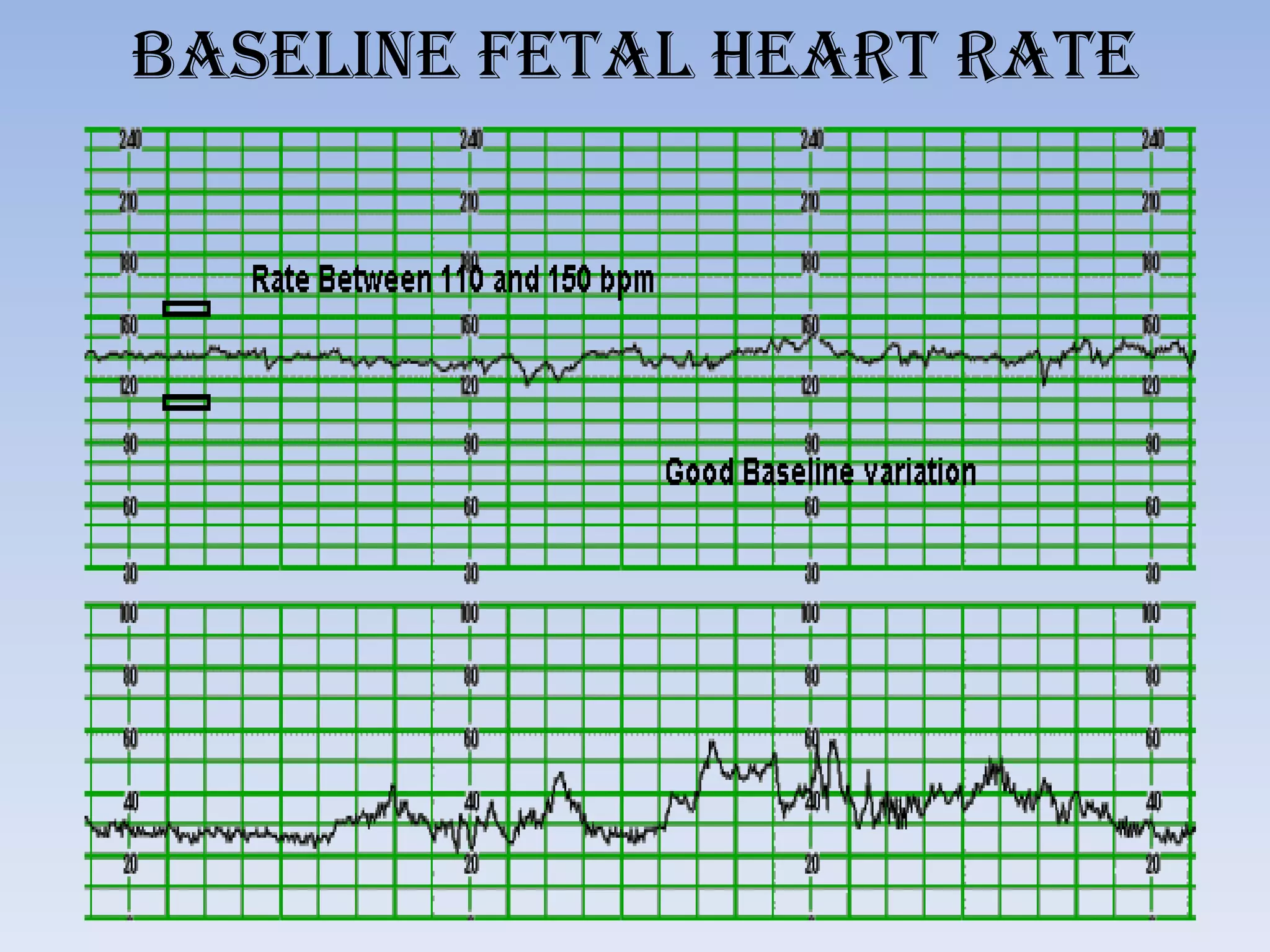
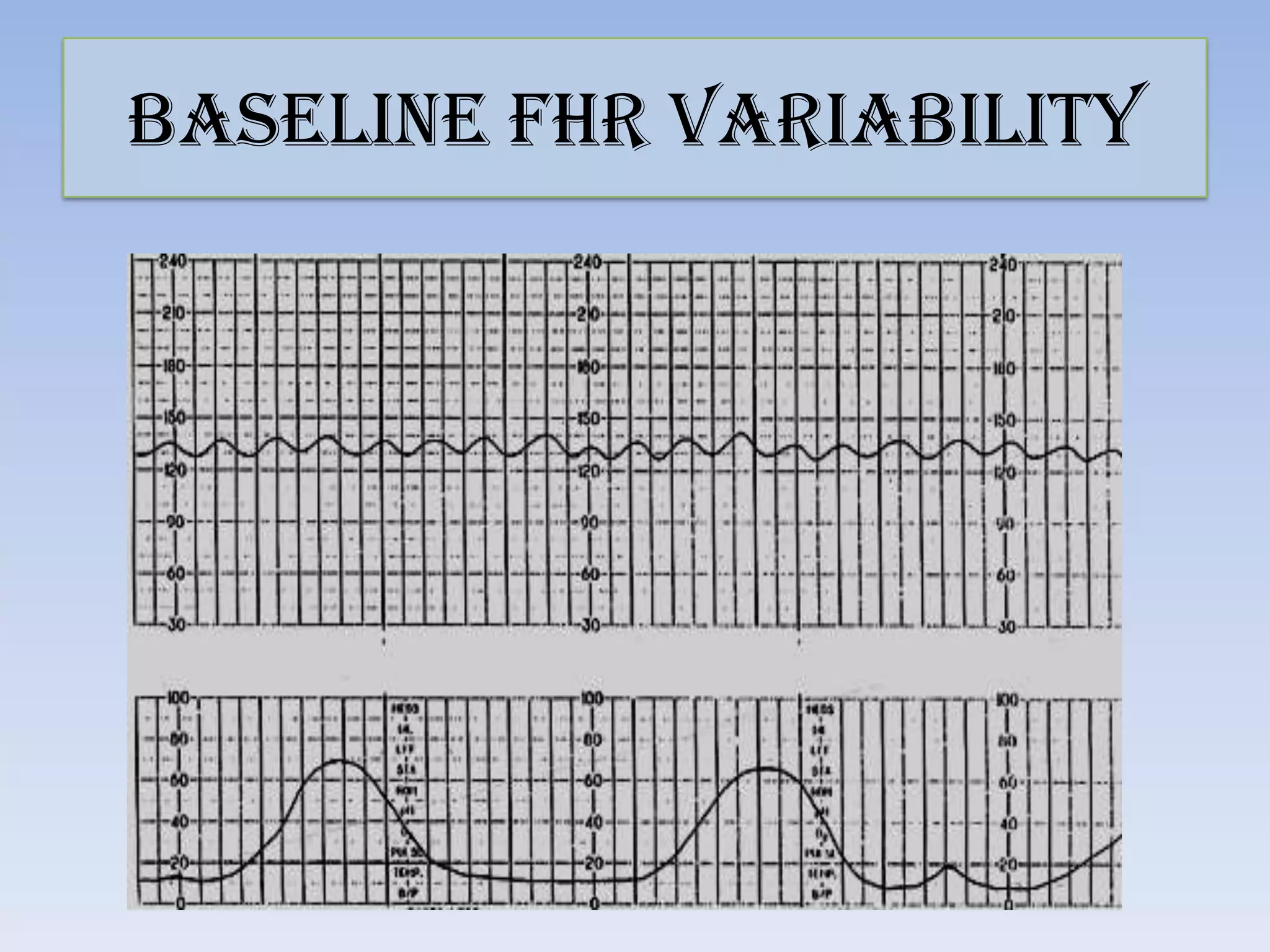
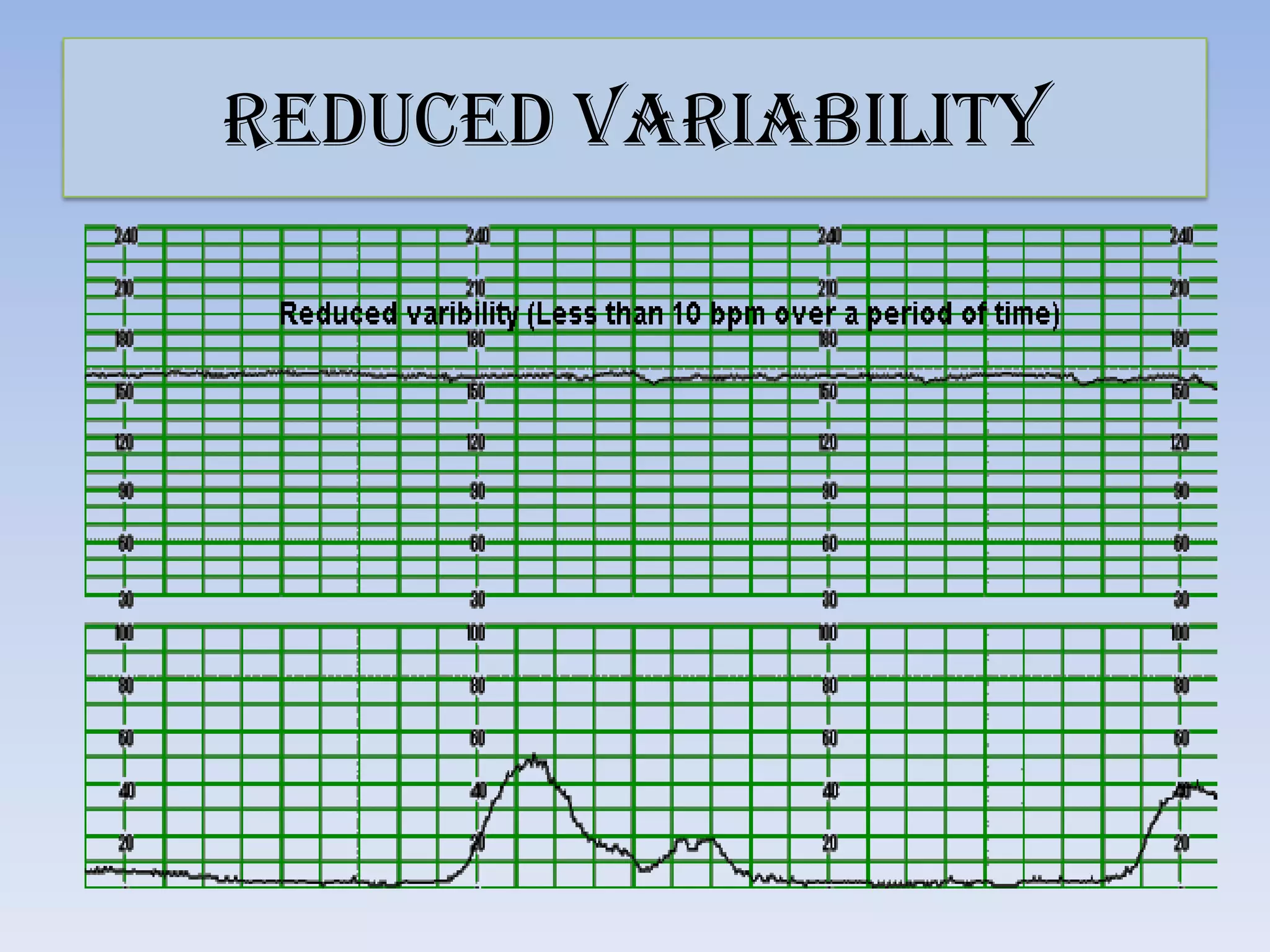
