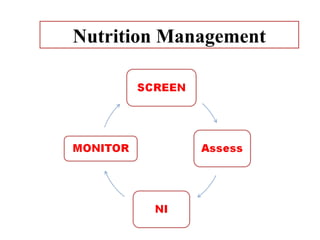
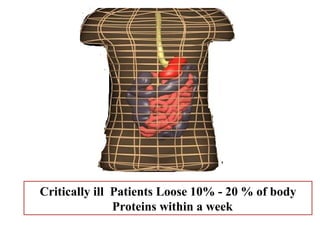
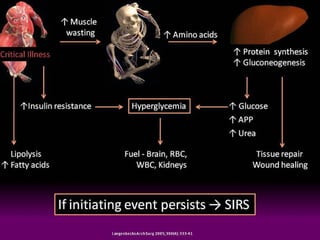
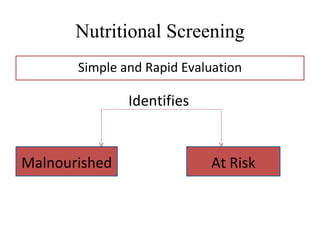
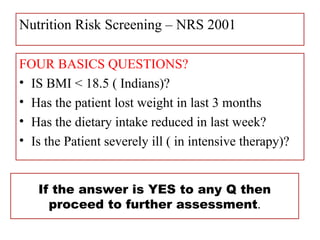
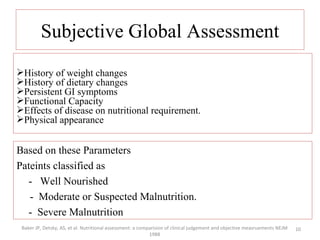
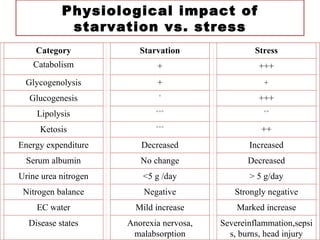
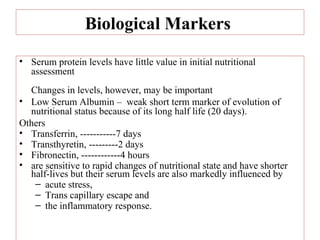
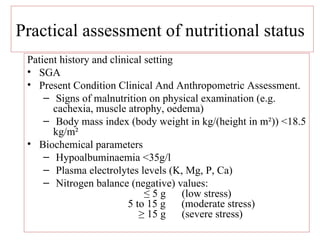
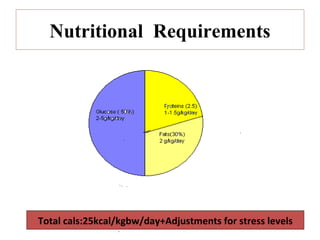
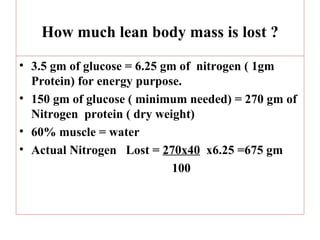
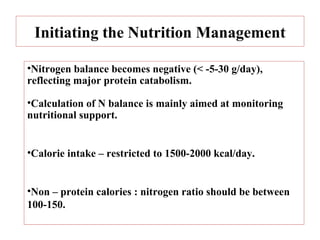
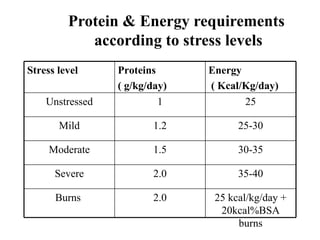
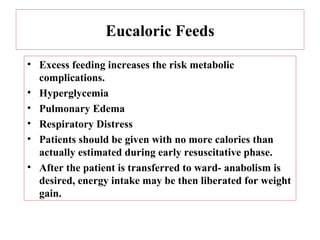
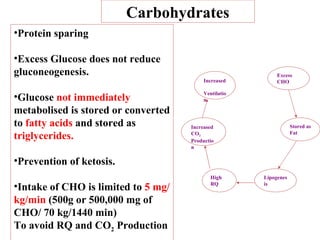
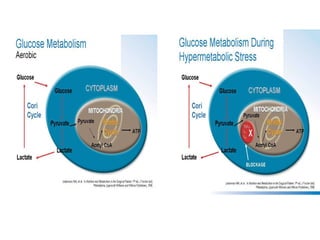
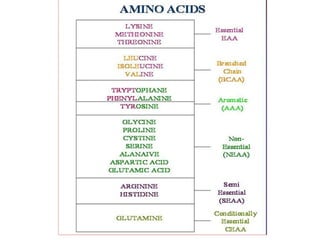
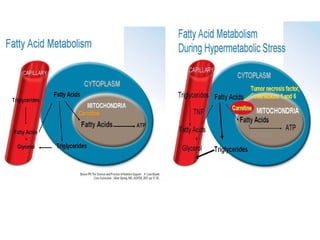
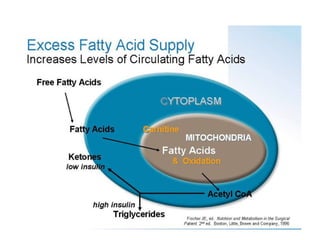
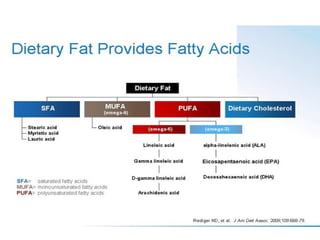
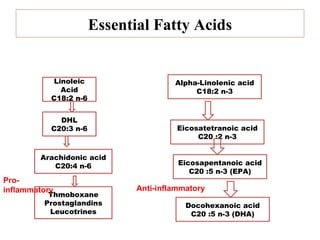
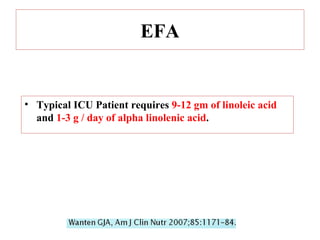
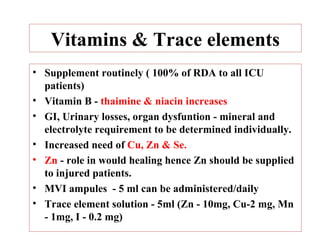
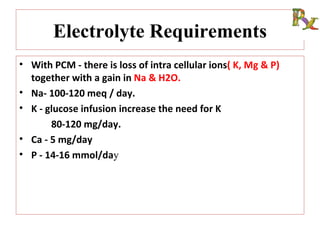
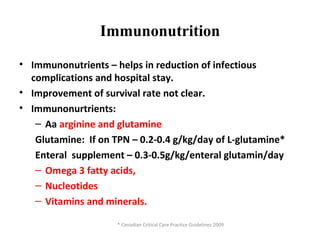
Dr. Geeta Dharmatti has over 15 years of experience as a chief dietician. She has expertise in enteral and parental nutrition. The document discusses guidelines for nutritional management of ICU patients, including the importance of nutritional screening and assessment within 24 hours. It covers methods of assessment including subjective global assessment and biological markers. The document also discusses protein and energy requirements based on stress levels, initiating nutrition support, and macronutrient management including carbohydrates, fats, and essential fatty acids.