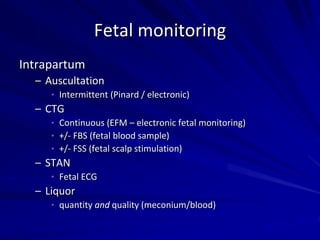
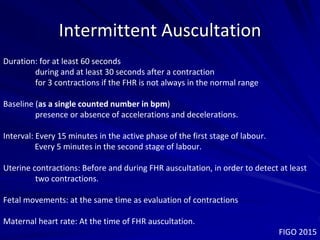
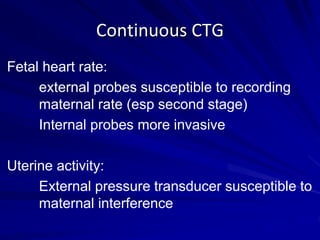
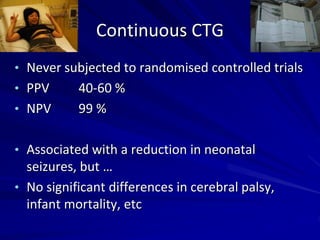
This document provides an overview of a course on fetal monitoring and CTG interpretation. It discusses:
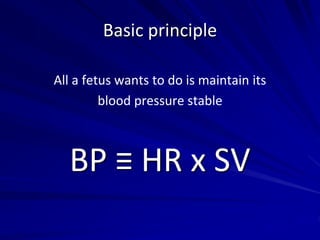
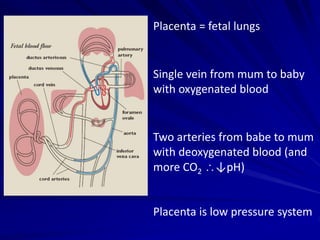
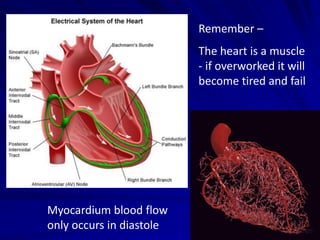
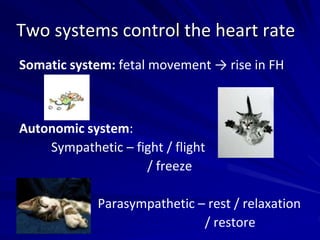
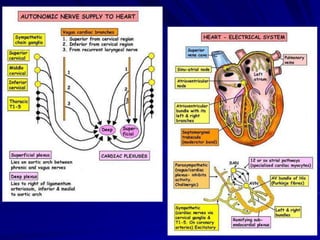
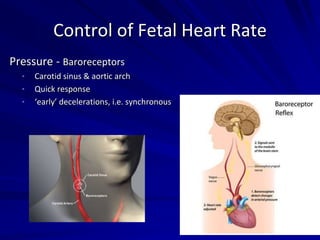
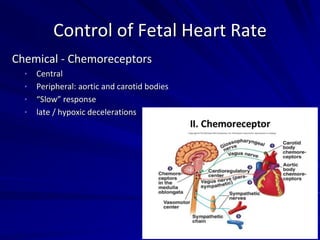
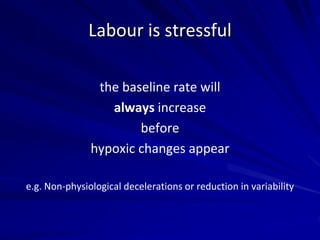
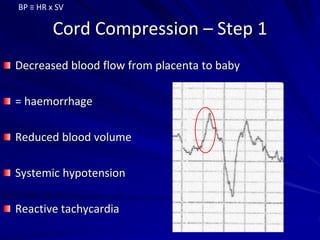
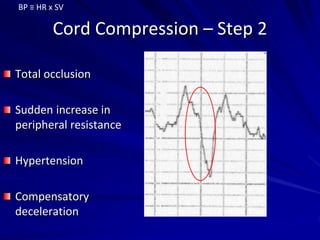
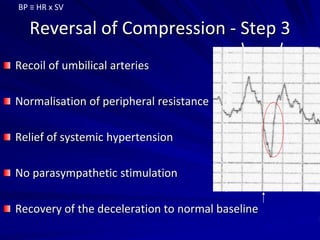
- The physiology and pathophysiology of fetal heart rate regulation.