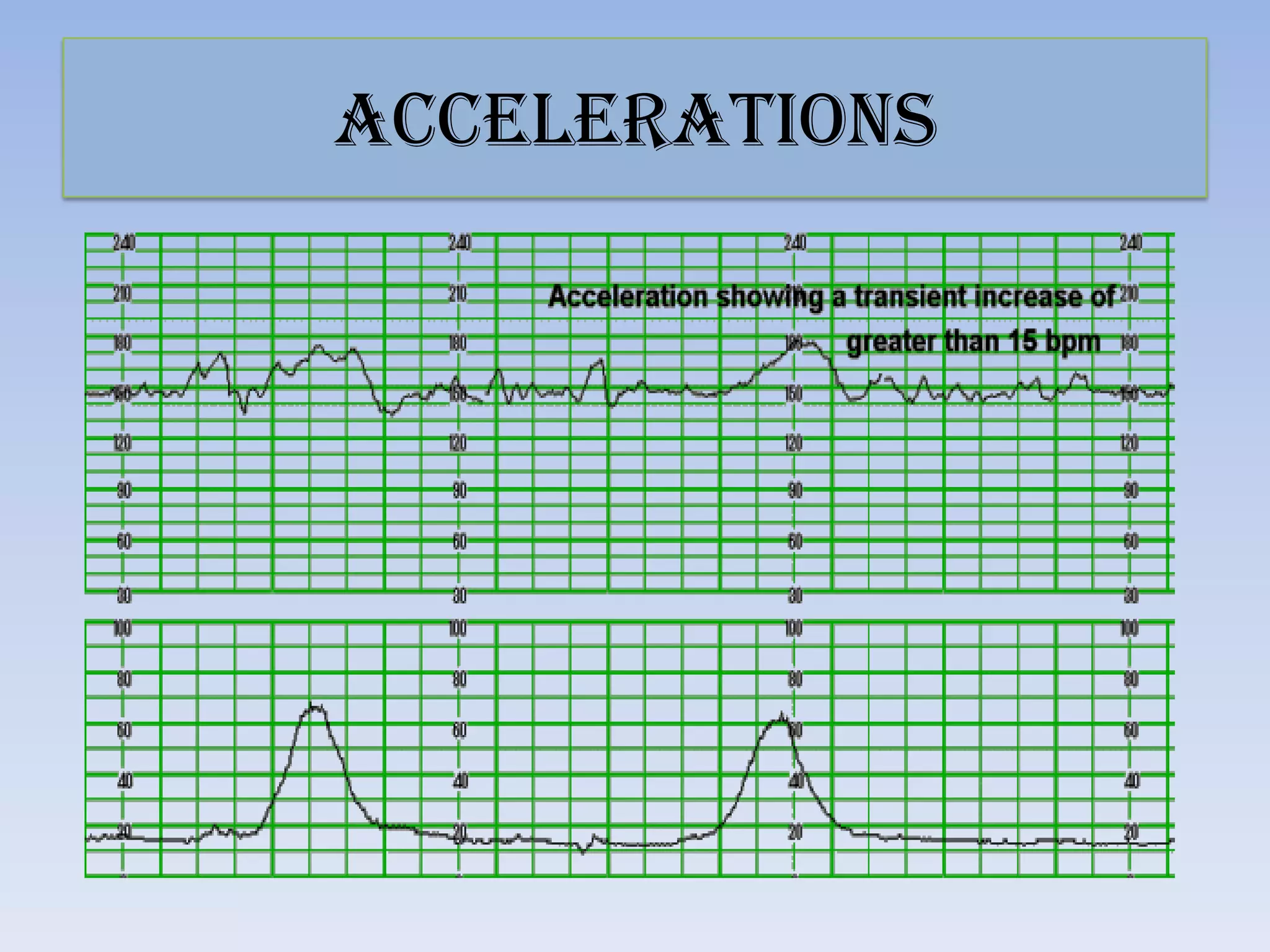
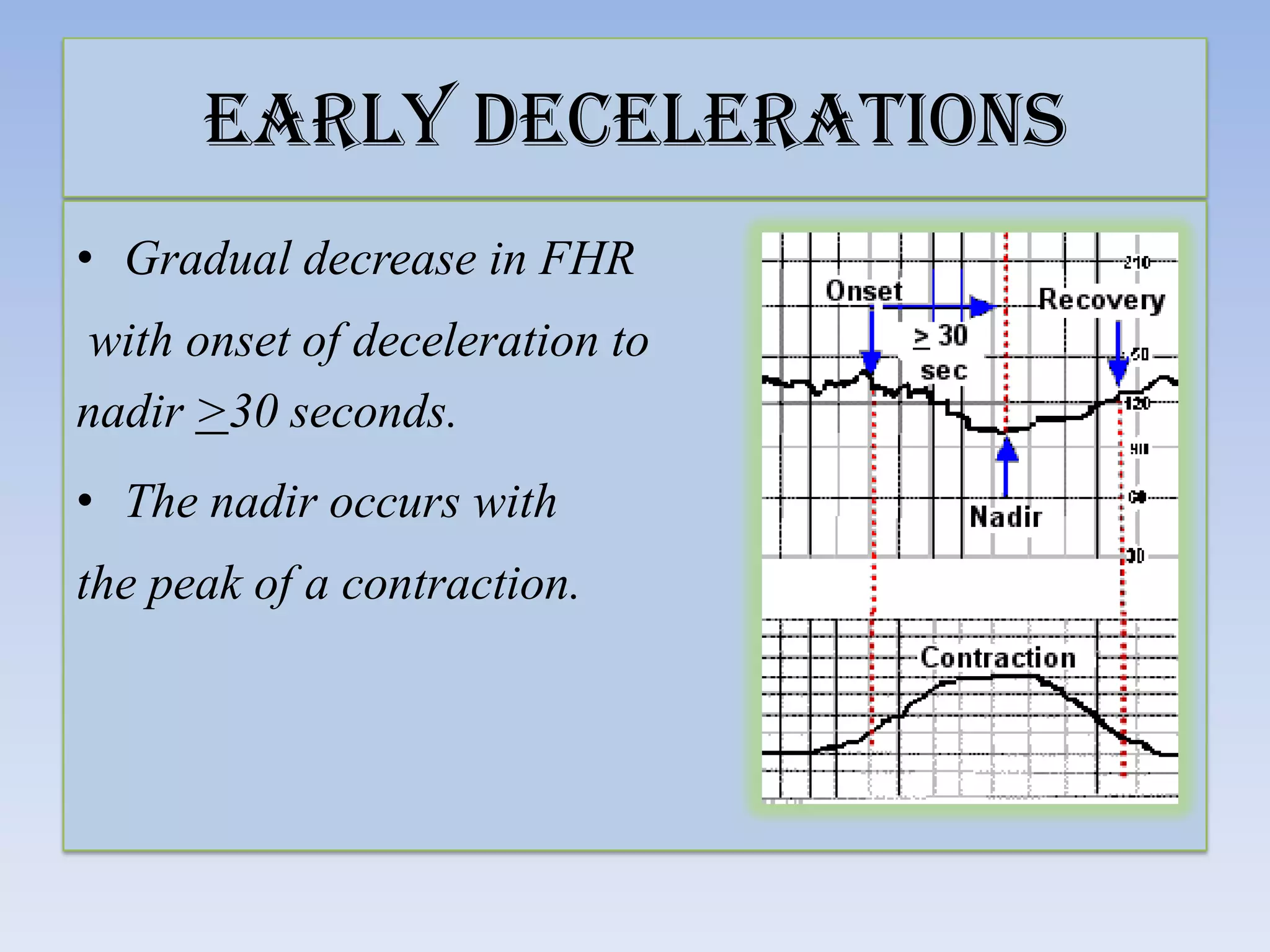
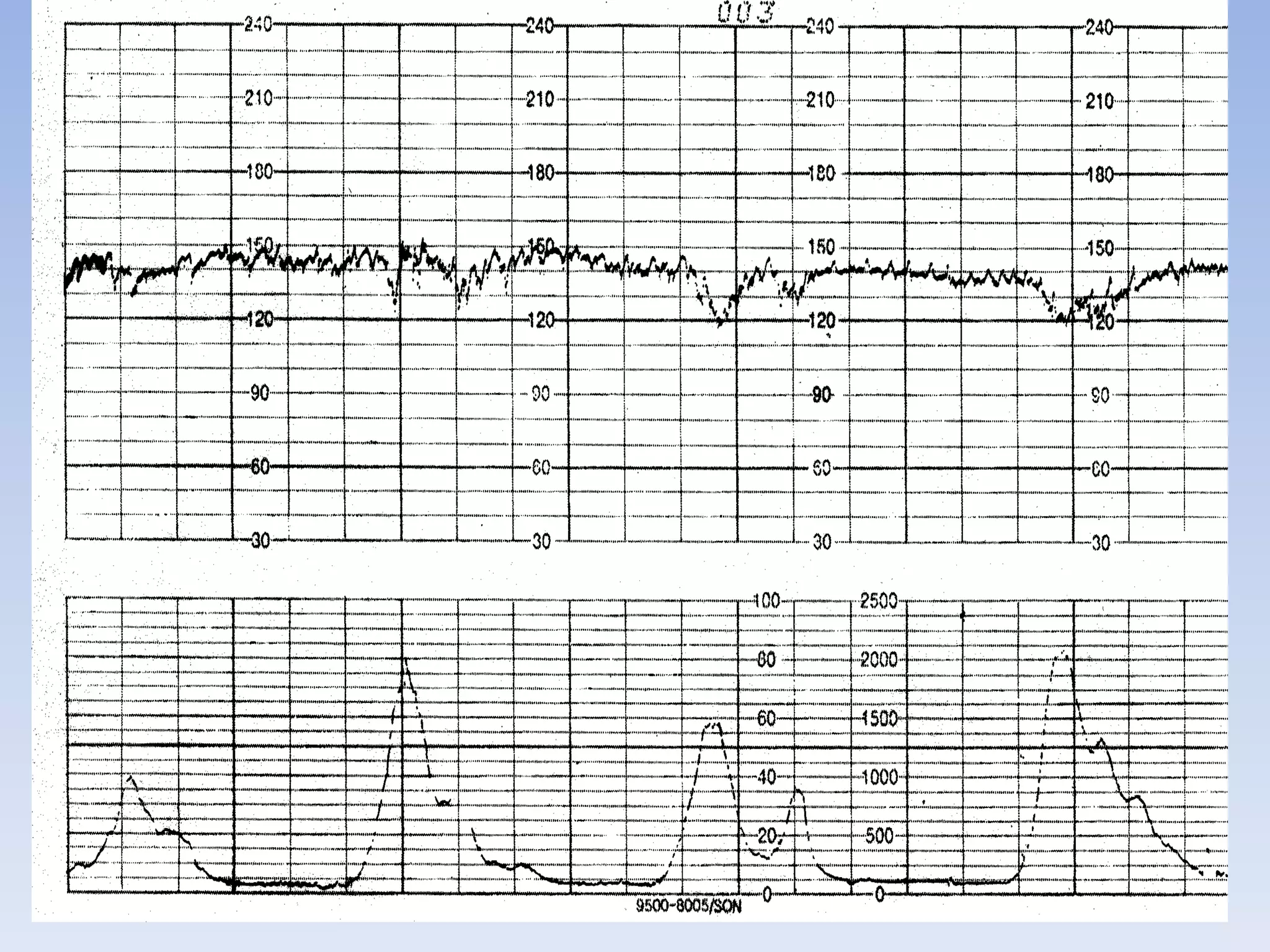
