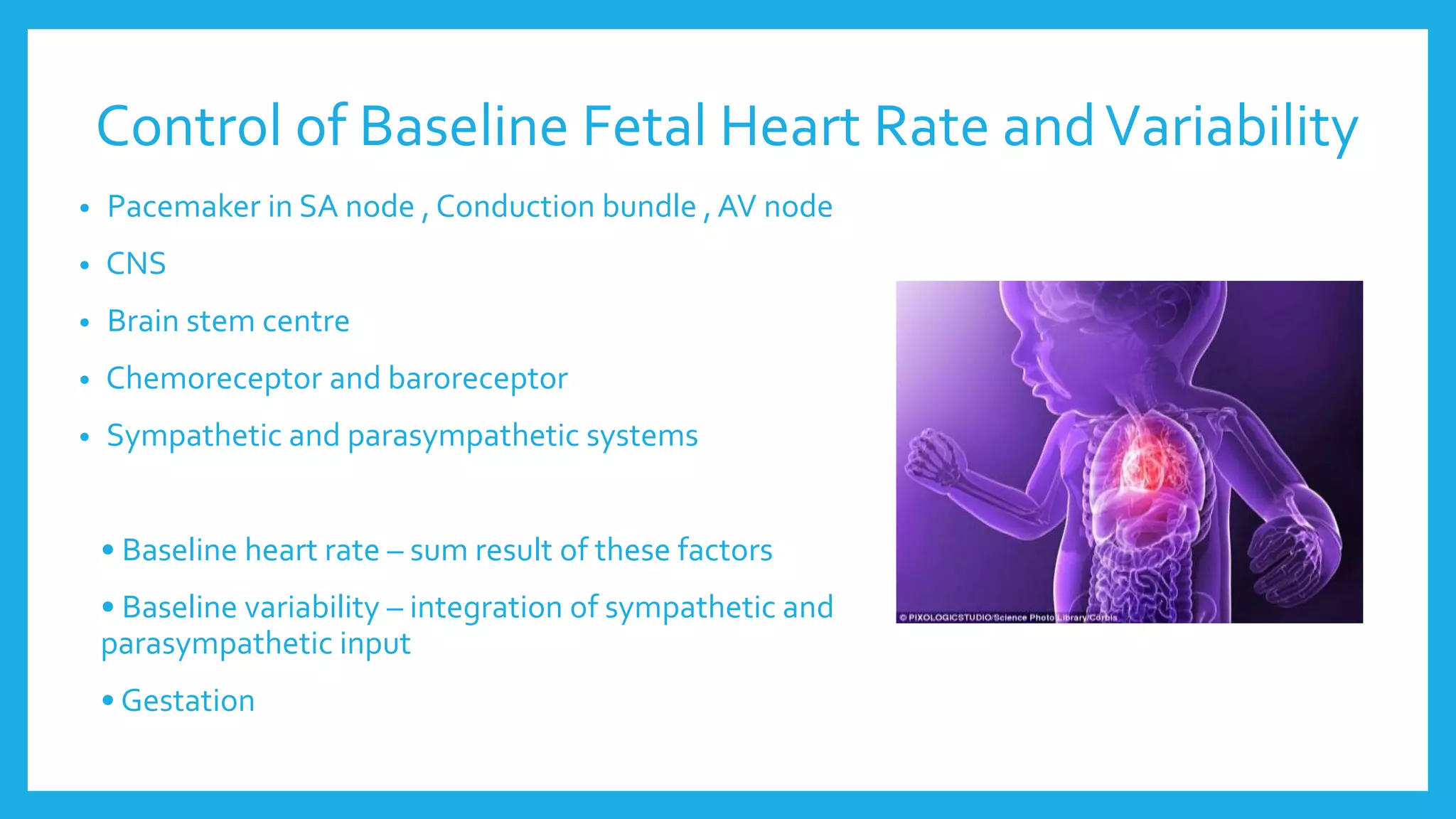
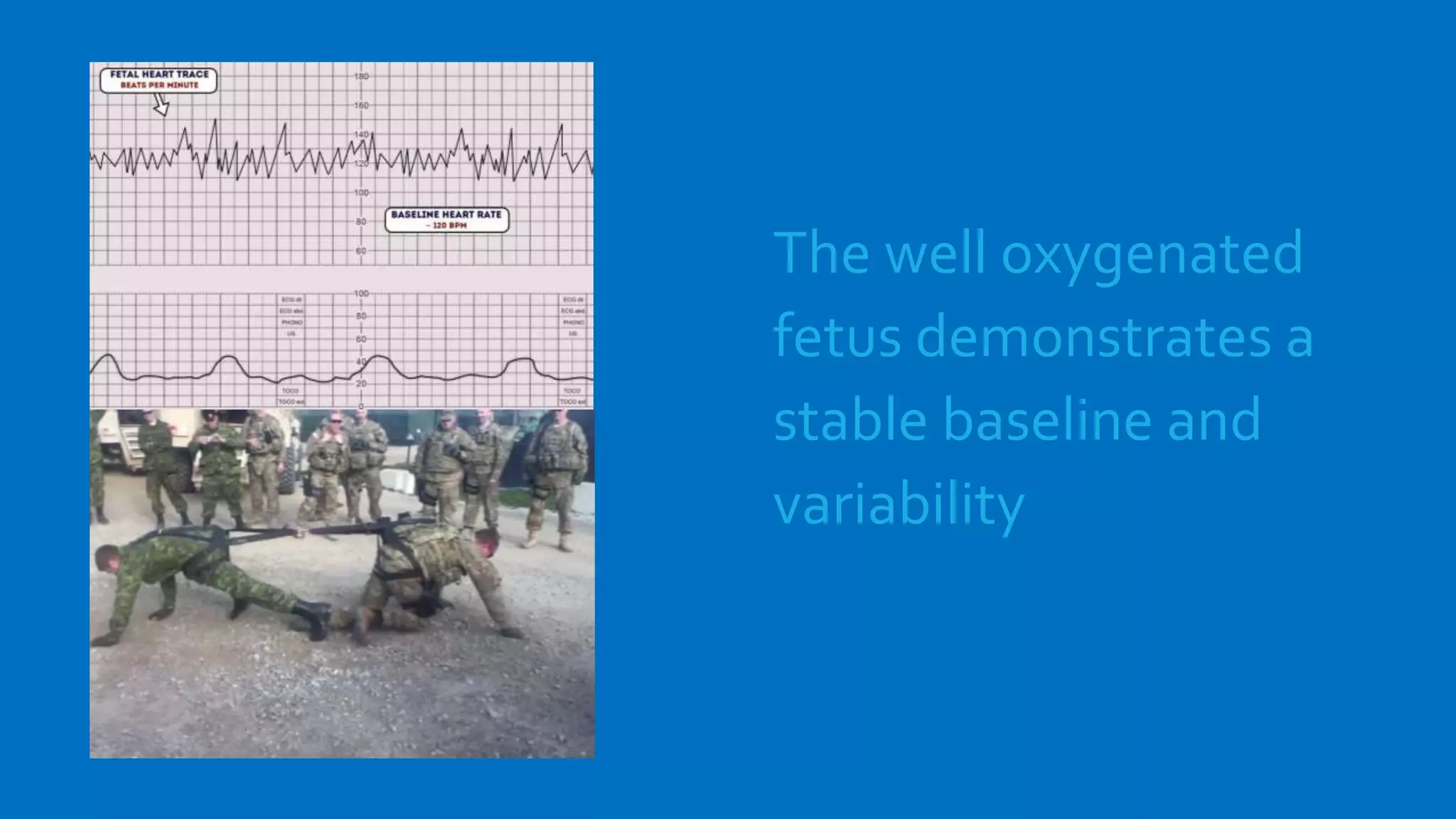
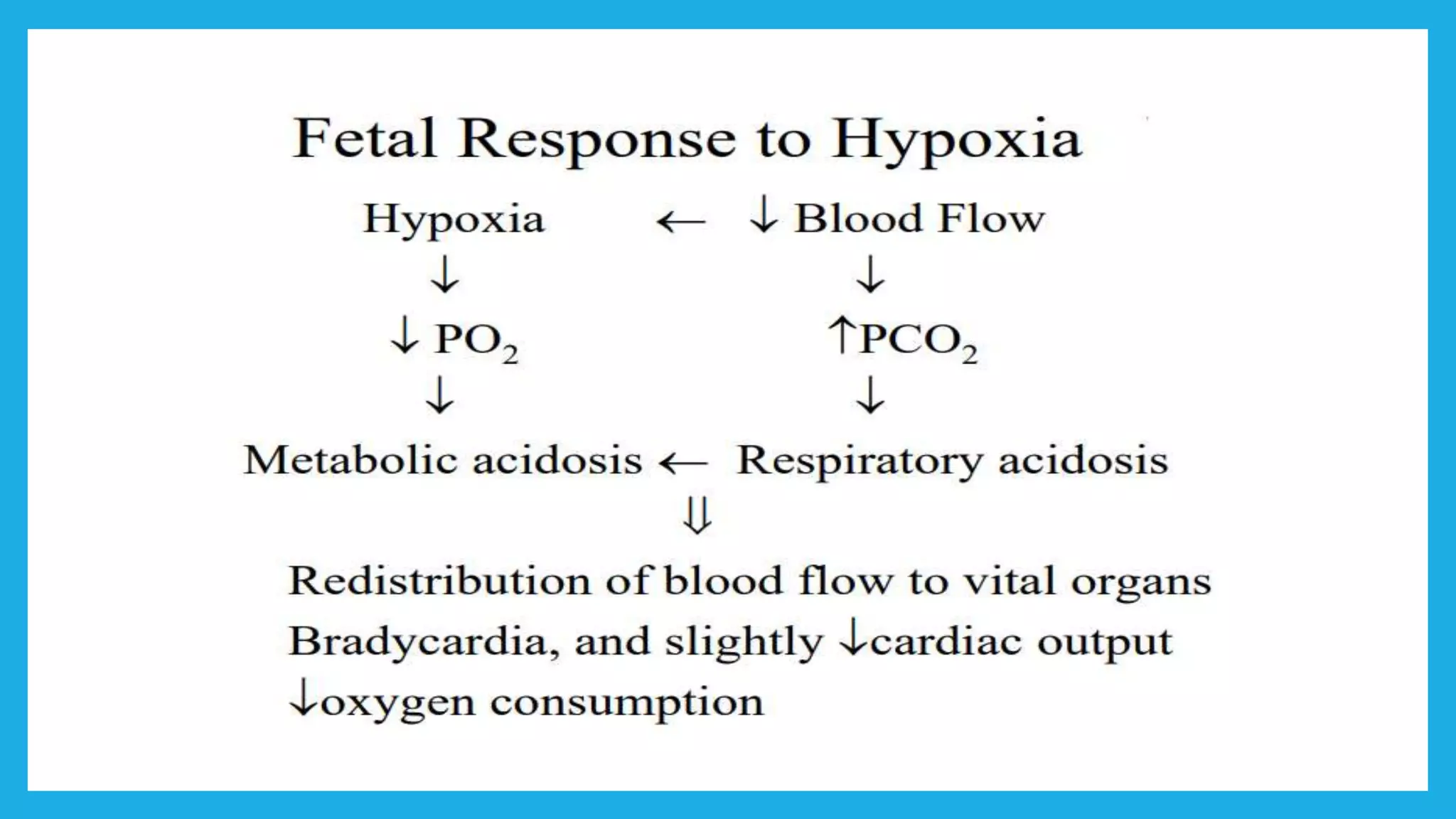
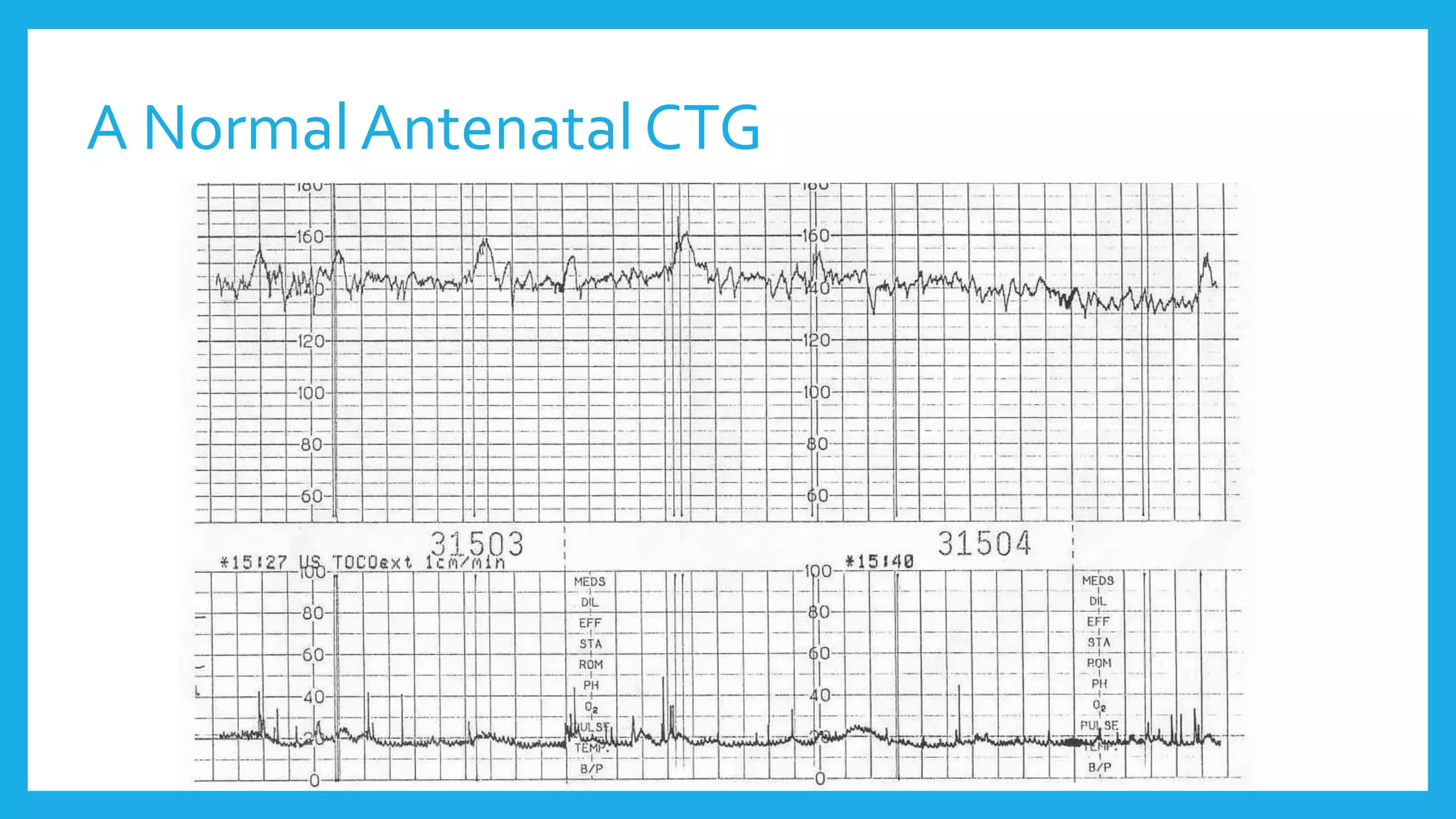