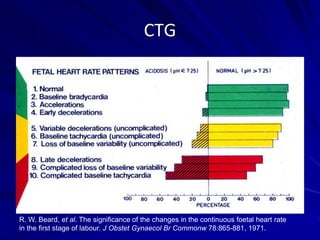
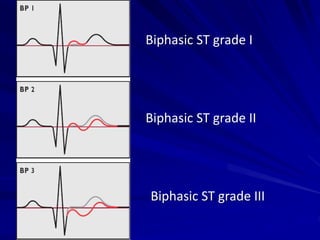
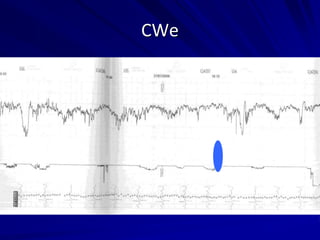
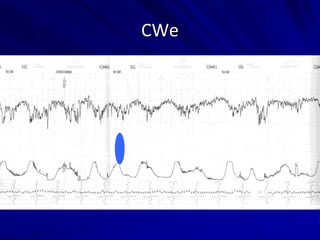
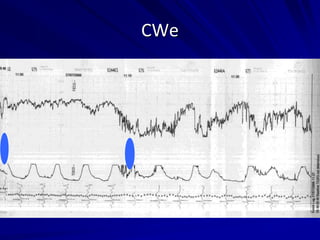
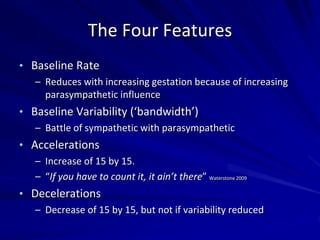
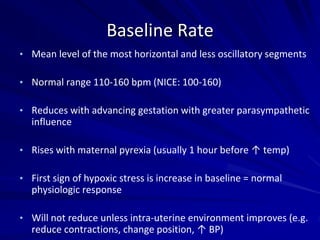
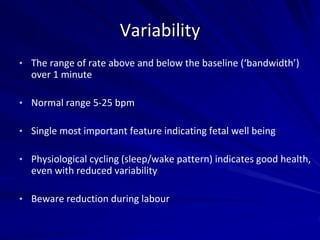
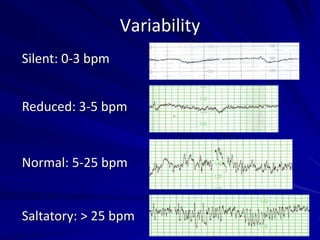
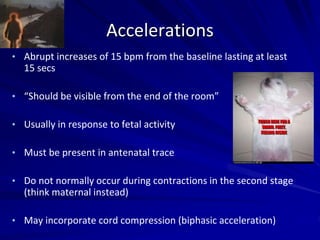
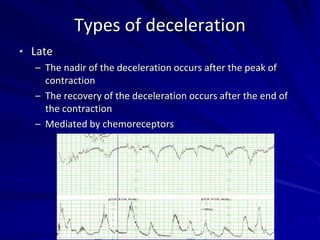
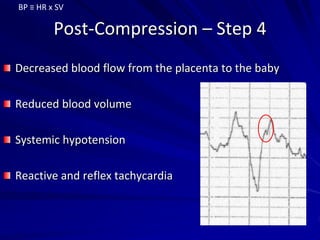
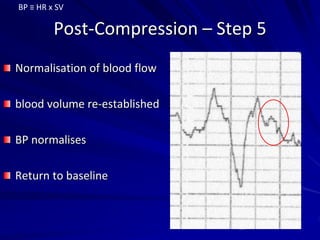
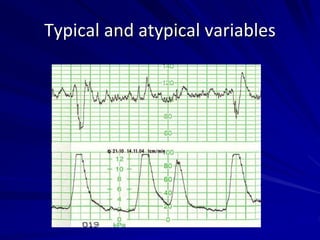
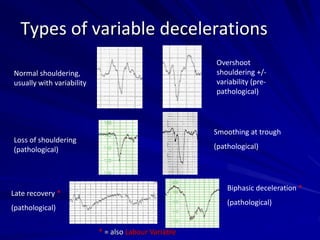
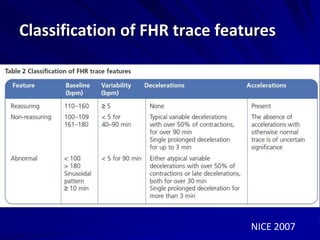
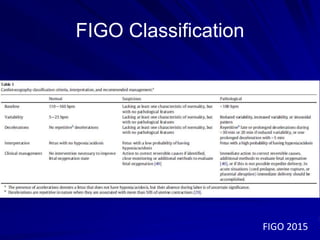
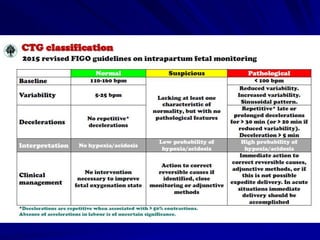
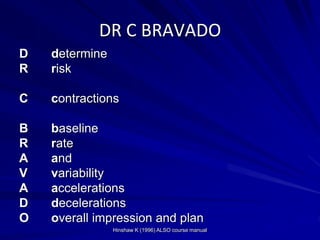
