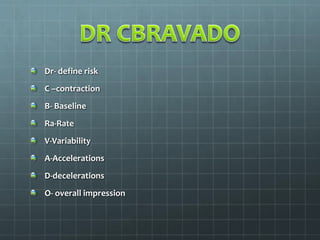
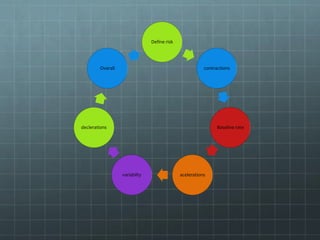
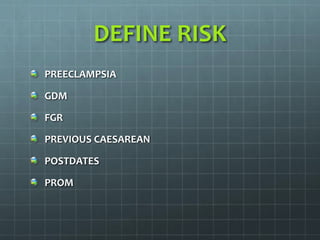
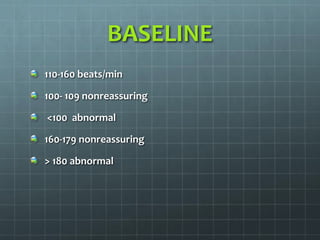
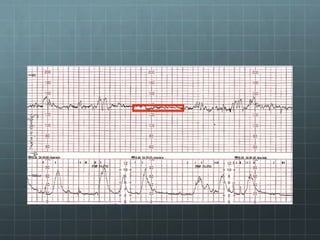
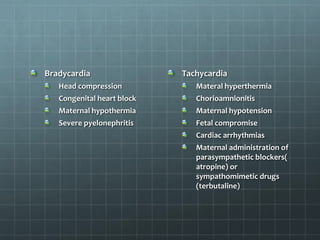
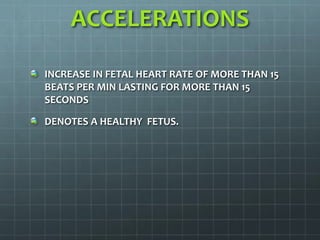
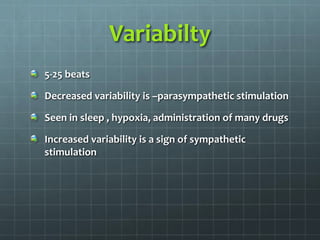
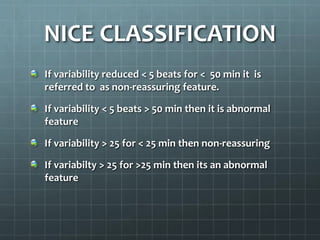
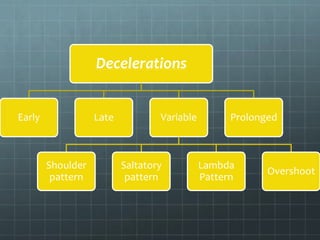
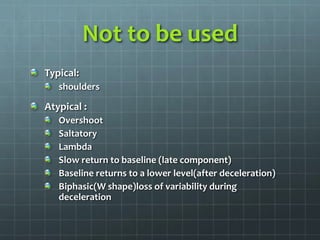
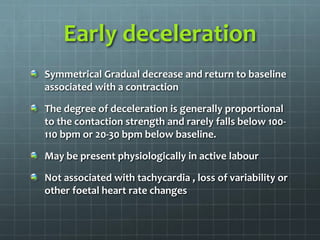
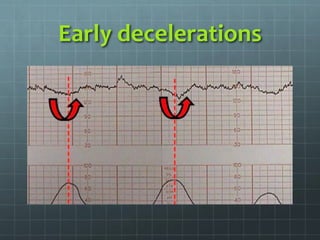
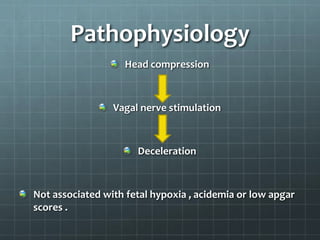
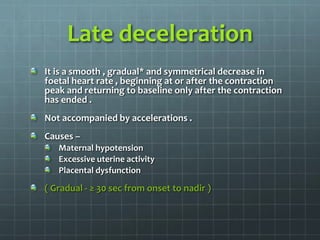
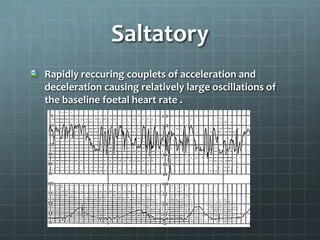
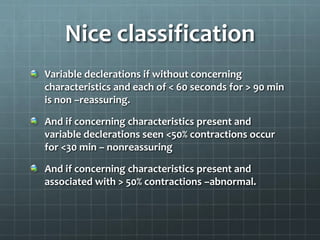
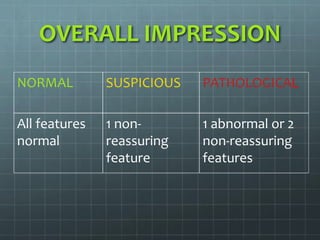
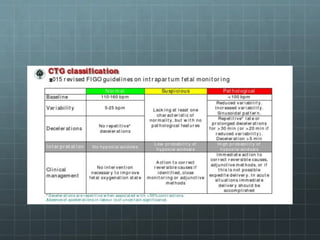
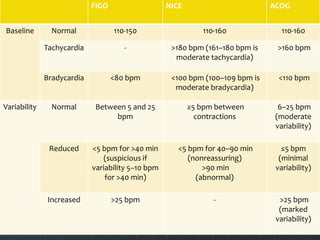
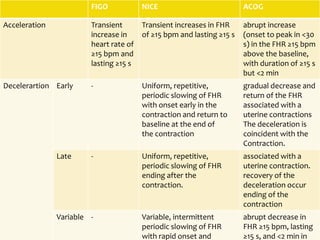
