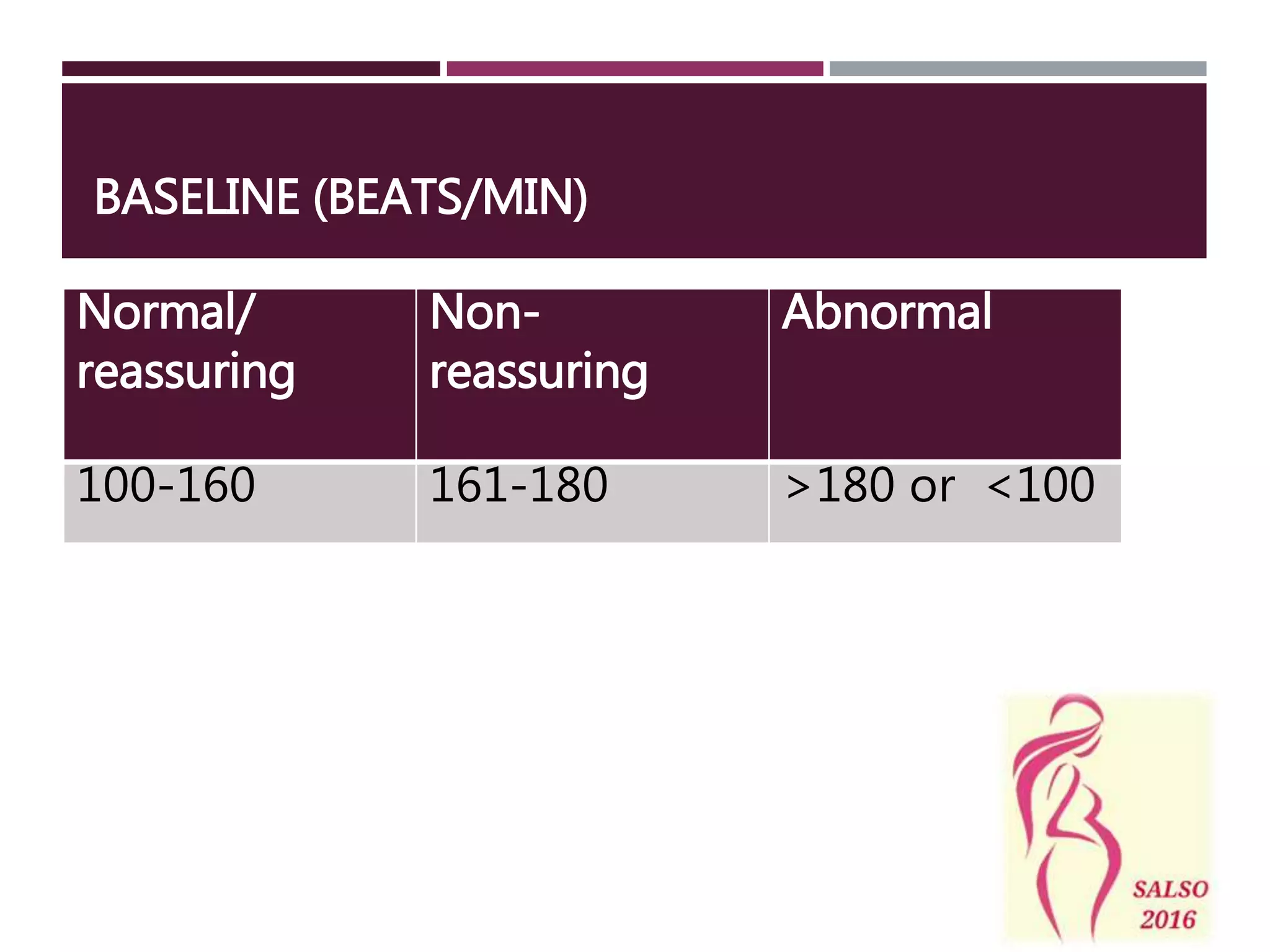
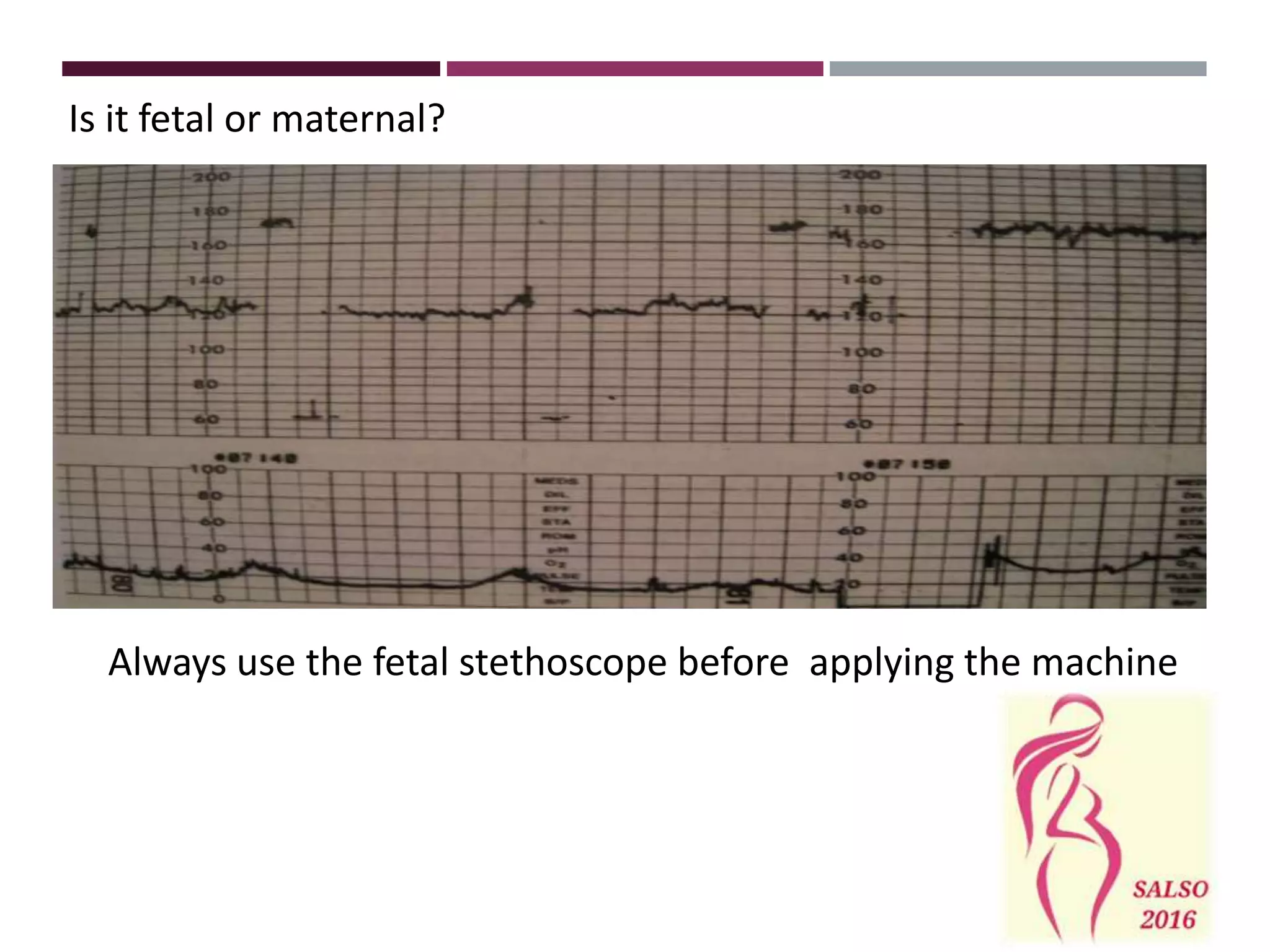
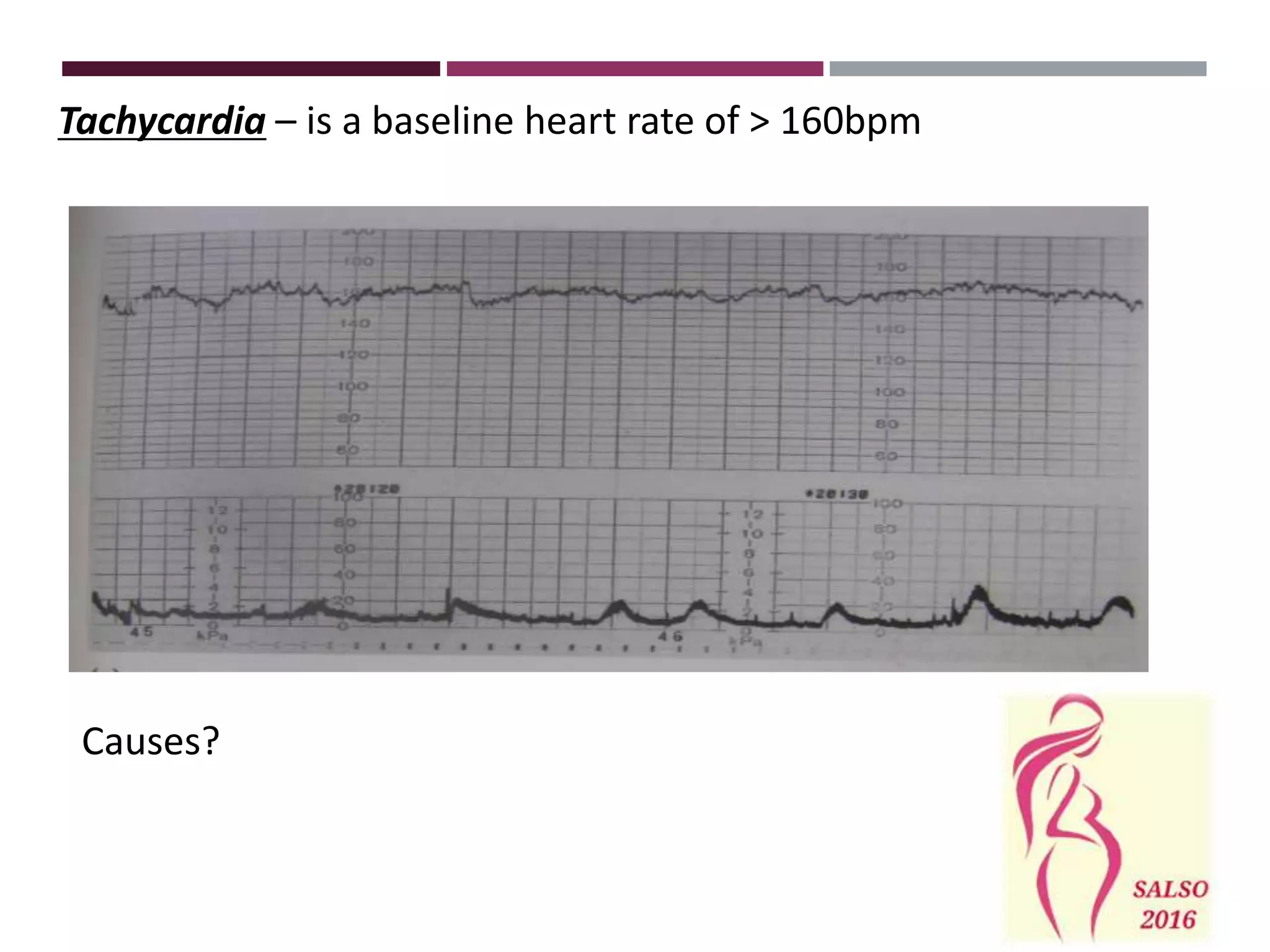