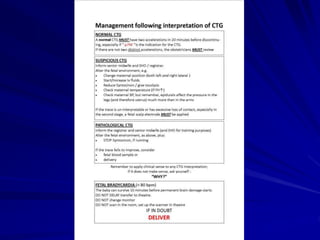
- The four key features of a CTG trace: baseline rate, variability, accelerations, and decelerations. It defines each feature and provides examples of normal and abnormal readings.
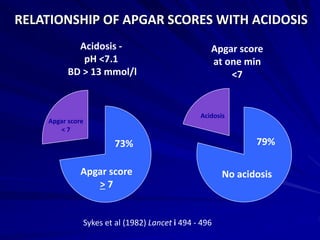
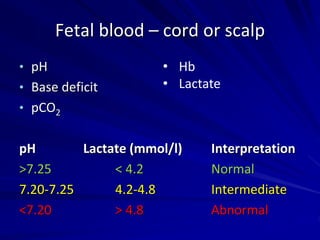
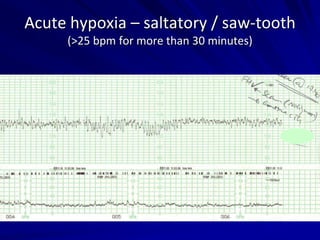
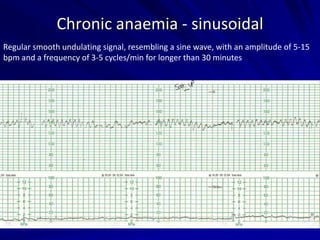
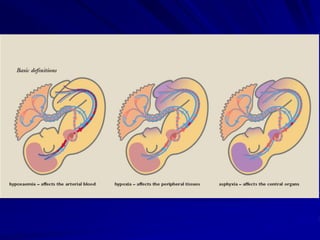
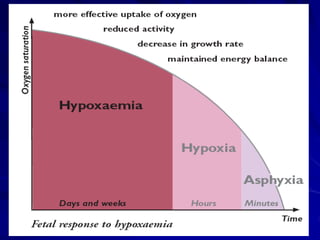
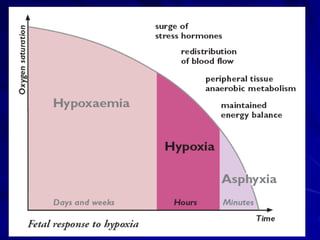
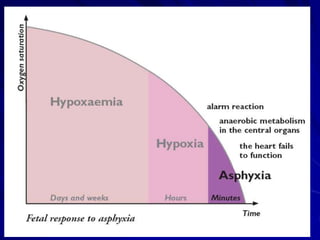
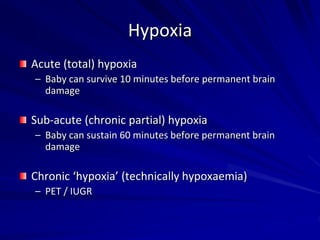
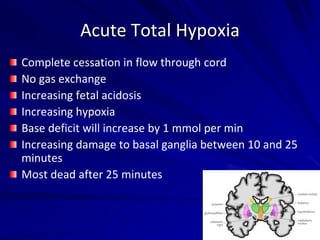
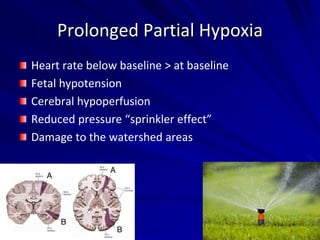
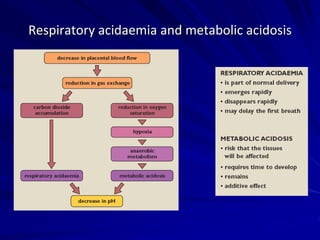
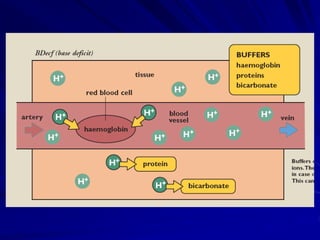
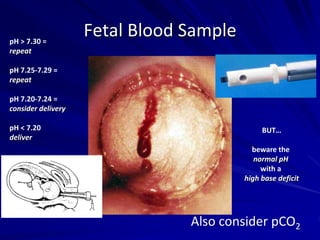
