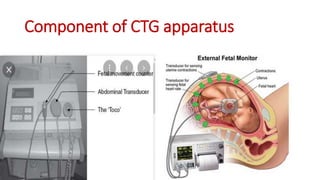
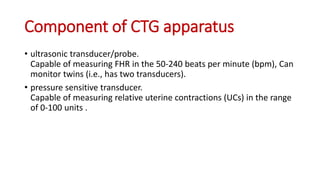
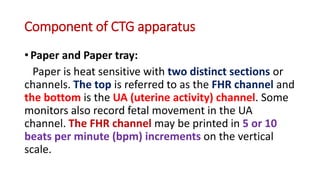
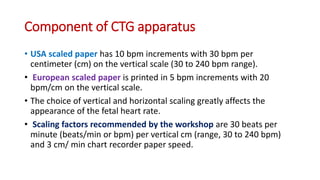
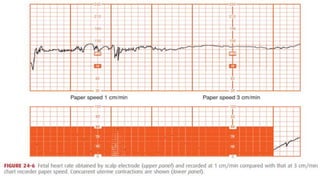
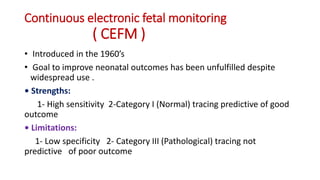
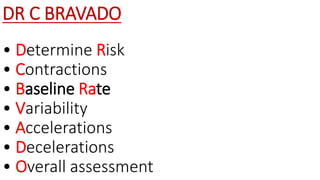
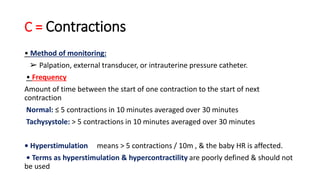
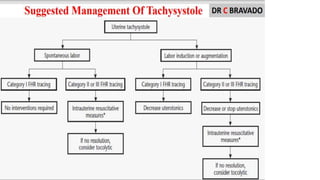
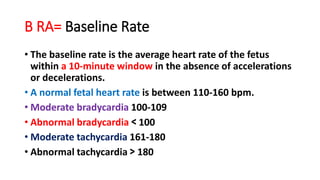
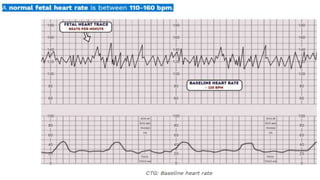
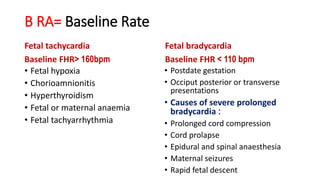
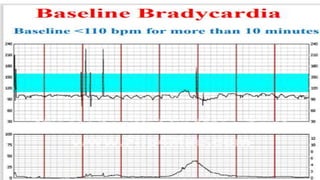
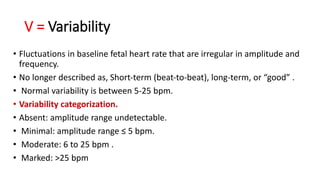
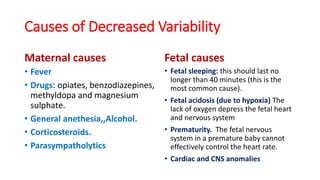
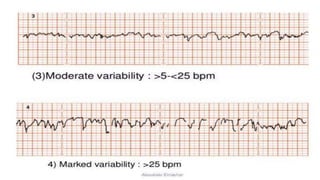
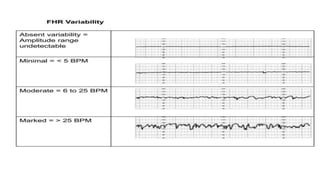
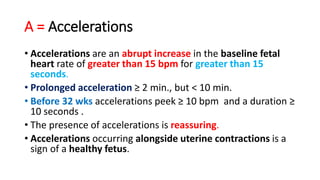
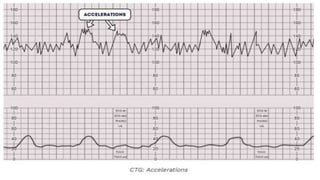
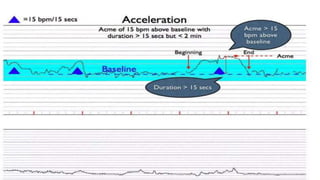
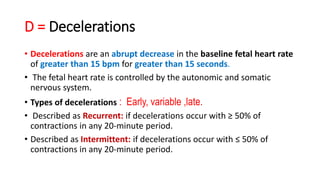
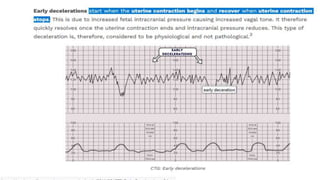
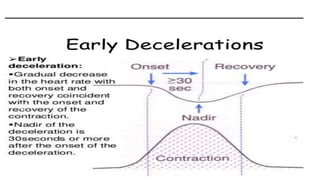
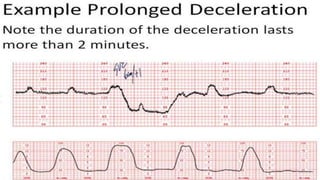
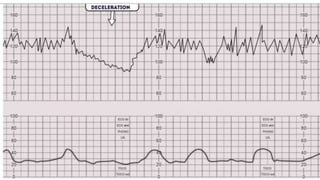
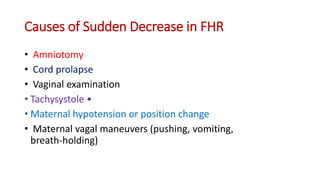
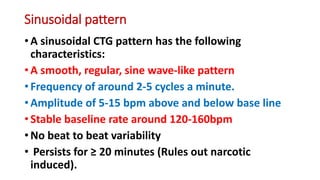
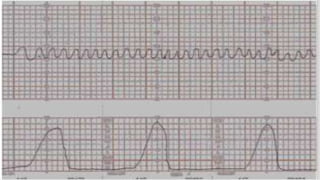
