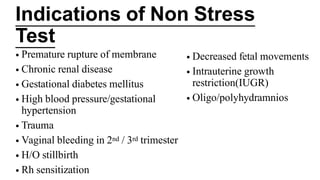
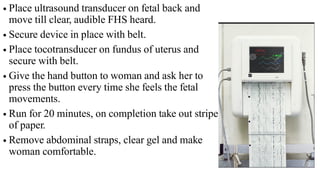
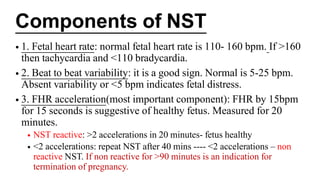
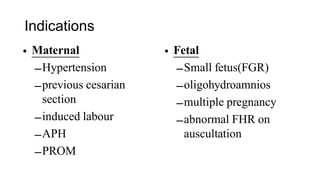
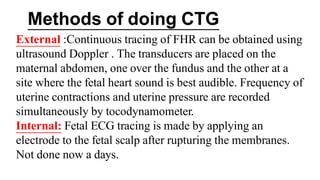
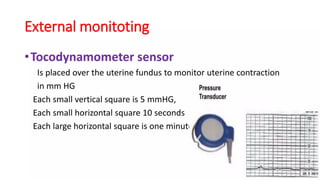
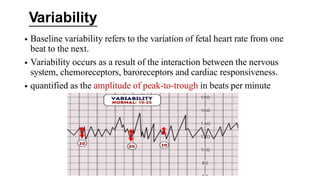
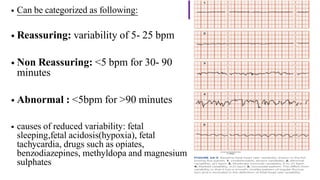
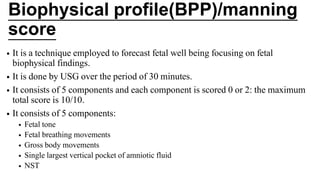
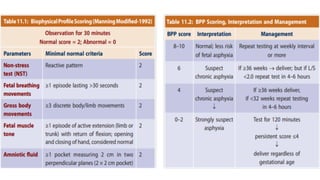
The document provides an overview of non-stress tests (NST) and biophysical profiles as methods for antepartum fetal monitoring, assessing fetal well-being through heart rate and movements. It outlines procedures, indications, components, and interpretations of NSTs and cardiotocography (CTG), including their significance in identifying potential fetal distress. Additionally, it explains the biophysical profile (BPP) and modified biophysical profile (MBPP) as tools for evaluating fetal health, focusing on various components assessed during the tests.