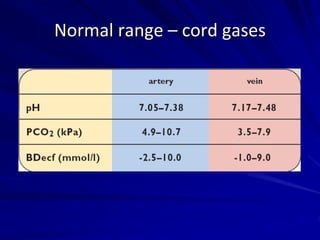
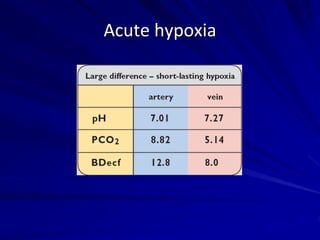
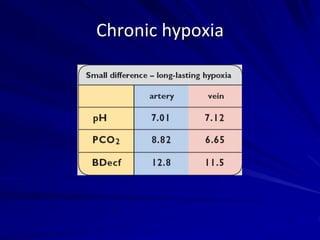
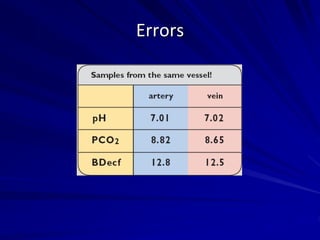
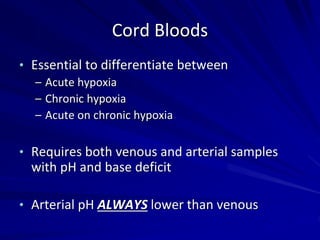
- Fetal acid-base status, including the differences between acute and chronic hypoxia. It discusses how to interpret cord blood gas results.
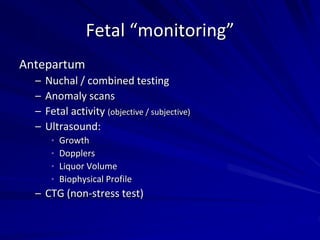
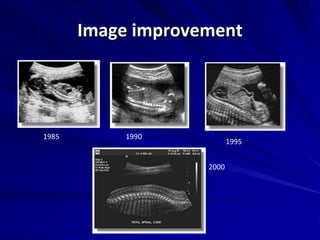
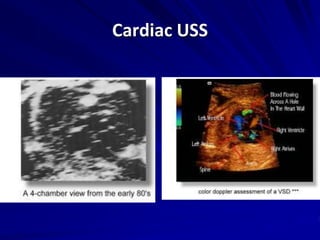
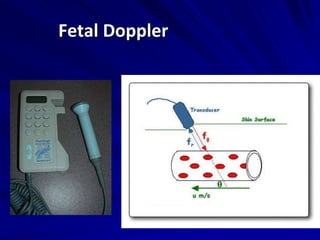
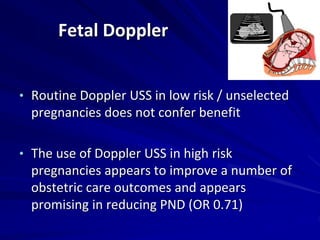
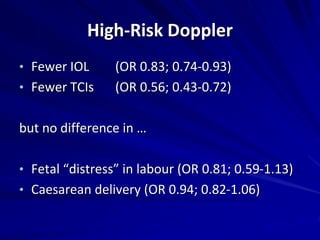
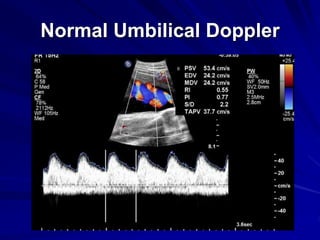
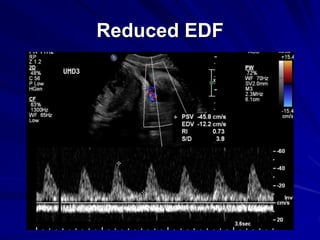
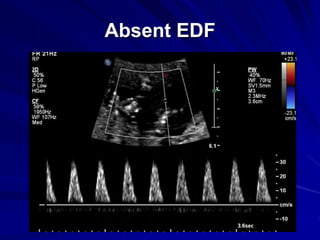
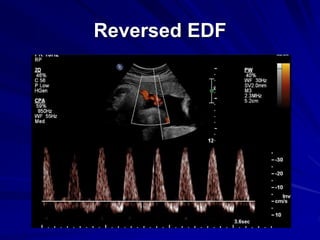
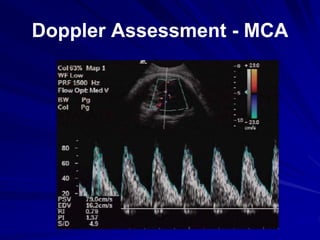