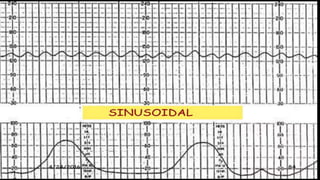
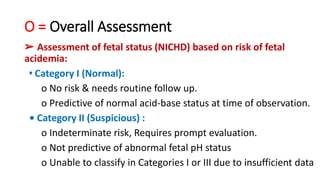
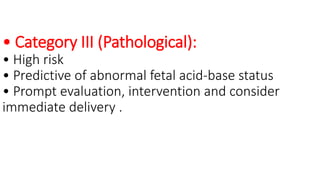
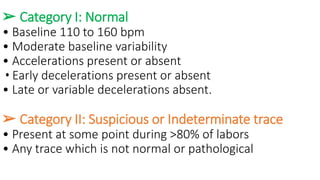
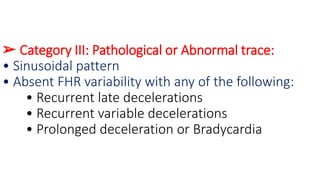
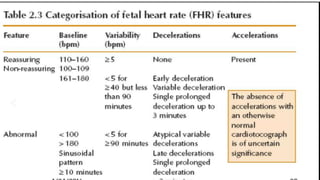
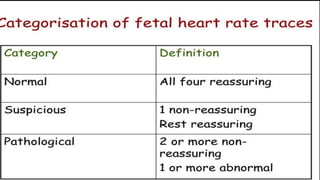
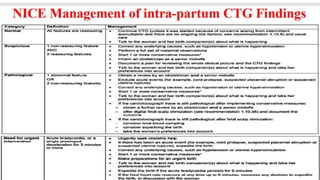
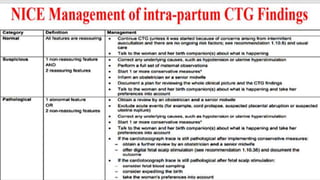
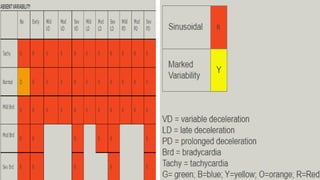
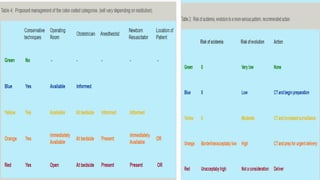
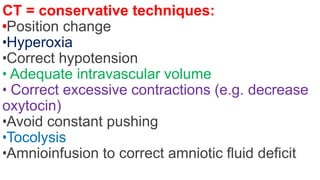
This document provides information on how to read and interpret a cardiotocography (CTG), which is a graphic recording of the fetal heart rate and uterine contractions. It discusses the components of a CTG apparatus and how to prepare for a CTG. It describes how to assess various characteristics of a CTG tracing using the DR C BRAVADO method, including determining risk, contractions, baseline rate, variability, accelerations, decelerations, and providing an overall assessment. It also discusses conservative techniques that can be used in response to certain CTG tracings and mentions tele-CTG as a potential cost-effective alternative.