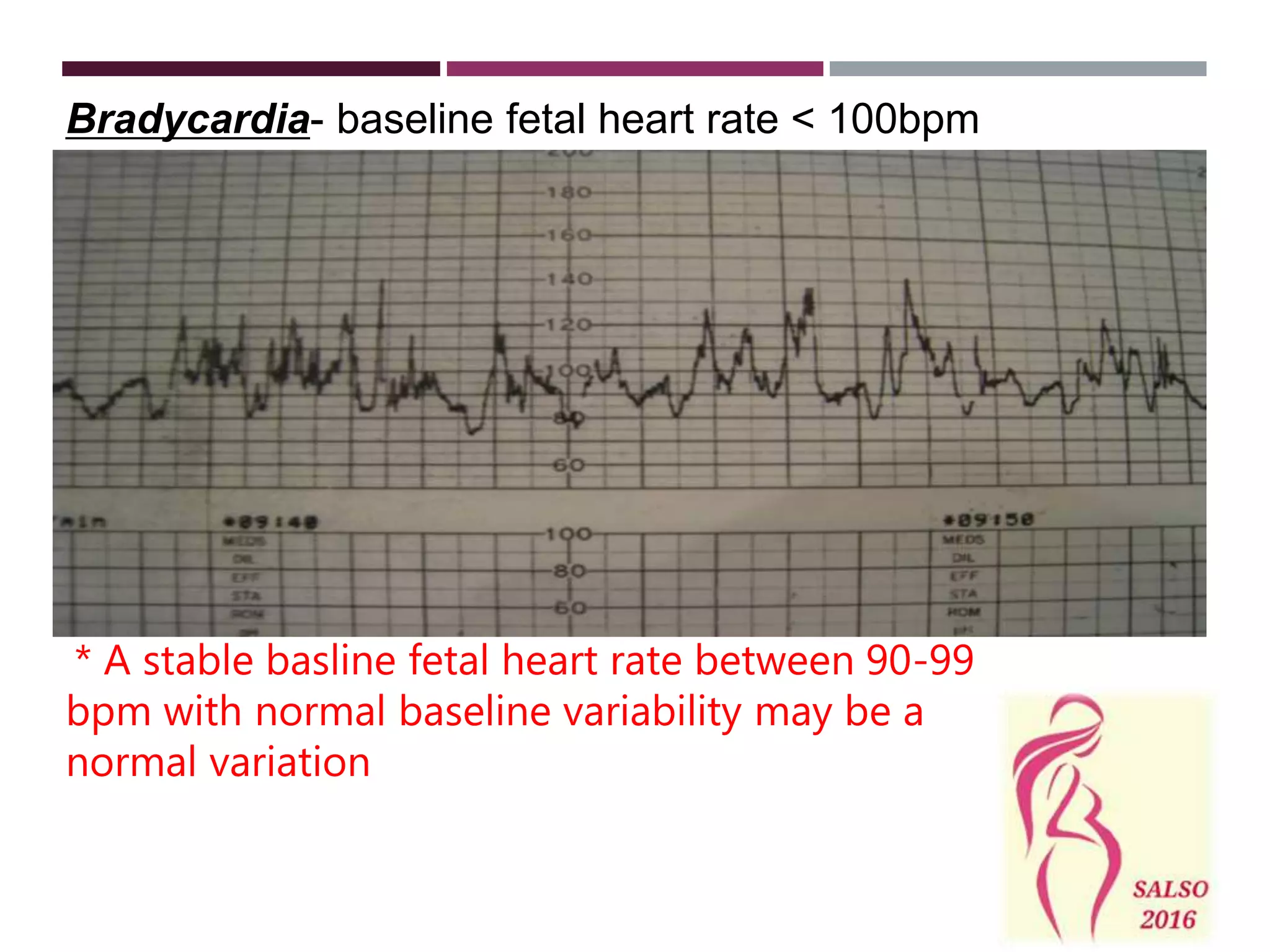
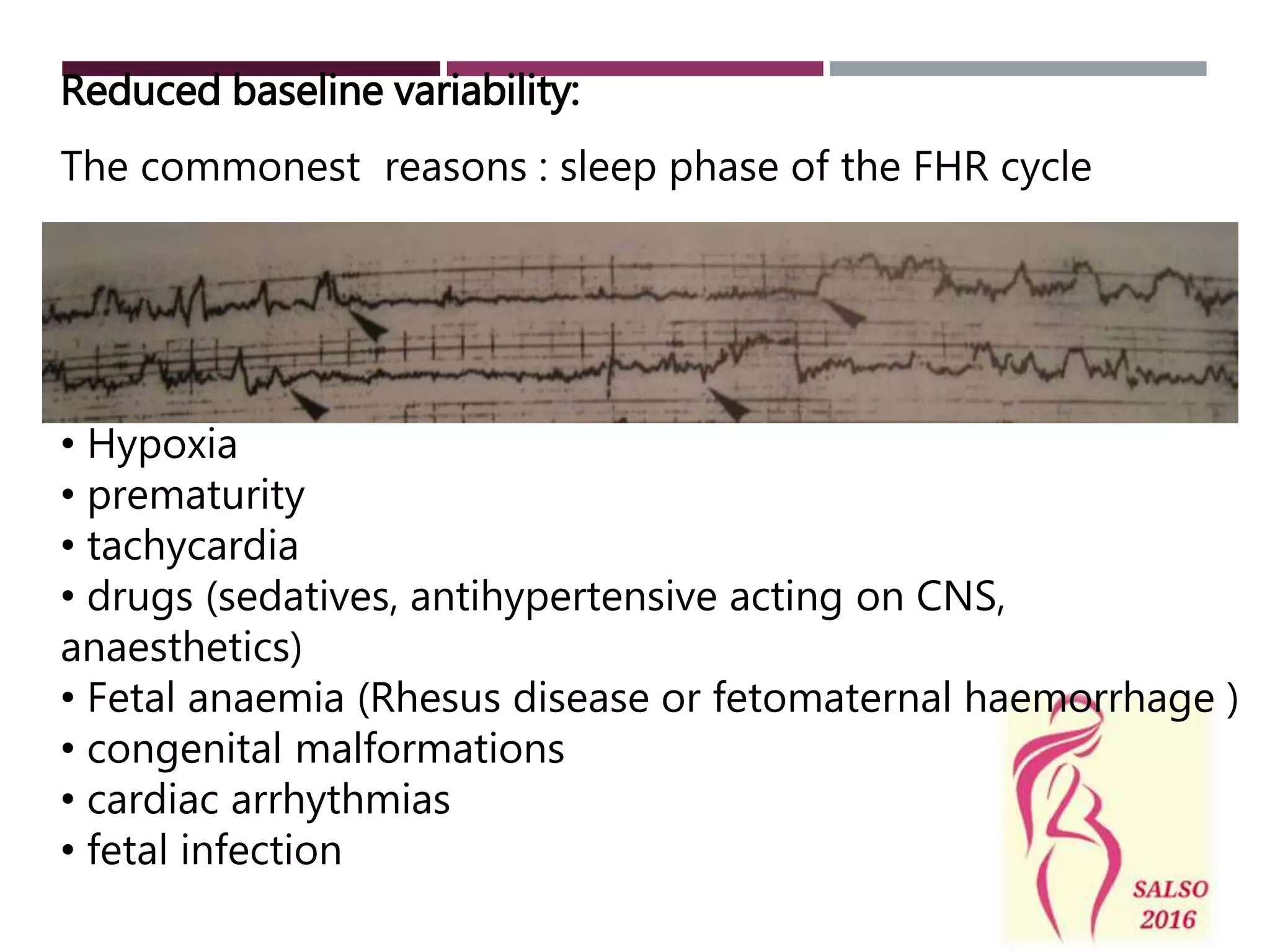