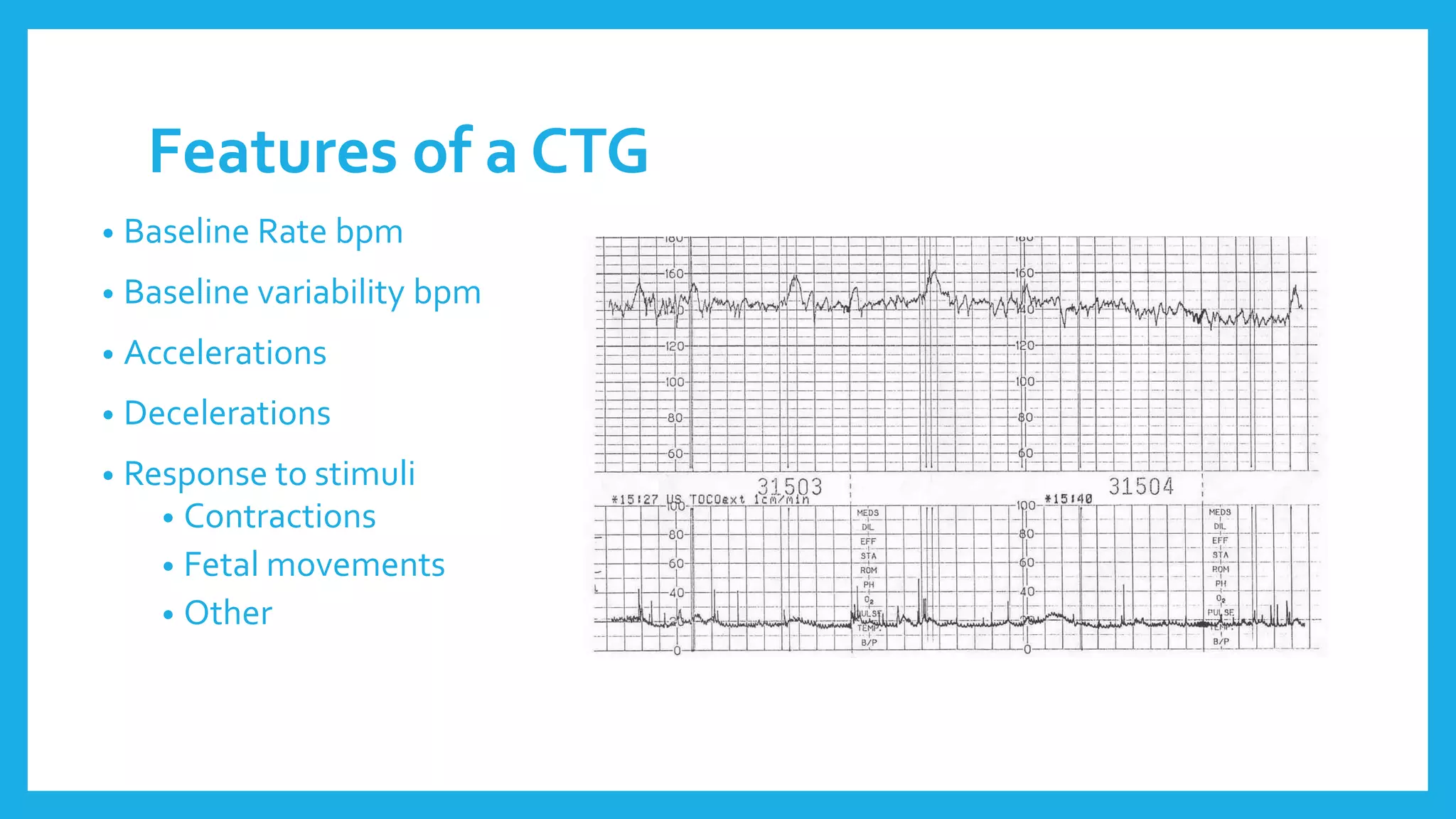
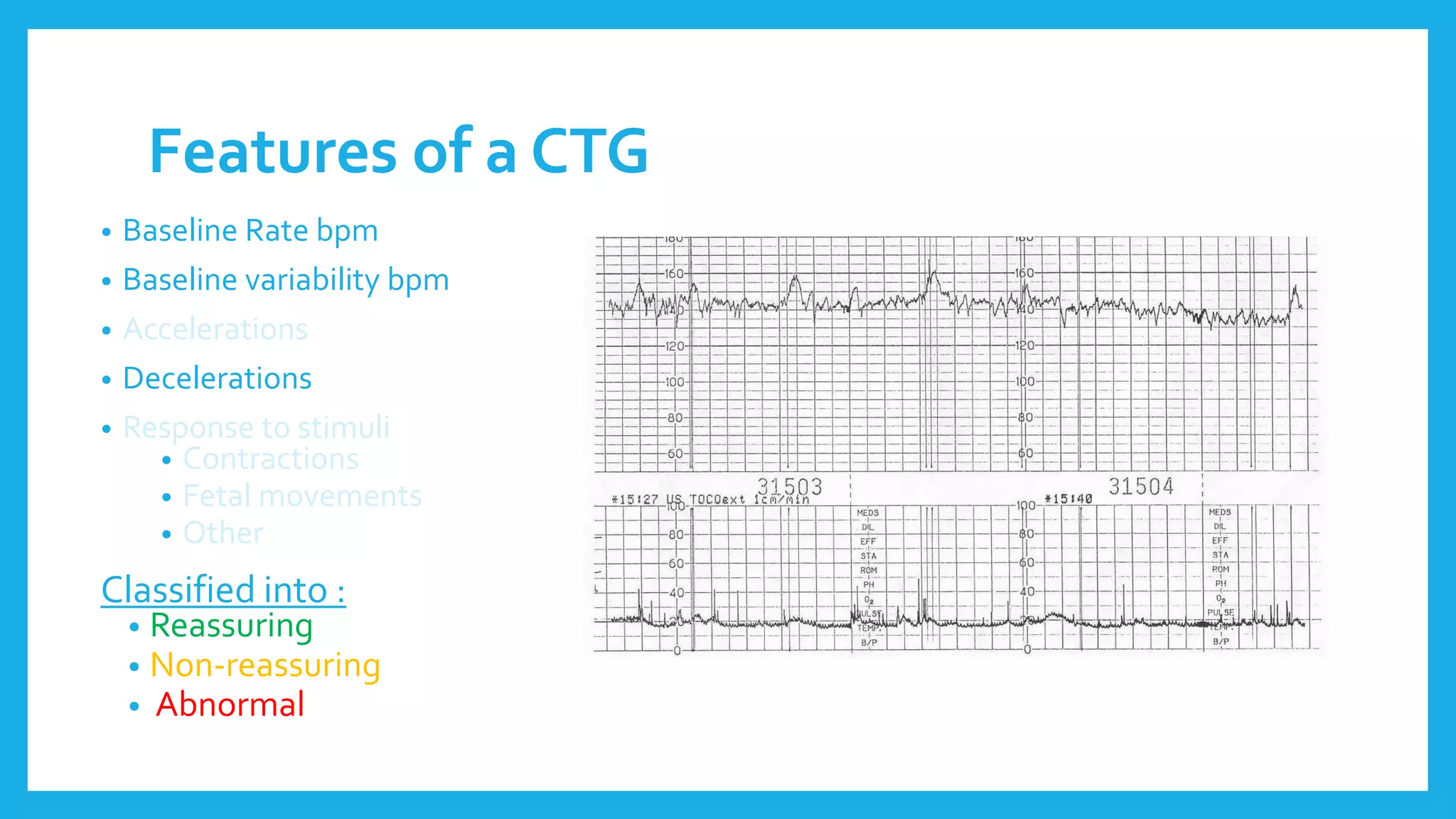
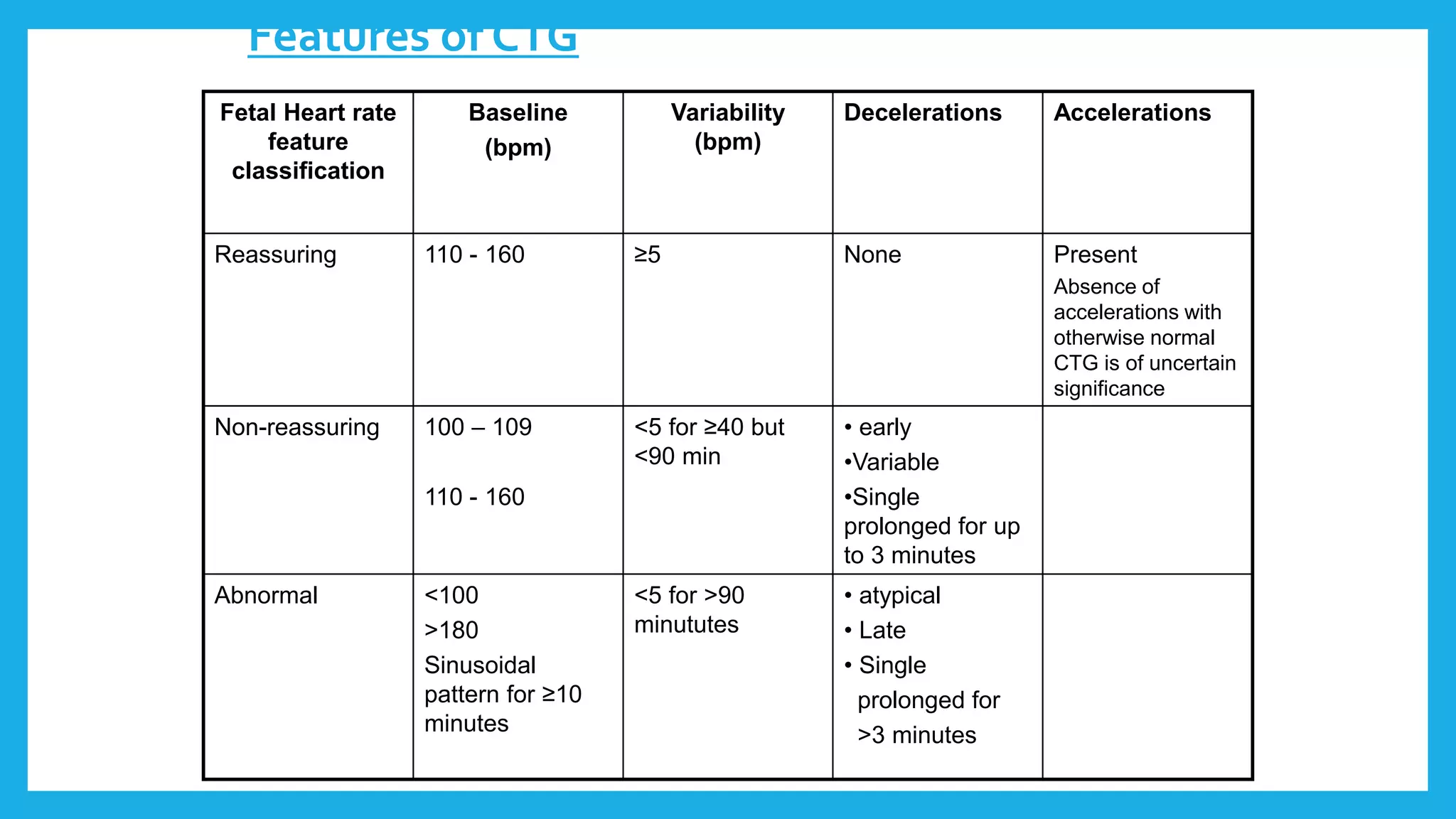
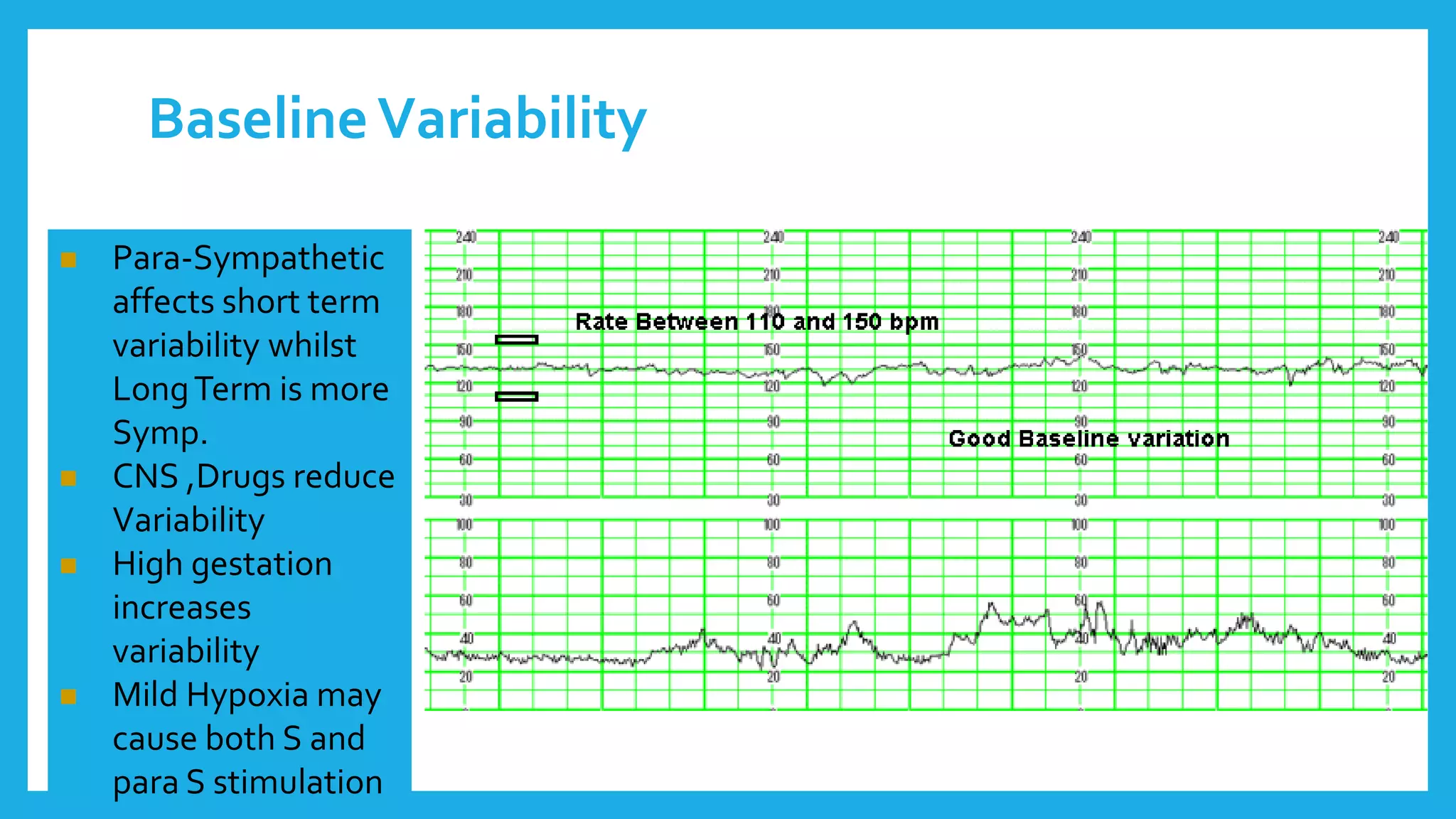
