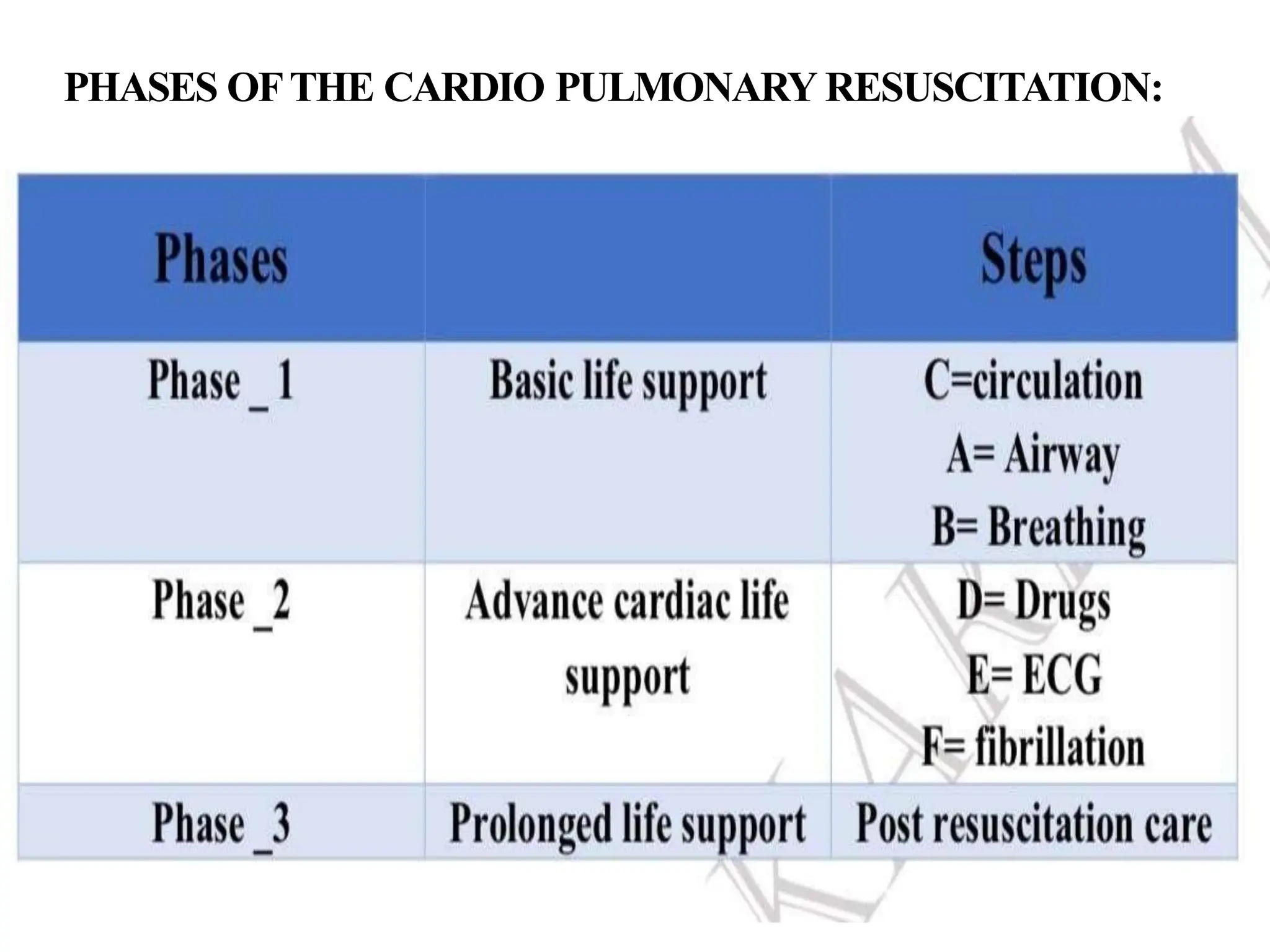
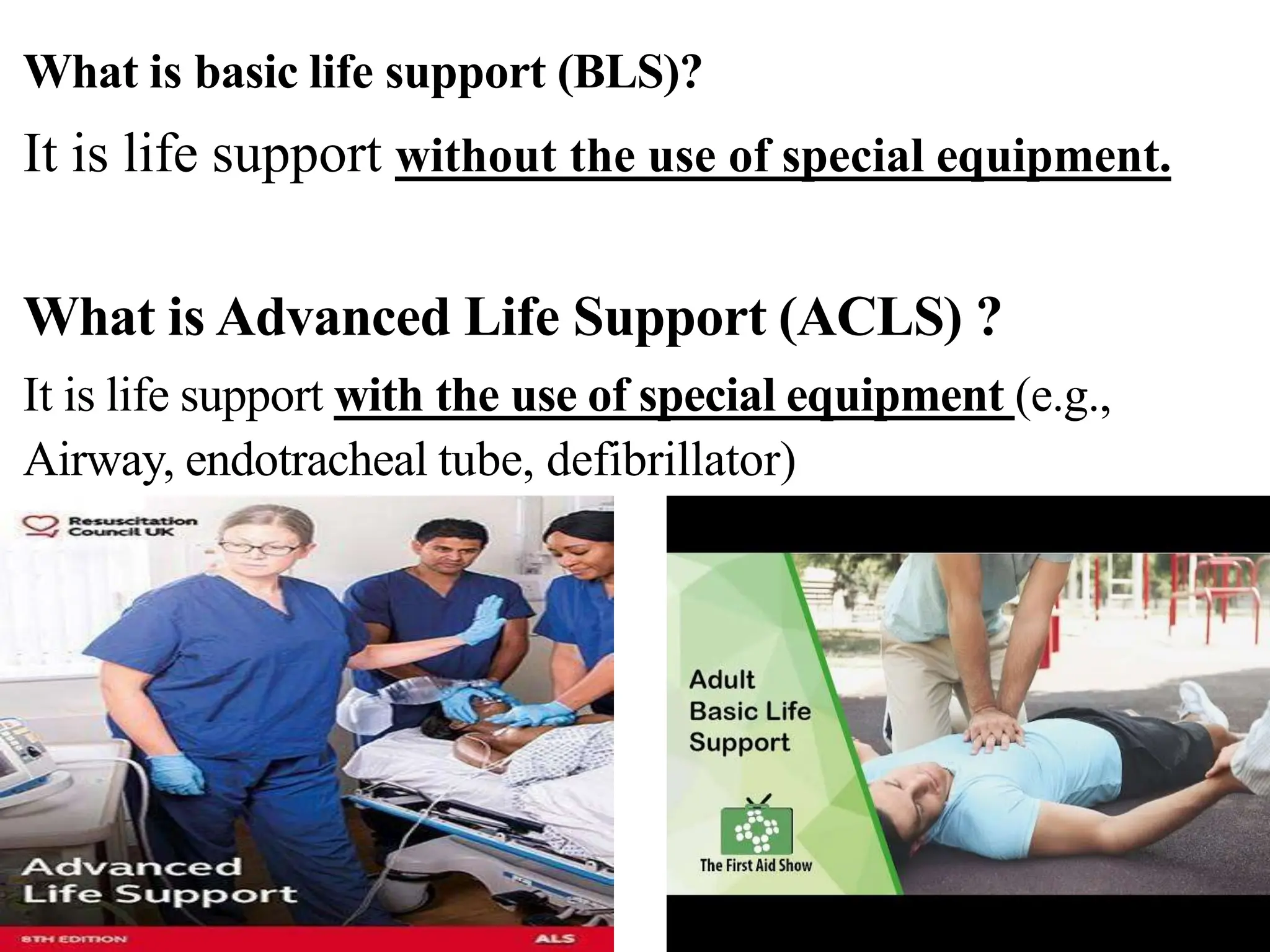
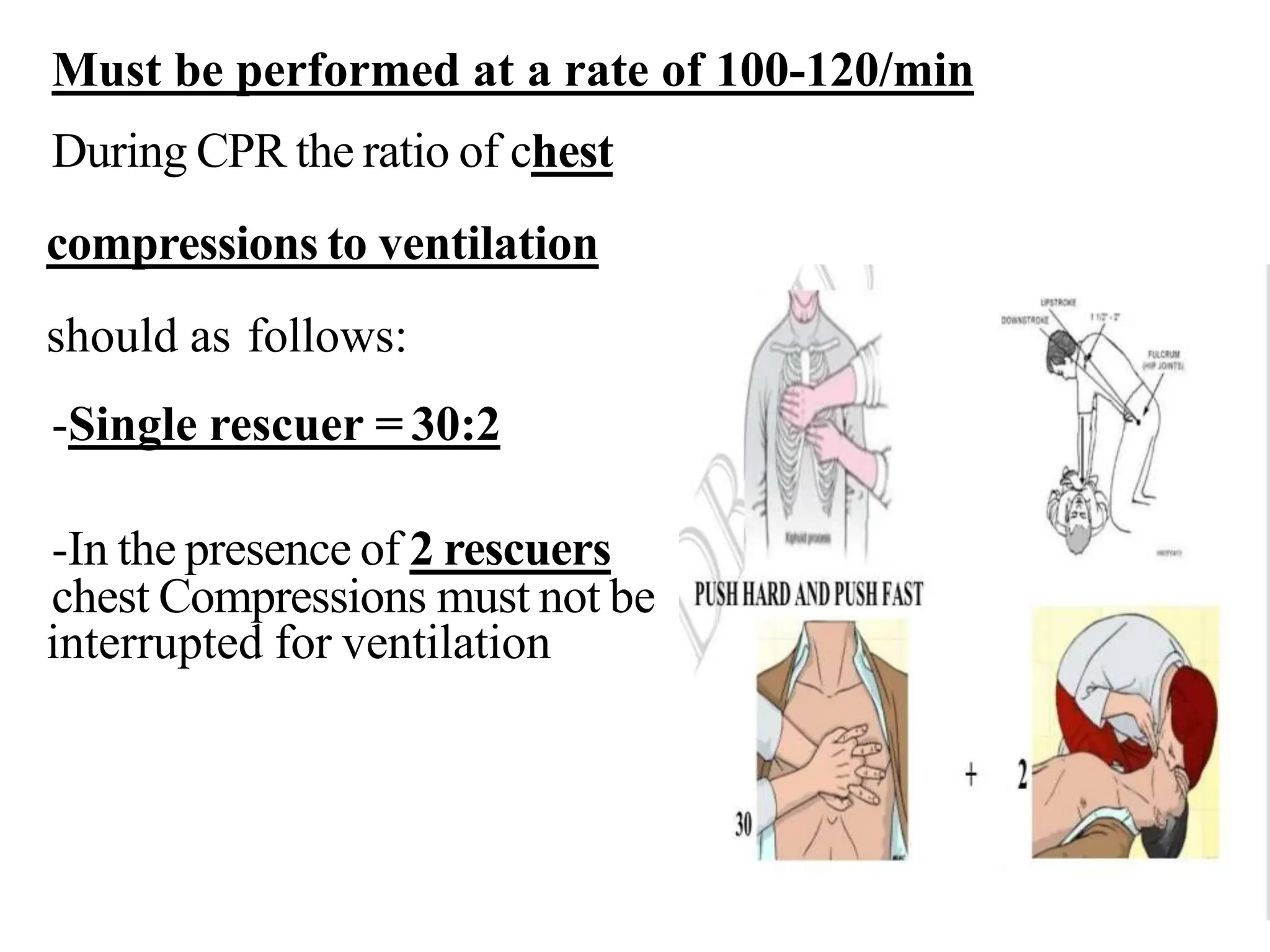
Cardio pulmonary resuscitation (CPR) involves basic life support techniques to maintain oxygenation to the heart, lungs and brain during cardiac or respiratory arrest. It includes chest compressions, opening the airway, and rescue breathing. The goals of CPR are to restore spontaneous circulation and breathing to prevent irreversible brain injury. It consists of early recognition of arrest, high quality chest compressions, airway management, rescue breathing, defibrillation if needed, and administration of drugs to support circulation.