This document discusses trigeminal neuralgia, a neuropathic pain condition that causes severe, sporadic facial pain. It provides information on:
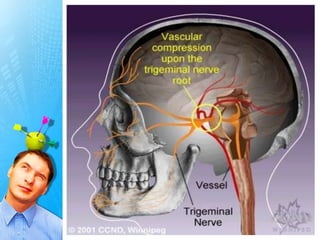
1) The etiology, including neurovascular compression as a common cause.
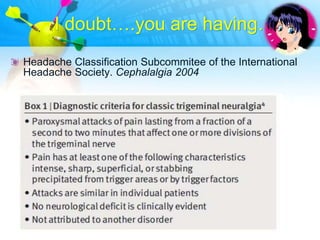
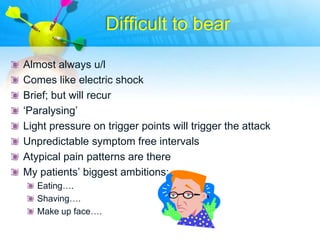
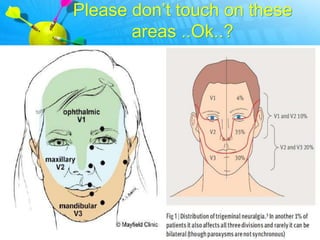
2) Symptoms like brief, severe facial pain that may be triggered by light touch.
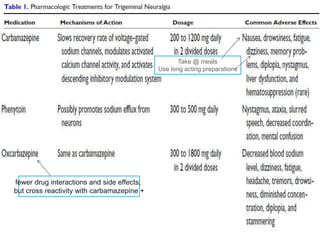
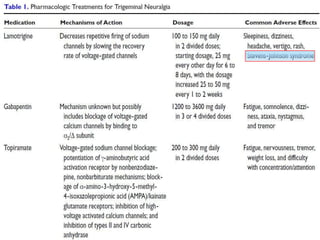
3) Treatment options like carbamazepine, microvascular decompression surgery, and percutaneous radiofrequency thermocoagulation of the gasserian ganglion.
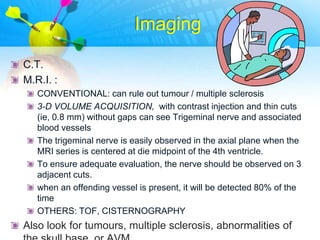
4) Imaging techniques like MRI that can identify compressive vascular structures.
![Peculiar neuropathic pain
not accompanied by sensory deficit
Can be cured by a small nerve or root lesion
Cause ? Now… sound hypothesis of neurovascular conflict
(NVC) [ Are we still hearing sounds of conflict? ]
tic douloureux = since painful brief muscle spasms](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-3-320.jpg)
![EPIDEMIOLOGY
3-5/ one lac; 52- 69 years most common
More recent estimates suggest the prevalence is
approximately 1.5 cases per 10,000 population, with an
incidence of approximately 15,000 cases per year
Multiple sclerosis is found to be a risk factor; ?HTN
I‟m also having..[youngest 12m]
3.4/lac 5.9/lac](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-4-320.jpg)
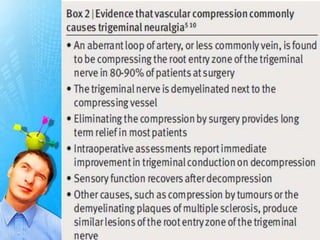
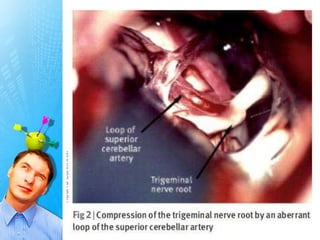
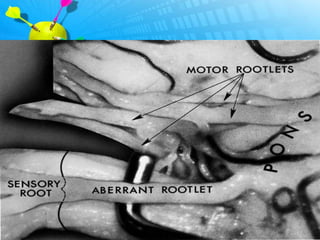
![Painful and annoying
conflict…
In 85%, no structural lesion is seen
Classic [idiopathic] form: “Neurovascular conflict” i.e.
vascular compression of nerve most commonly @ its entry
into pons [REZ]
Significant NVC= an artery (not a vein), crossing (not
parallel to) the nerve and provoking displacement/grooving
of it (Casselman,2000)](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-19-320.jpg)
![Amplifying….
compression results in focal trigeminal nerve demyelination
leads to ephaptic transmission [action potentials jump from
one fiber to another]
A lack of inhibitory inputs from large myelinated nerve fibers
plays a role.
a reentry mechanism causes an amplification of sensory
inputs](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-20-320.jpg)
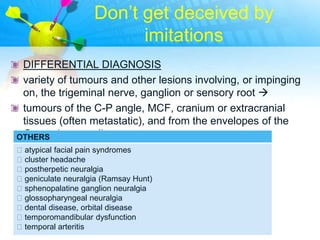
![Two types....One feature..