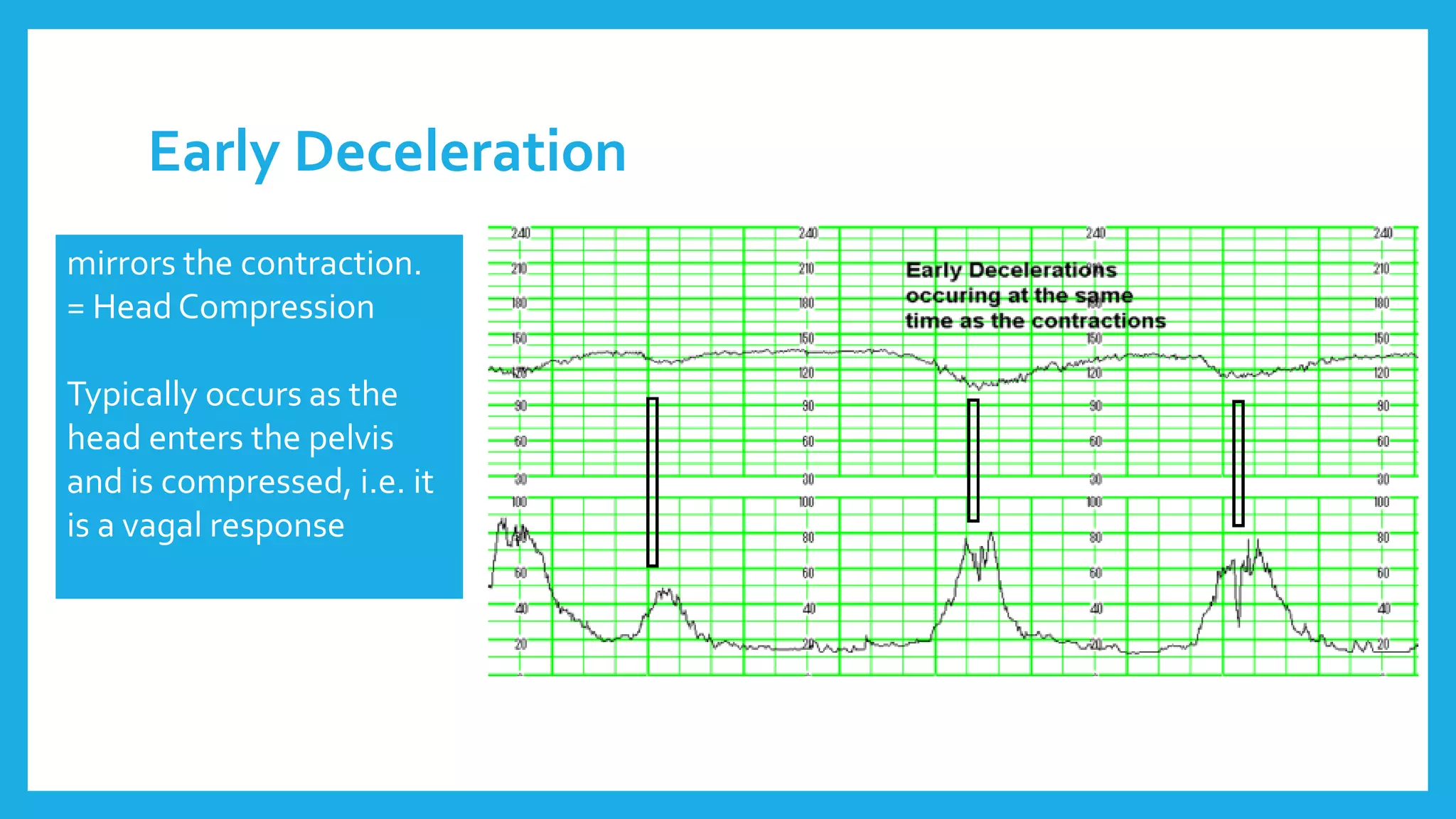
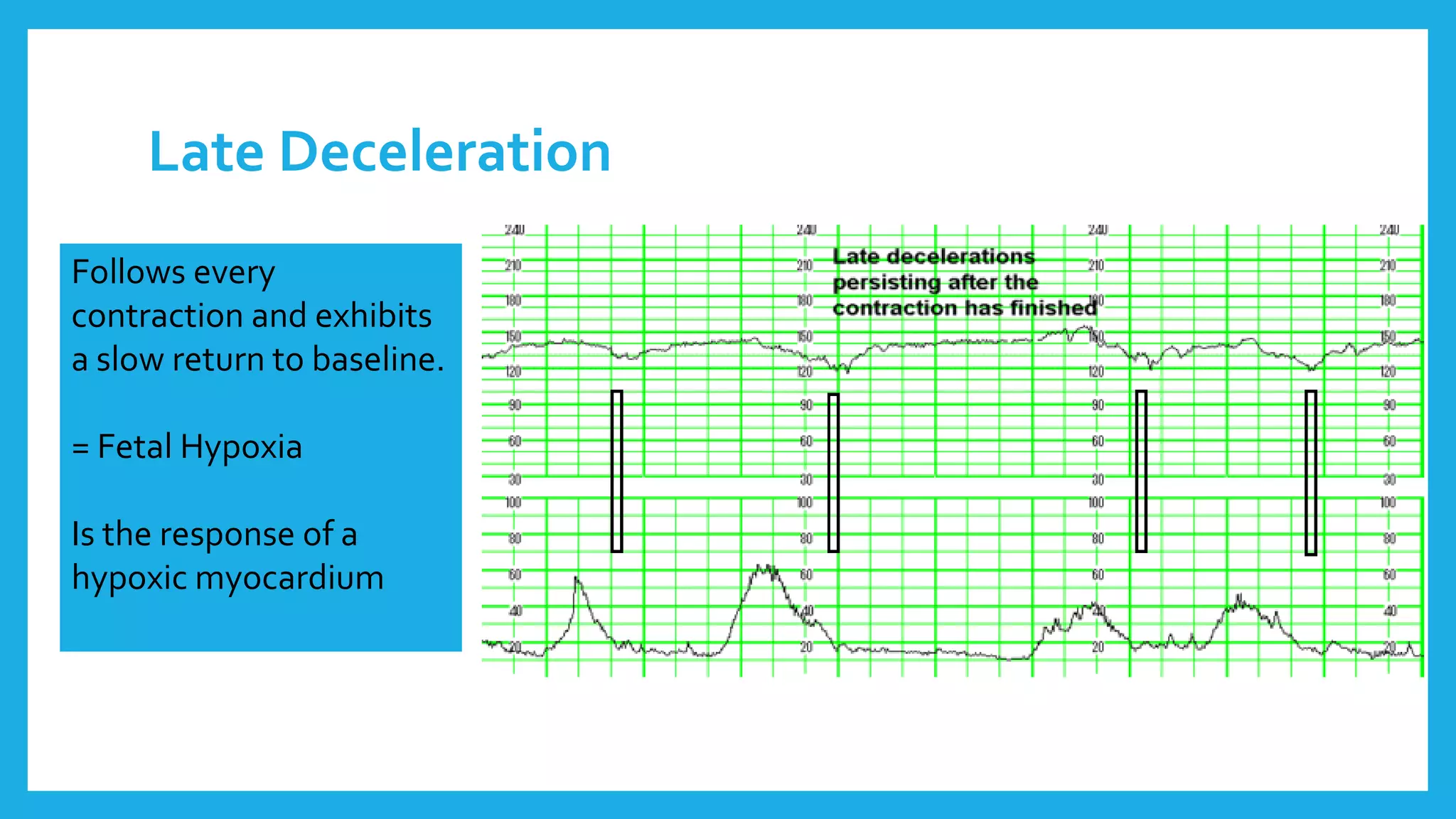
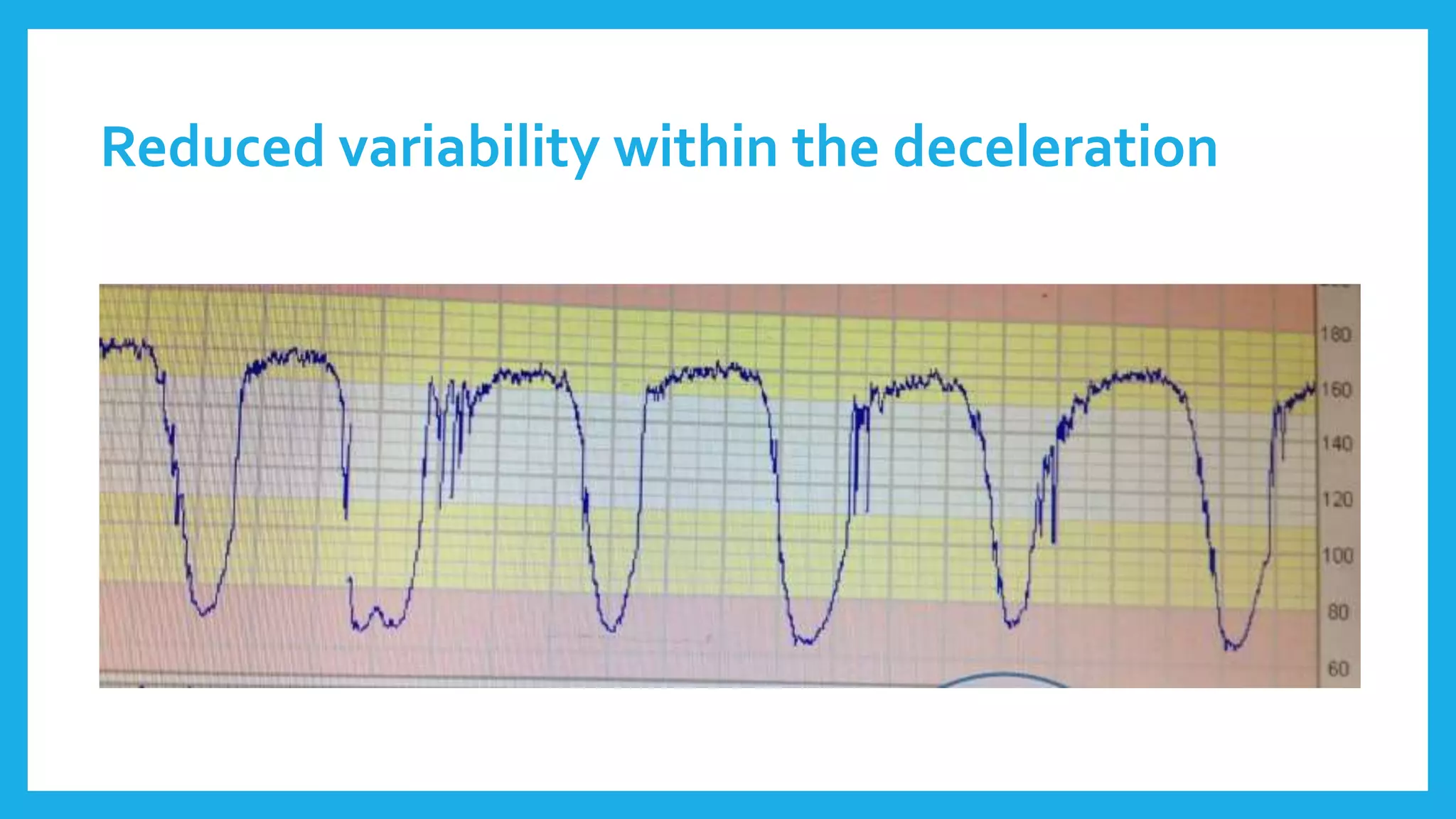
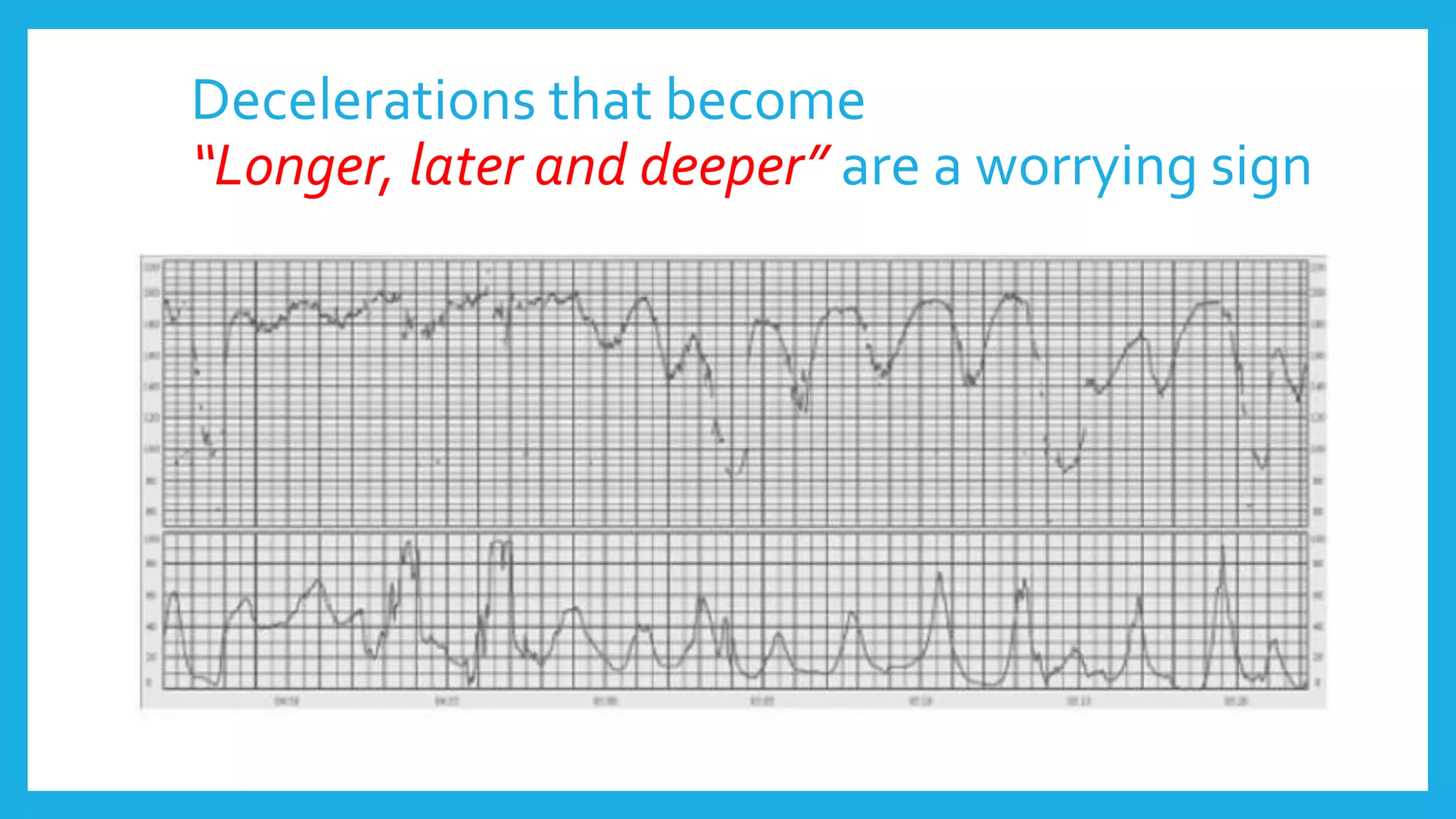
