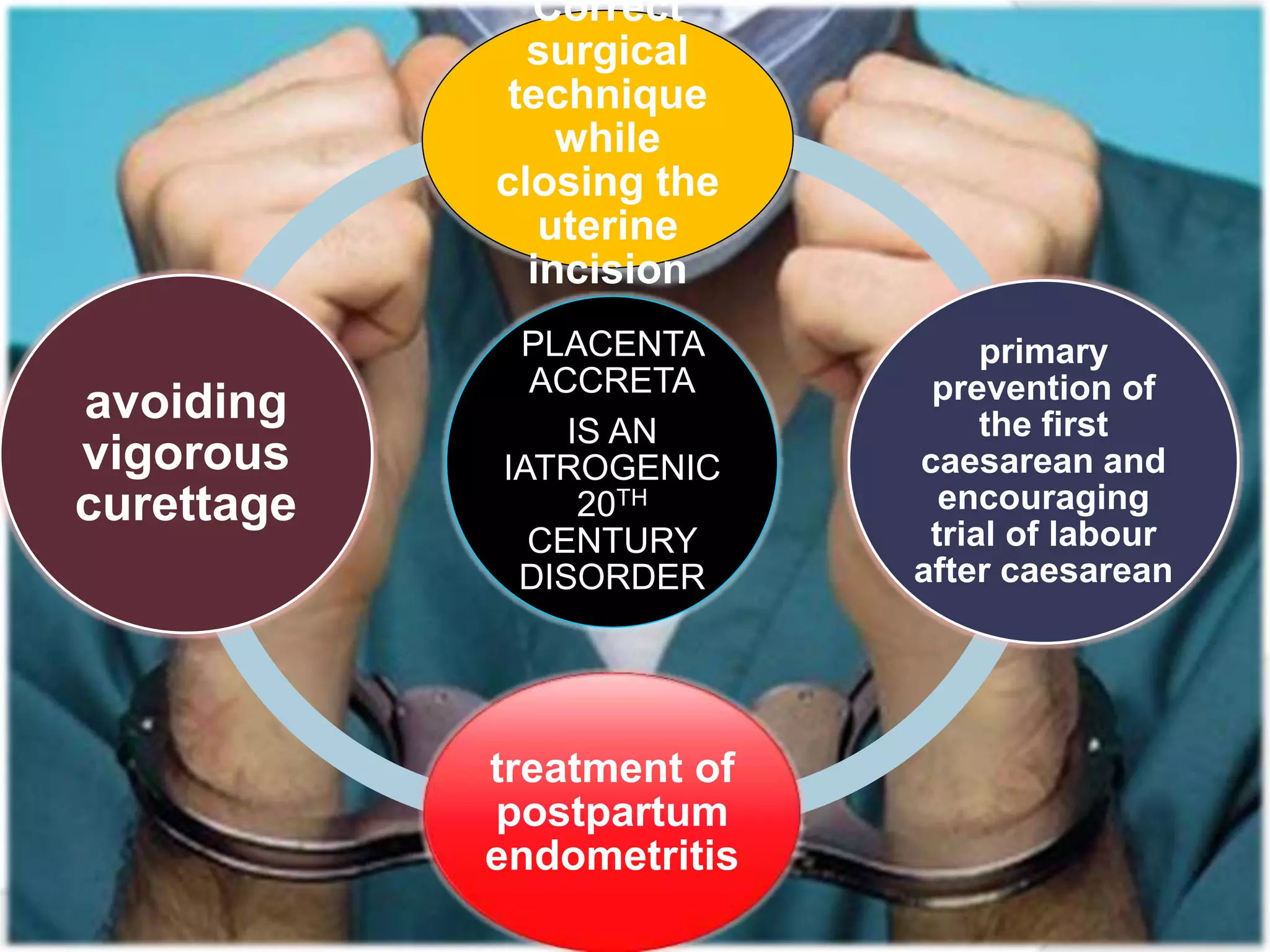
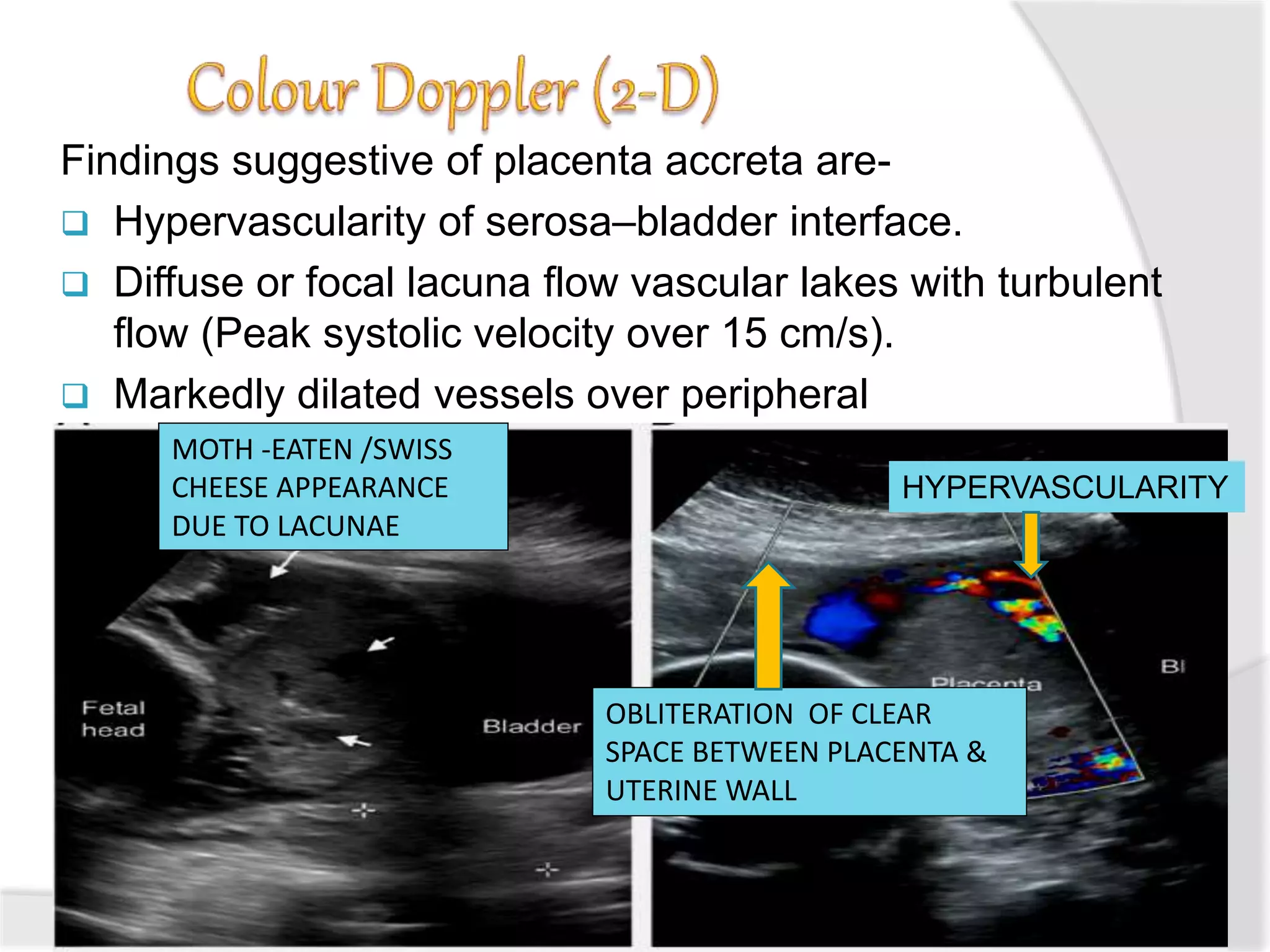
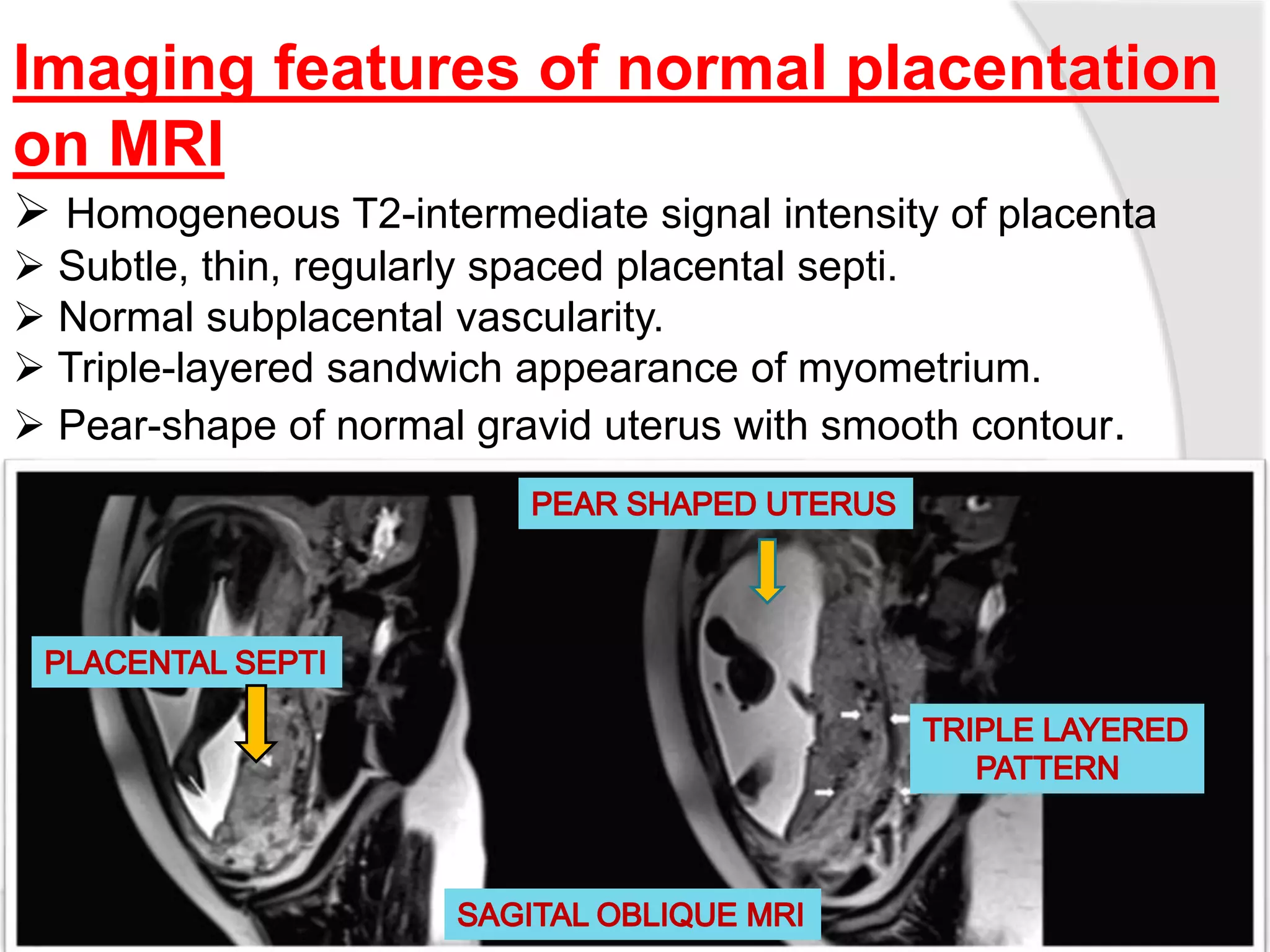
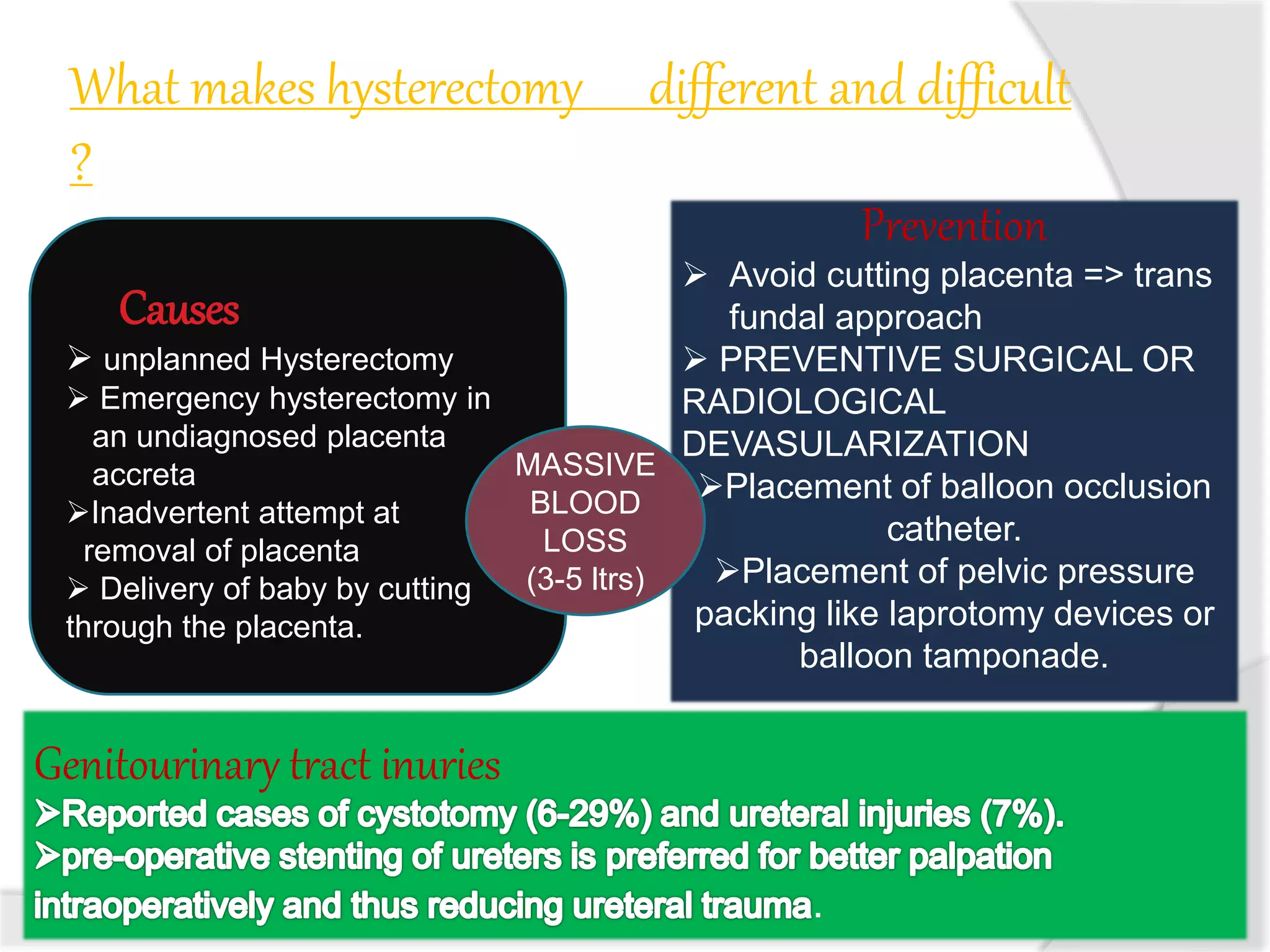