Trigeminal neuralgia is divided into classic [idiopathic] and
symptomatic types
The classic form includes the cases that are due to a normal
artery present in contact with the nerve, such as the SCA or
even a primitive trigeminal artery
Symptomatic forms can have multiple origins: Aneurysms,
tumors, chronic meningeal inflammation.An abnormal
vascular course of the superior cerebellar artery is often
cited as the cause
Uncommonly, an area of demyelination from multiple
sclerosis may be the precipitant](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-22-320.jpg)
![ETIOLOGY
• compression of nerve root [most common-vascular; rarely
tumor/vein/avm] usually when pain @ v2 / v3, compression
is by SCA ; pain @ v1 by AICA
• Inflammatory causes: multiple sclerosis [in1-5% of patients
with MS;more likely if patient with TN is 20-40ys] ; Damage
to myelin sheath [Myelin gone….signals blend….nerves
may sense light touch as pain!!!!!] ), sarcoidosis, and Lyme
disease neuropathy
• traumatic accidents
• unsuccessful dental work](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-23-320.jpg)


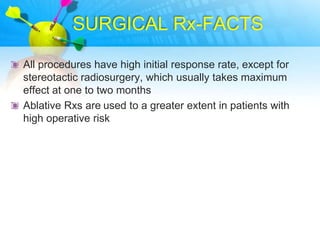
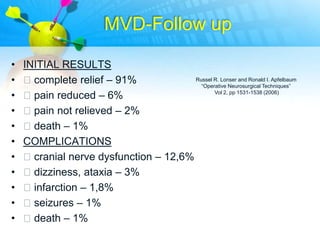
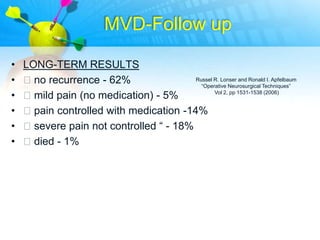
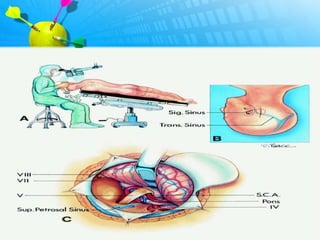
![SURGICAL Rx-FACTS
aimed at either destroying parts of nerve fibers or
decompressing the trigeminal nerve to relieve pain
although surgical treatment may initially be successful,
trigeminal neuralgia may recur retry medical therapy
[because drugs that were previously ineffective may
become effective later]
patients with classic trigeminal neuralgia, evidence of
vascular compression, shorter duration of disease, and no
previous surgery respond better to all treatment options.
In such patients, MVD can be considered the “gold
standard” surgical procedure, and it offers the best long
term cure rates.](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-40-320.jpg)
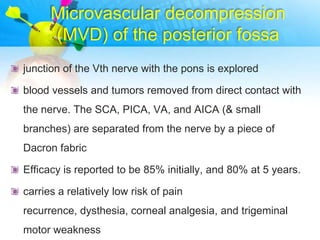
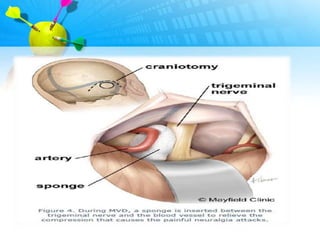
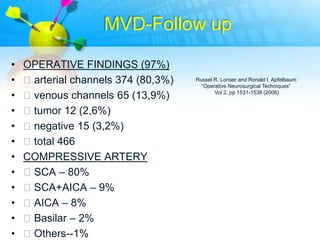
![MVD-Risks
Risks higher in patients who have an ecstatic
(atherosclerotic) and a tortuous vertebrobasilar arterial tree
the risk for perioperative mortality [around 0.4%], serious
morbidity (eg, stroke, hemorrhage, venous occlussion,
M.I.,HCP), permanent hearing loss, and facial palsy is
higher after MVD than after percutaneous procedures.
But ablative procedures are less effective in the long term
and more likely to produce facial numbness and other minor
complications than MVD](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-44-320.jpg)


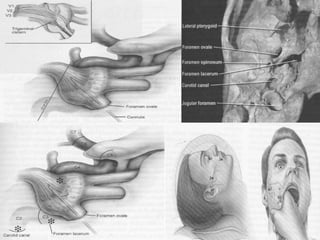
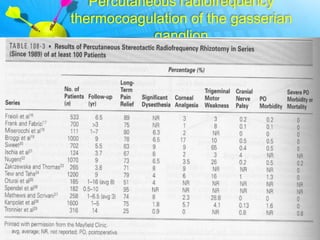
![Percutaneous radiofrequency
thermocoagulation of the gasserian
ganglion
Under fluoroscopic guidance, an insulated needle is passed
through the foramen ovale next to the gasserian ganglion
The initial efficacy ̴ 90%, with 80% patients remaining free of
pain at 1 year and 50% remaining pain free at 5 years.
appropriate for elderly and for those with poor medical
conditions
Risks : numbness, paresthesia, and anesthesia
dolorosa,corneal anesthesia [may develop after lesioning of
the ophthalmic division]](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-55-320.jpg)
![Gamma knife irradiation
[NIHCE,U.K. APPROVED]
radiation is aimed at the proximal nerve and root entry zone
in the pons
gamma knife projects 201 very fine beams of gamma rays
(generated by RA Cobalt) through the skull and brain.
The dose of radiation along any one beam is too small to
effect any change by itself
but when all 201 beams intersect, a very high dose of
radiation can be administered with little or no radiation to
surrounding tissue.41
has been shown to affect abnormal ephaptic transmission
but not normal axonal conduction](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-60-320.jpg)
![References
• Trigeminal neuralgia Pathophysiology and treatment A.
JOFFROY, M. LEVIVIER and N. MASSAGER
• Manish K Singh, MD; Chief Editor: Robert A Egan, MD[2012]
Medscape
• Pain Management: Trigeminal Neuralgia;Meraj N. Siddiqui,
Hospital Physician;Turner White;2003
• BMJ Luke Bennetto, Nikunj K Patel and Geraint Fuller ;2008
• John tew, Mayfield Clinic Update,2012
• review on the causes of trigeminal neuralgia symptomatic to
other diseases florin popovici1, ROMANIAN JOURNAL OF
NEUROLOGY – VOLUME X, NO. 2, 2011](https://image.slidesharecdn.com/tn-121125020735-phpapp01/85/TRIGEMINAL-NEURALGIA-65-320.jpg)