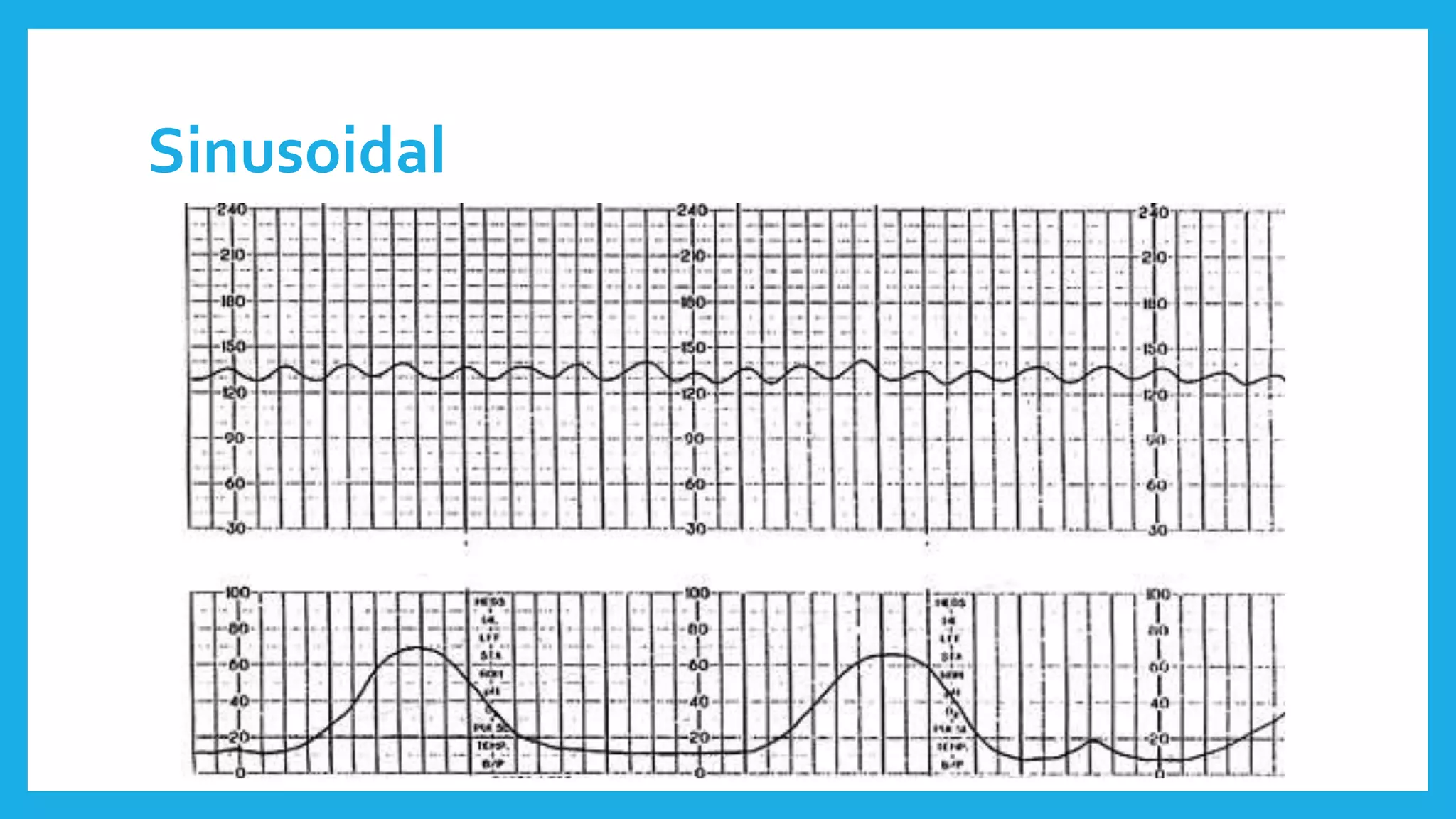
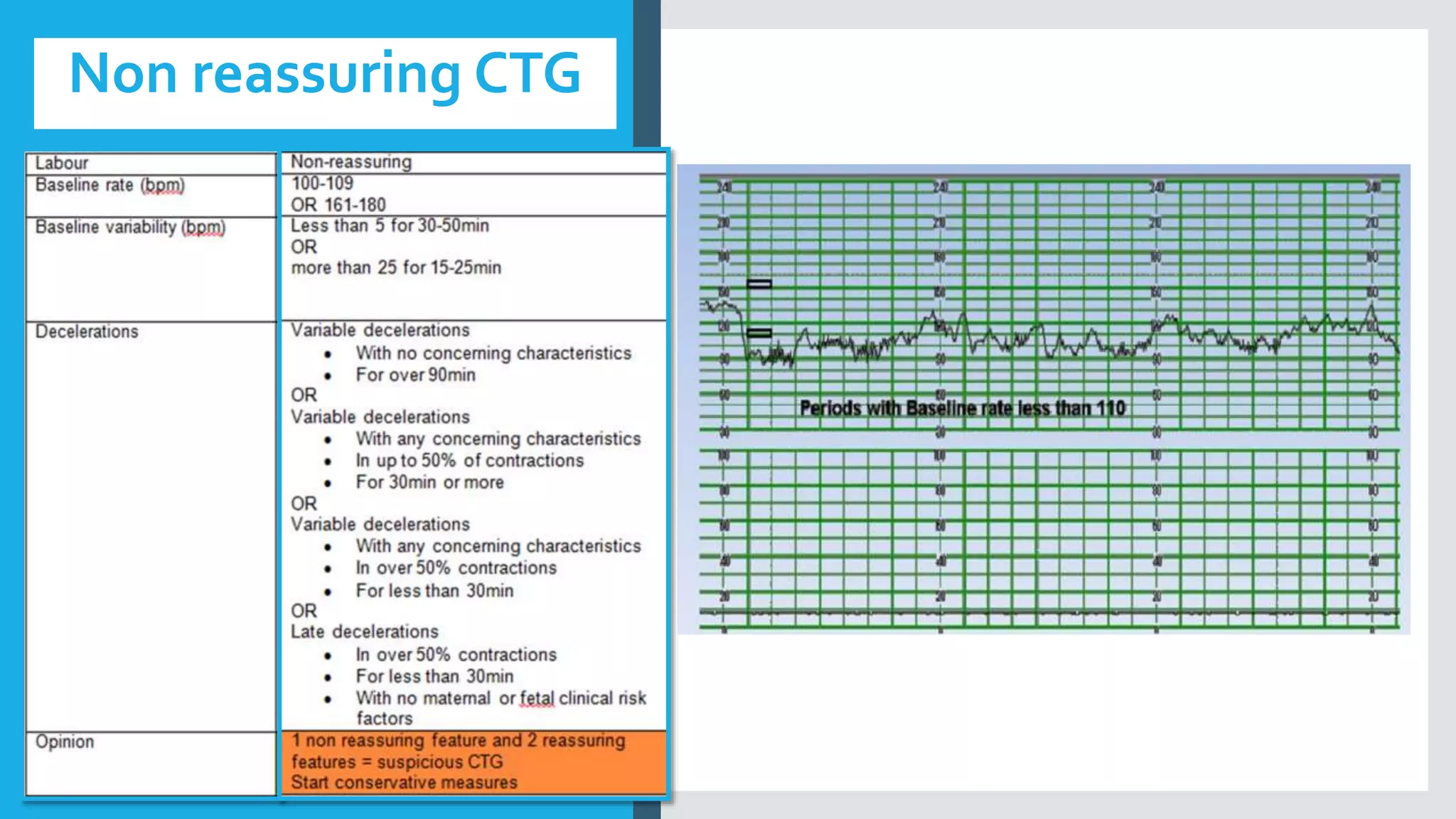
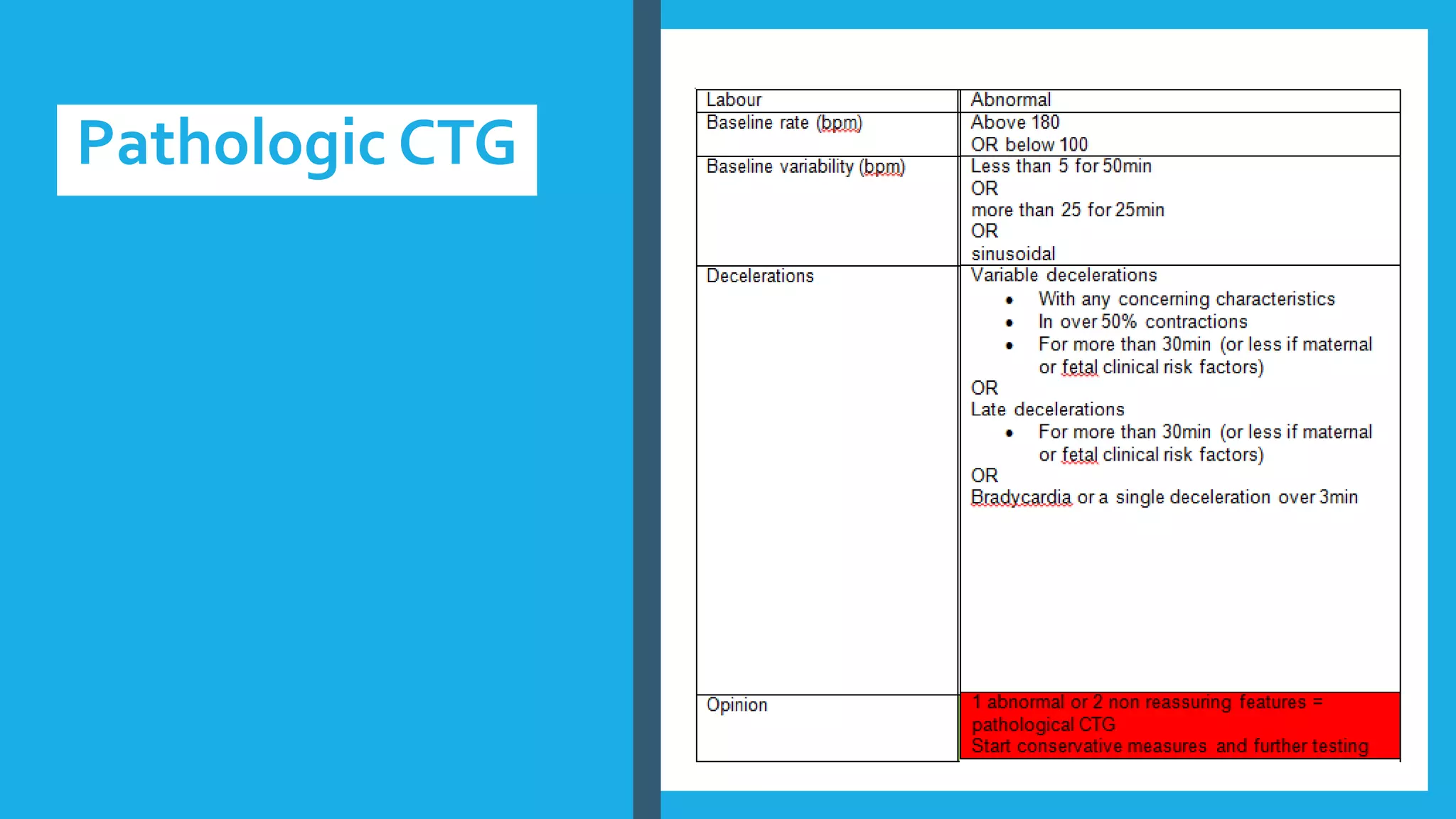
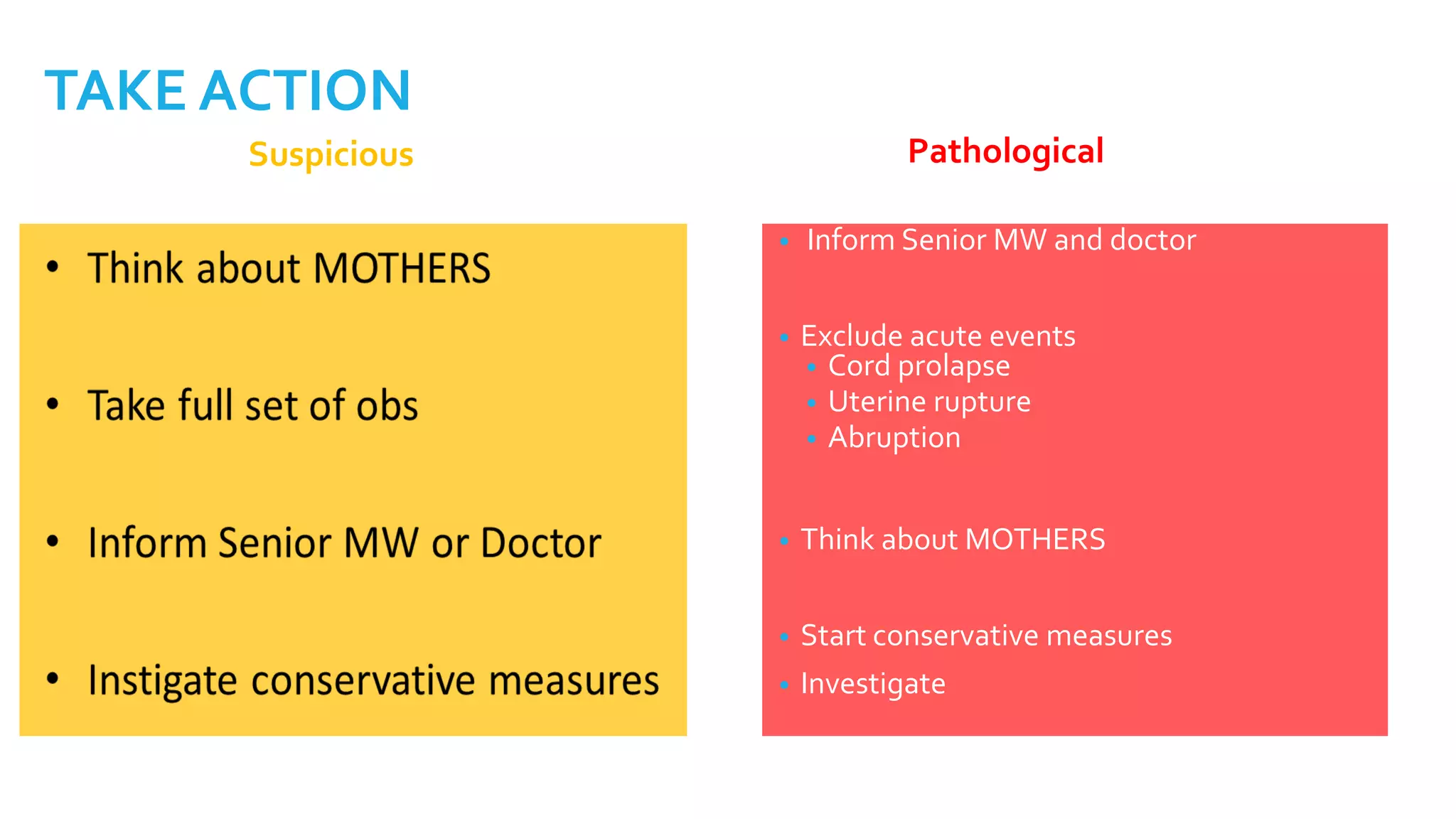