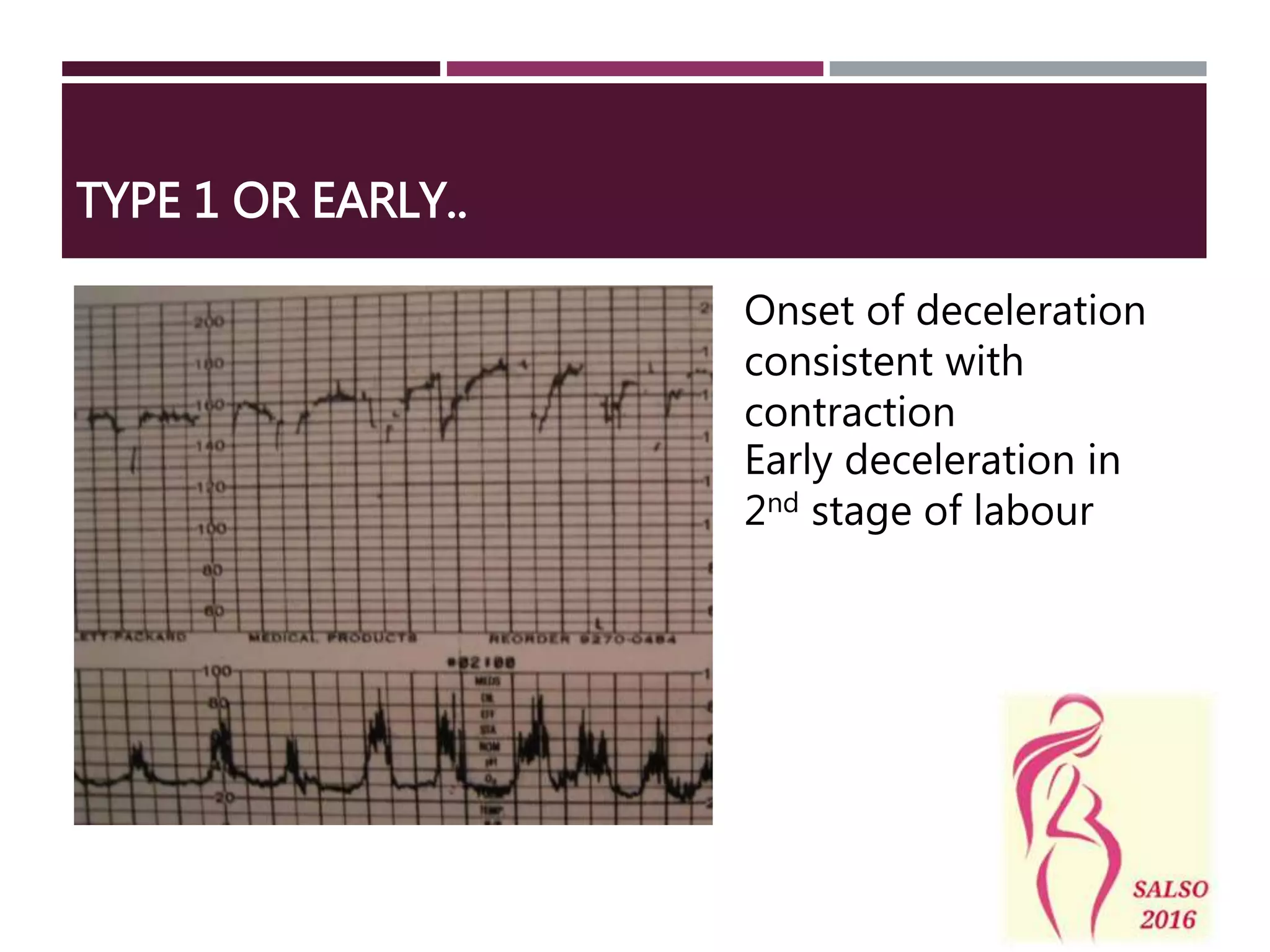
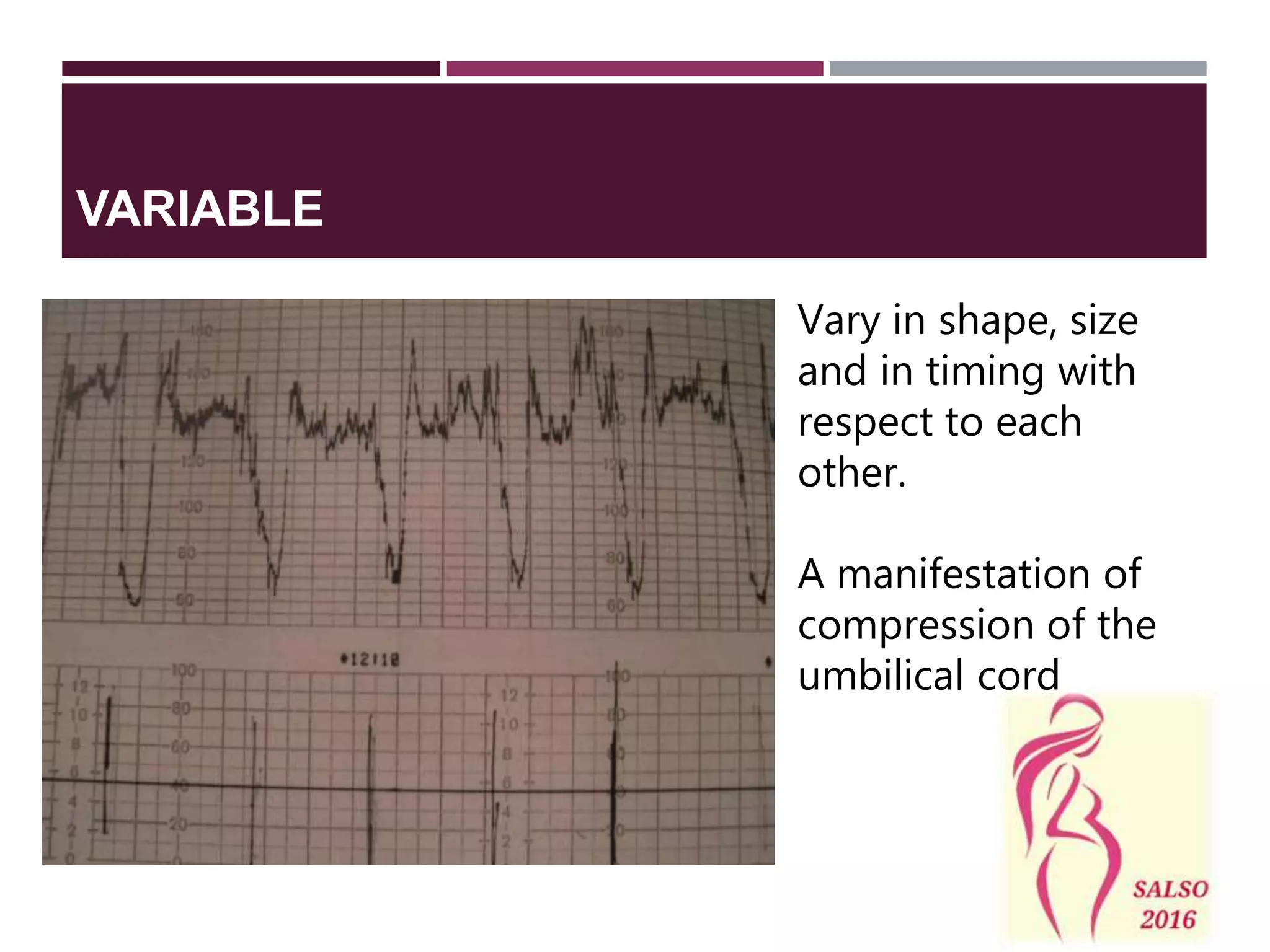
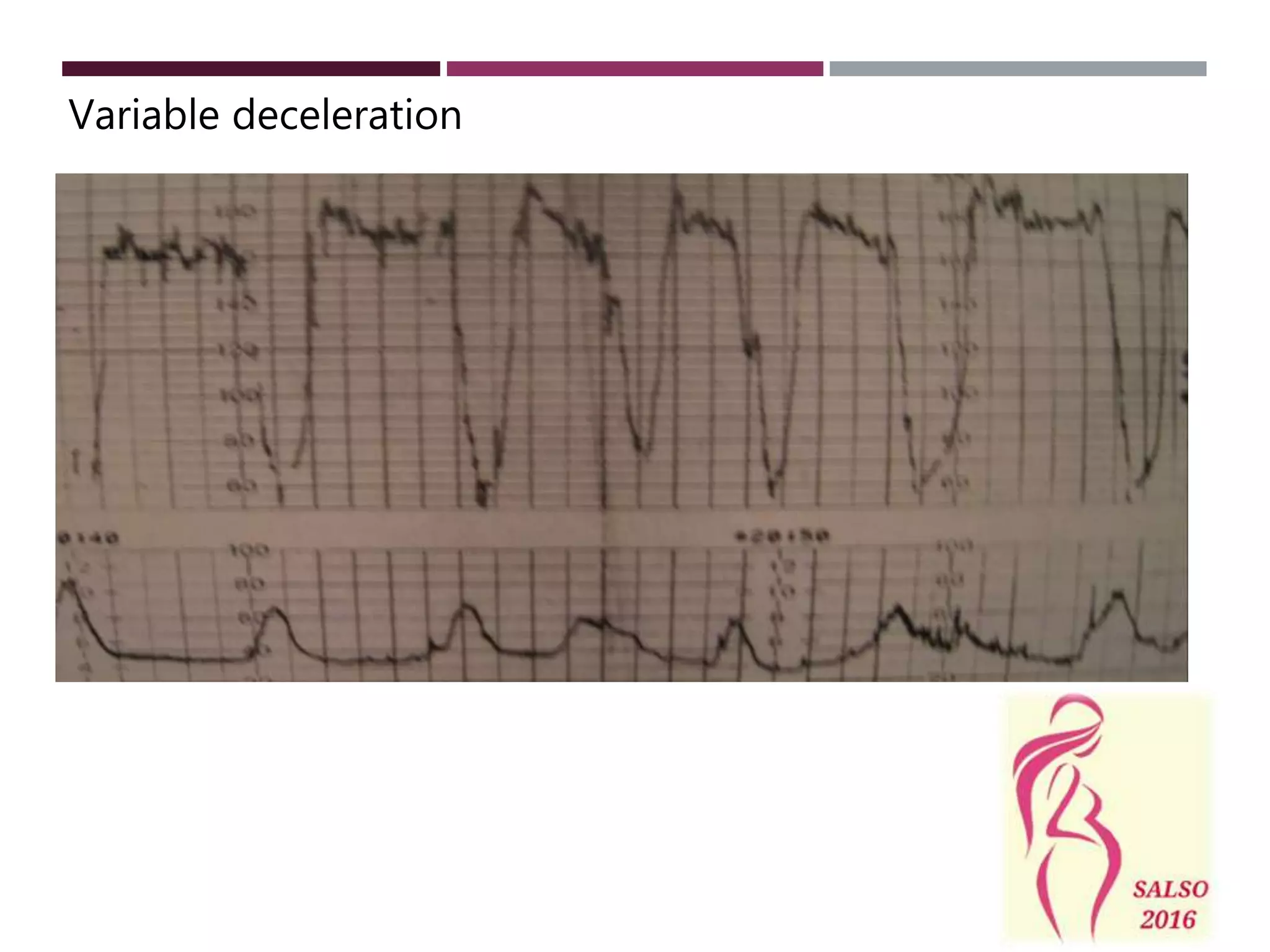
This document discusses fetal monitoring techniques used at SGH including intermittent auscultation, electronic fetal monitoring, and cardiotocography. It describes the goals of fetal monitoring and provides details on the different monitoring modalities, terminology used in CTG interpretation, guidelines for monitoring based on risk level, and management of abnormal tracings. Fetal scalp blood sampling is also discussed as a technique to determine fetal acid-base status when CTG changes are non-reassuring.