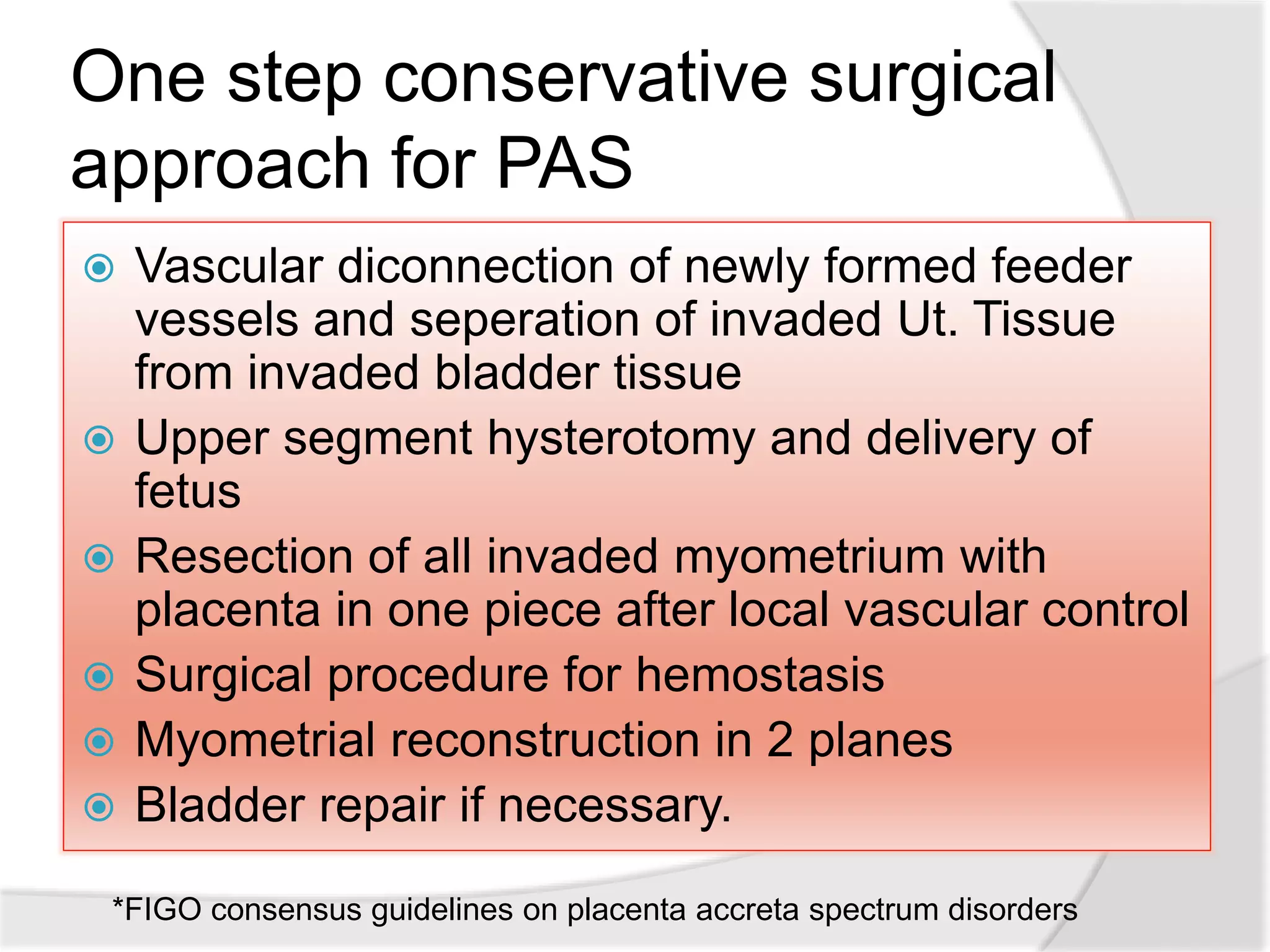
This document discusses placenta accreta syndrome, including risk factors, diagnostic methods, and management strategies. It begins with an overview of placenta accreta classifications. Ultrasound and MRI are important diagnostic tools, with ultrasound being the primary method. Risk factors include prior c-sections, placenta previa, and uterine surgeries. Early diagnosis allows for elective c-section and interventions like arterial embolization to reduce bleeding. Hysterectomy is often needed to control hemorrhage but conservative approaches aim to preserve the uterus. Proper multidisciplinary care and prevention of delays in management can improve outcomes for this serious condition.