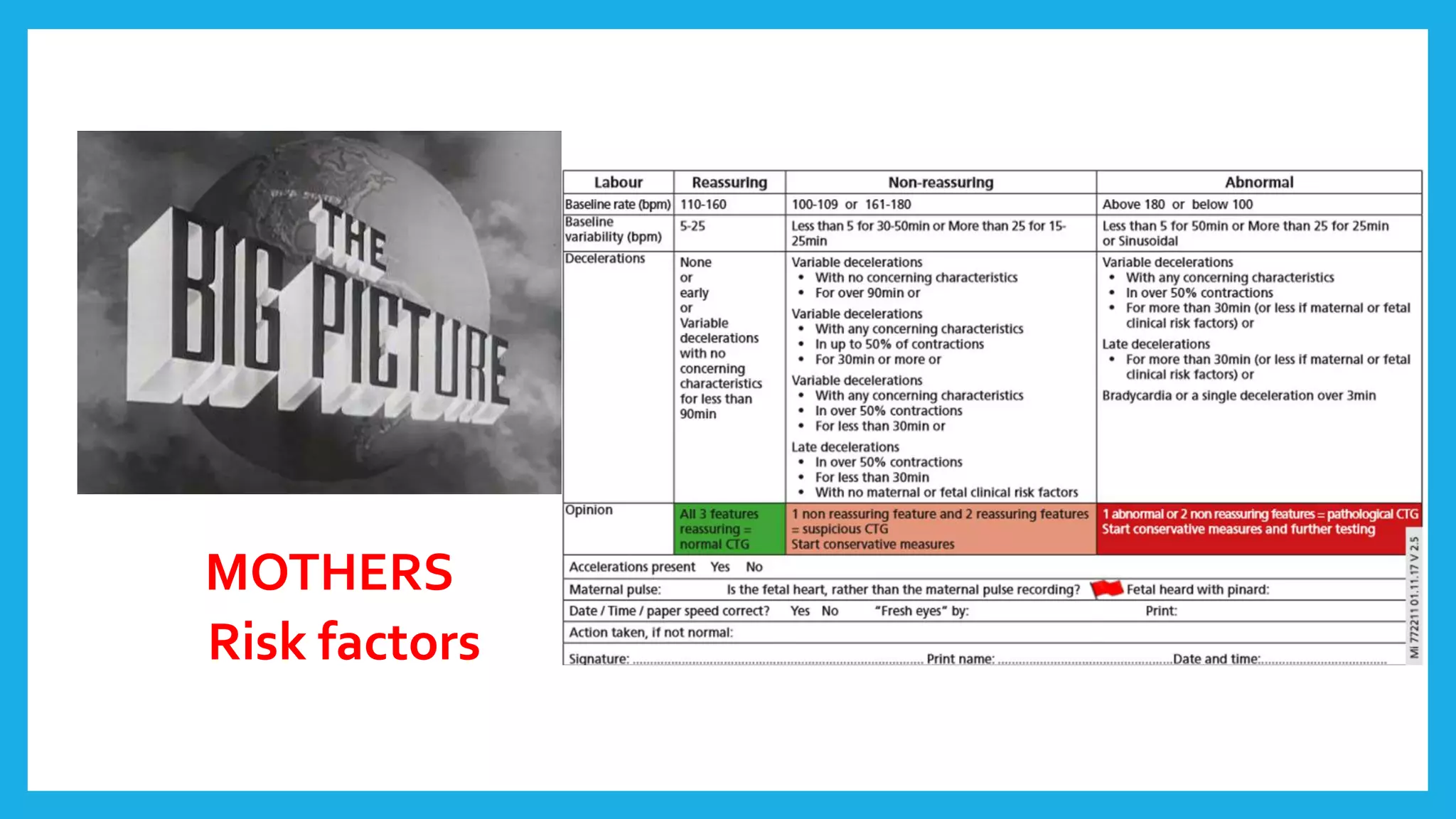
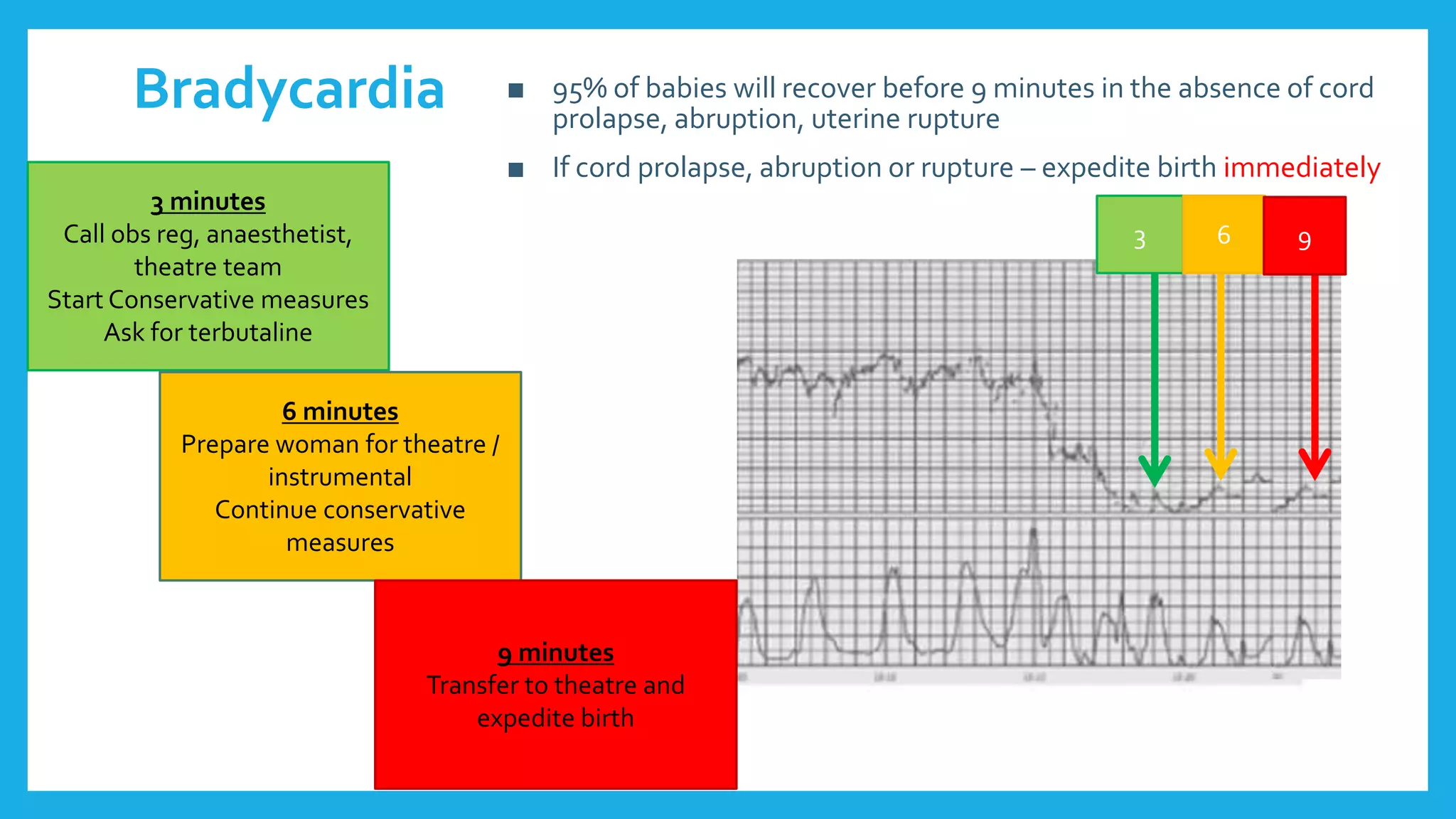
The document outlines fetal physiology during labor, detailing how a fetus adapts to labor conditions through various physiological mechanisms, including the regulation of heart rate and variability. It describes the classification of cardiotocograph (CTG) features into reassuring, non-reassuring, and abnormal categories based on heart rate and variability metrics, as well as the implications of different deceleration patterns. Additionally, it emphasizes the importance of monitoring CTG patterns to determine necessary actions, especially in cases of abnormal findings indicating potential fetal distress.