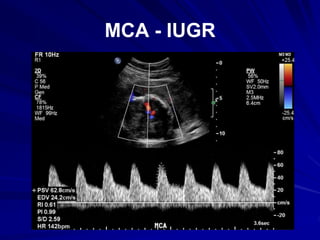
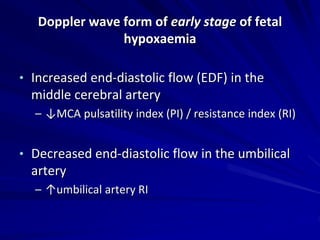
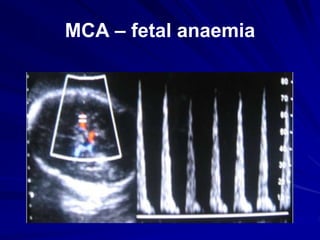
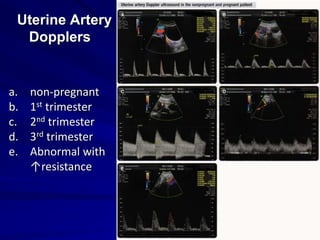
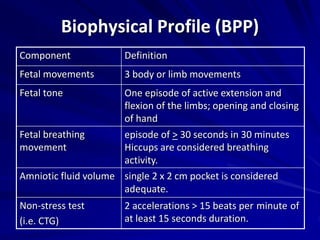
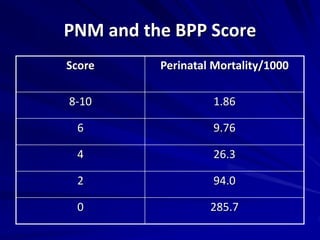
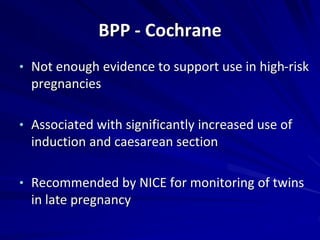
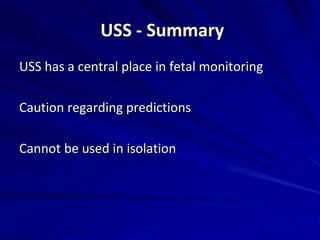
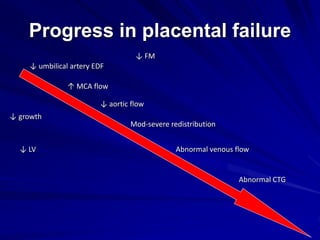
- The use of ultrasound in fetal monitoring, including cardiac ultrasound, biophysical profile, and Doppler assessments of umbilical and middle cerebral artery blood flow.
![The Aim of Obstetrics
Healthy mum
Healthy babe(s)
[happy family]
NOT a vaginal
delivery at any cost](https://image.slidesharecdn.com/48569bbf-1073-4015-bea4-f355b0e88b60-160226093320/85/The-DVH-MasterClass-Course-one-day-2016-5-320.jpg)