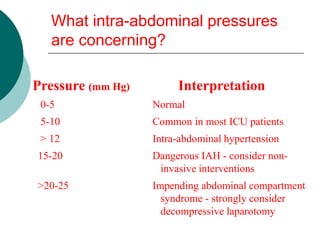
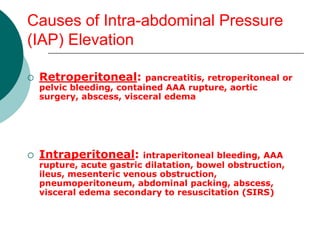
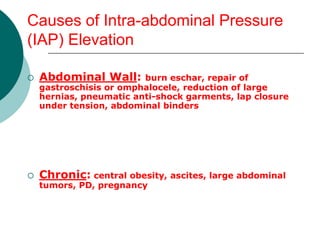
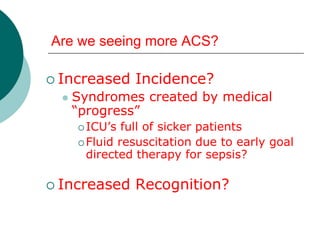
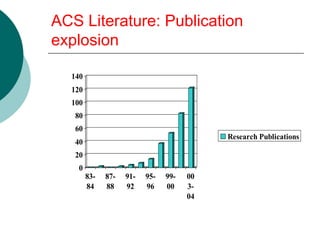
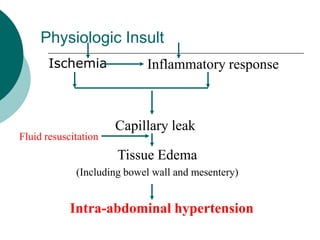
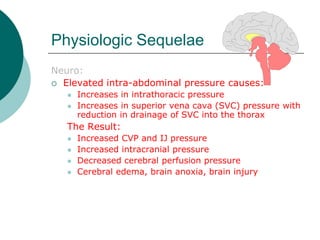
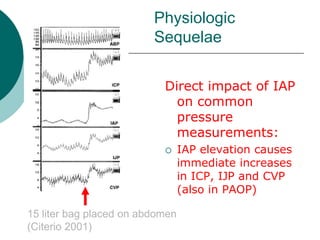
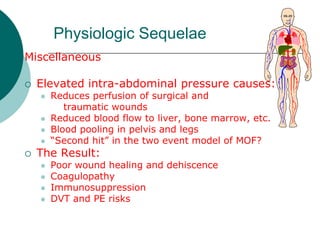
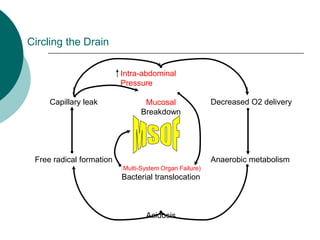
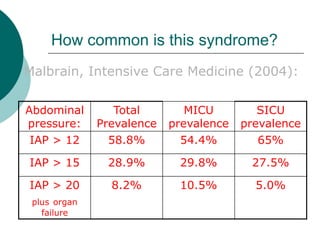
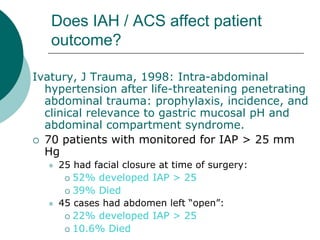
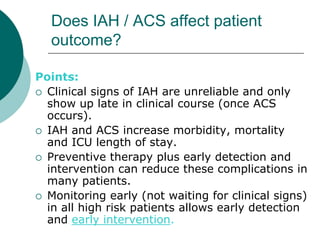
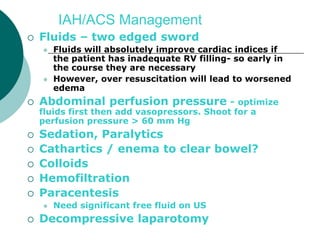
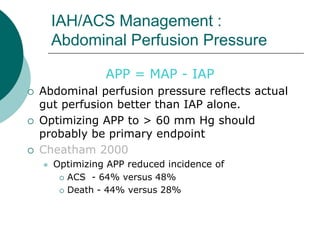
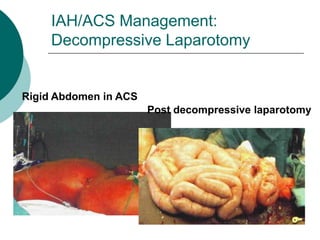
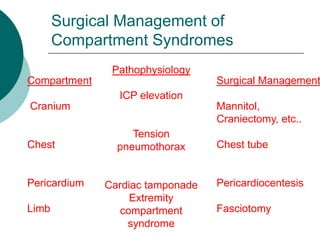
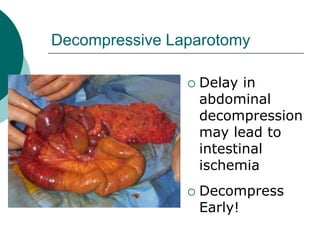
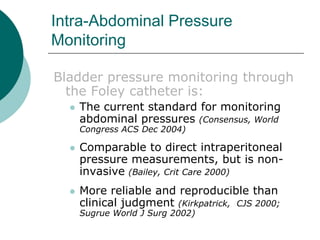
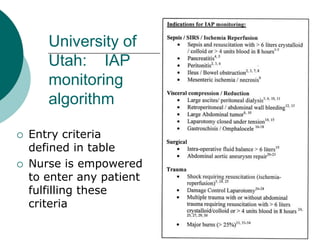
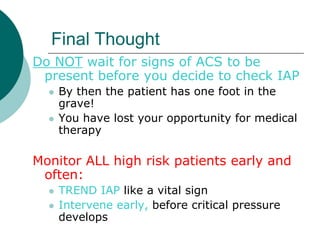
This document discusses abdominal compartment syndrome (ACS), an underrecognized cause of acute kidney injury. It defines ACS as multiple organ dysfunction caused by elevated intra-abdominal pressure. The document outlines various causes of increased intra-abdominal pressure and the physiologic manifestations of ACS, which can impact the cardiac, pulmonary, gastrointestinal, renal and neurological systems. Left untreated, ACS can lead to multi-system organ failure and death. Early detection of increased intra-abdominal pressure and treatment, including decompressive laparotomy if needed, are important to prevent complications of ACS.