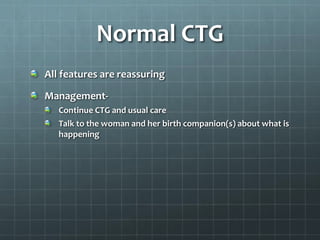
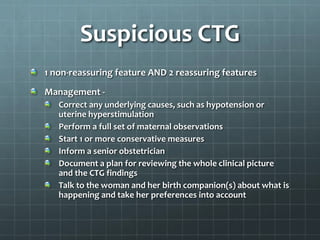
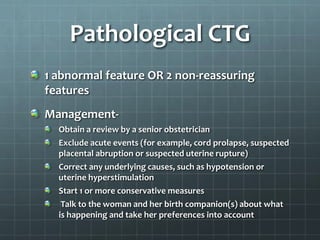
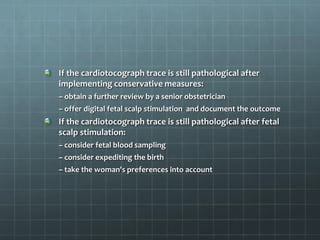
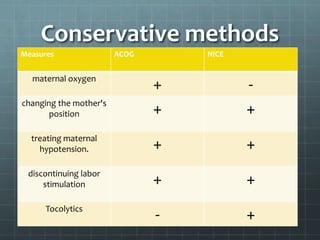
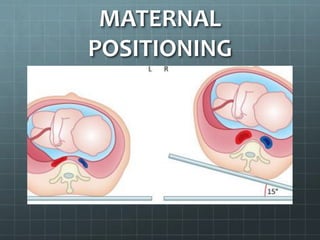
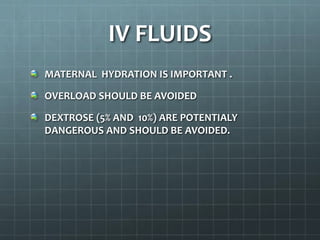
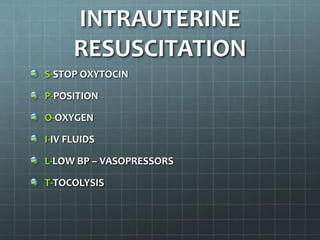
This document provides guidance on cardiotocography (CTG), which assesses fetal well-being by monitoring the fetal heart rate and uterine contractions. It outlines the indications for CTG, how to perform and interpret a CTG, management based on CTG findings, and conservative measures that can be tried to improve abnormal tracings before expediting delivery. Key aspects of CTG include assessing the baseline heart rate, variability, accelerations, decelerations, and developing an overall impression of normal, suspicious, or pathological to guide management decisions.