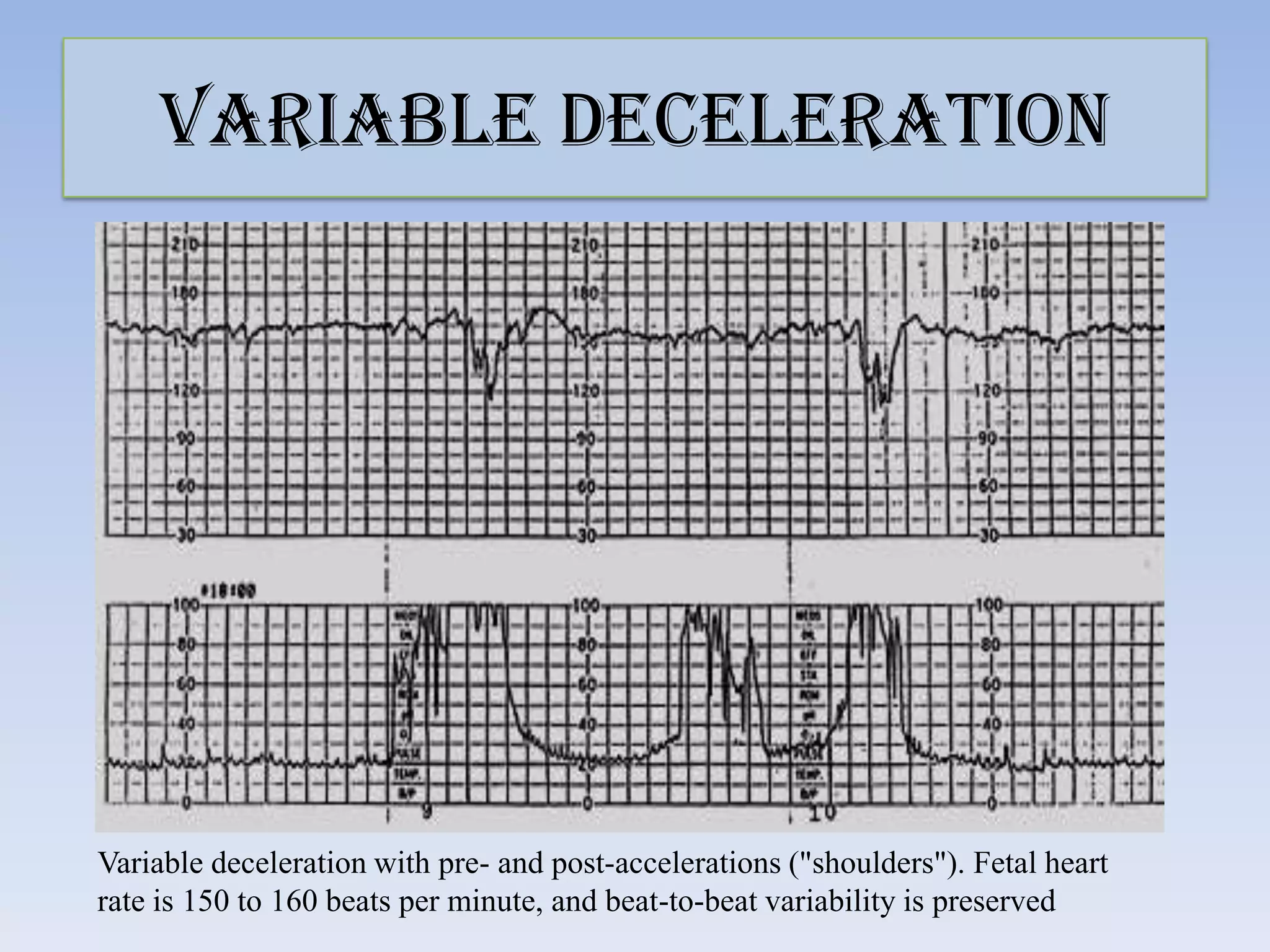
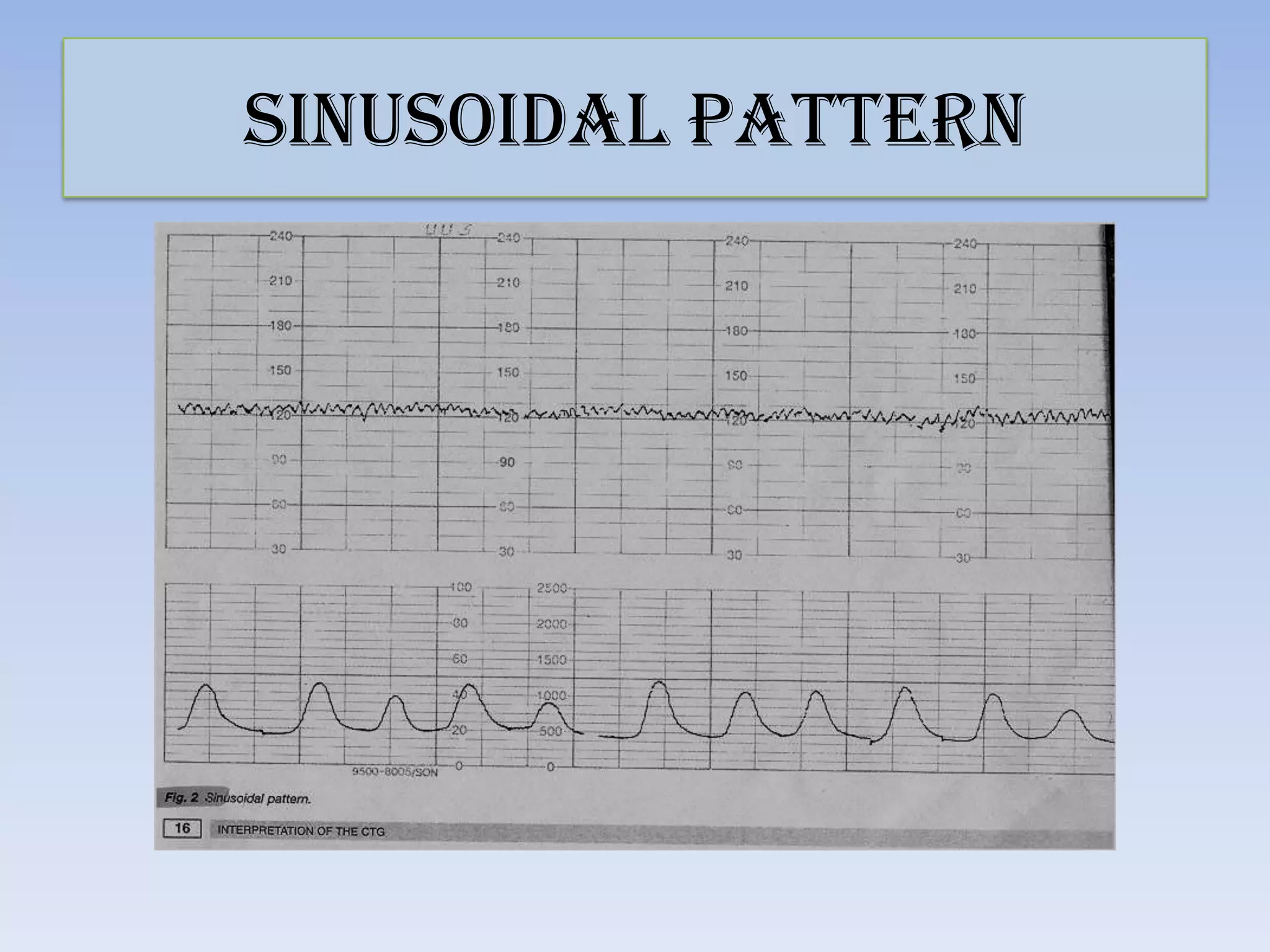
This document provides guidance on interpreting cardiotocography (CTG) readings during labor and delivery. It discusses how to prepare for and perform CTG monitoring, including setting up the machine, positioning the patient, and differentiating the maternal and fetal heart rates. It then describes how to interpret various features of the CTG tracing such as the baseline fetal heart rate, variability, accelerations, decelerations, and overall patterns. Recommendations are provided on the actions to take based on whether the CTG reading is normal, suspicious, or pathological.