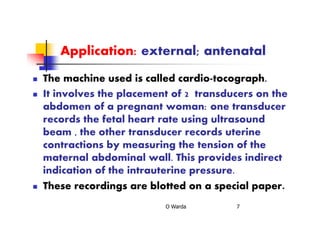
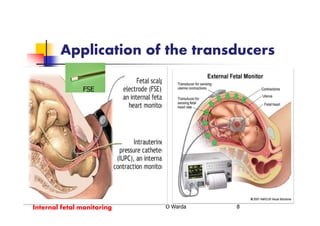
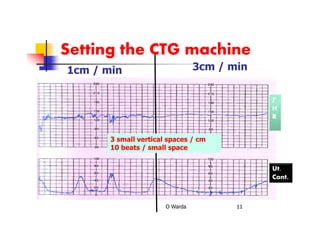
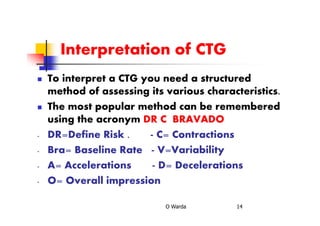
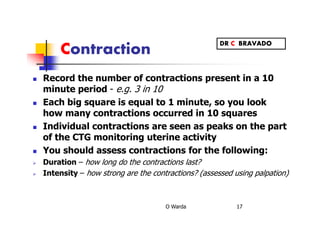
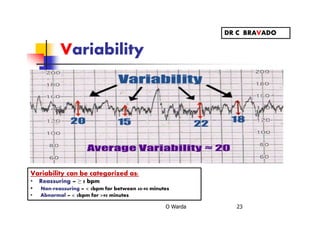
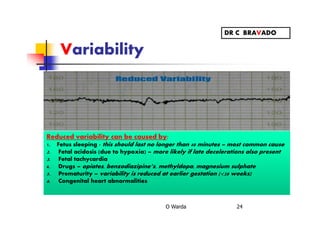
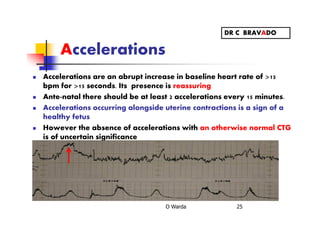
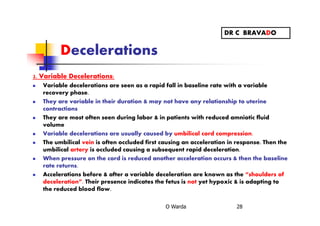
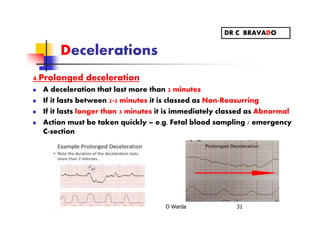
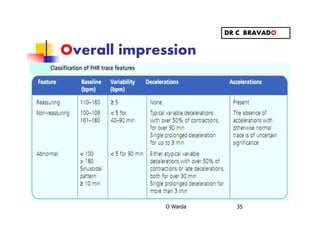
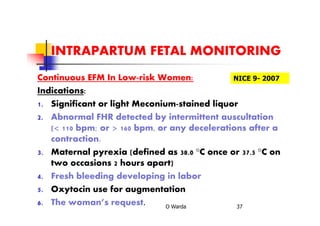
This document discusses cardiotocography (CTG), which monitors fetal heart rate and uterine contractions during pregnancy. CTG is performed in the third trimester using external transducers on the abdomen or internal monitors during labor. Recordings are interpreted using the DR C BRAVADO method: defining risk, assessing contractions, baseline rate, variability, accelerations, decelerations, and the overall impression. Abnormal findings like late decelerations or a sinusoidal pattern indicate fetal distress requiring emergency measures.