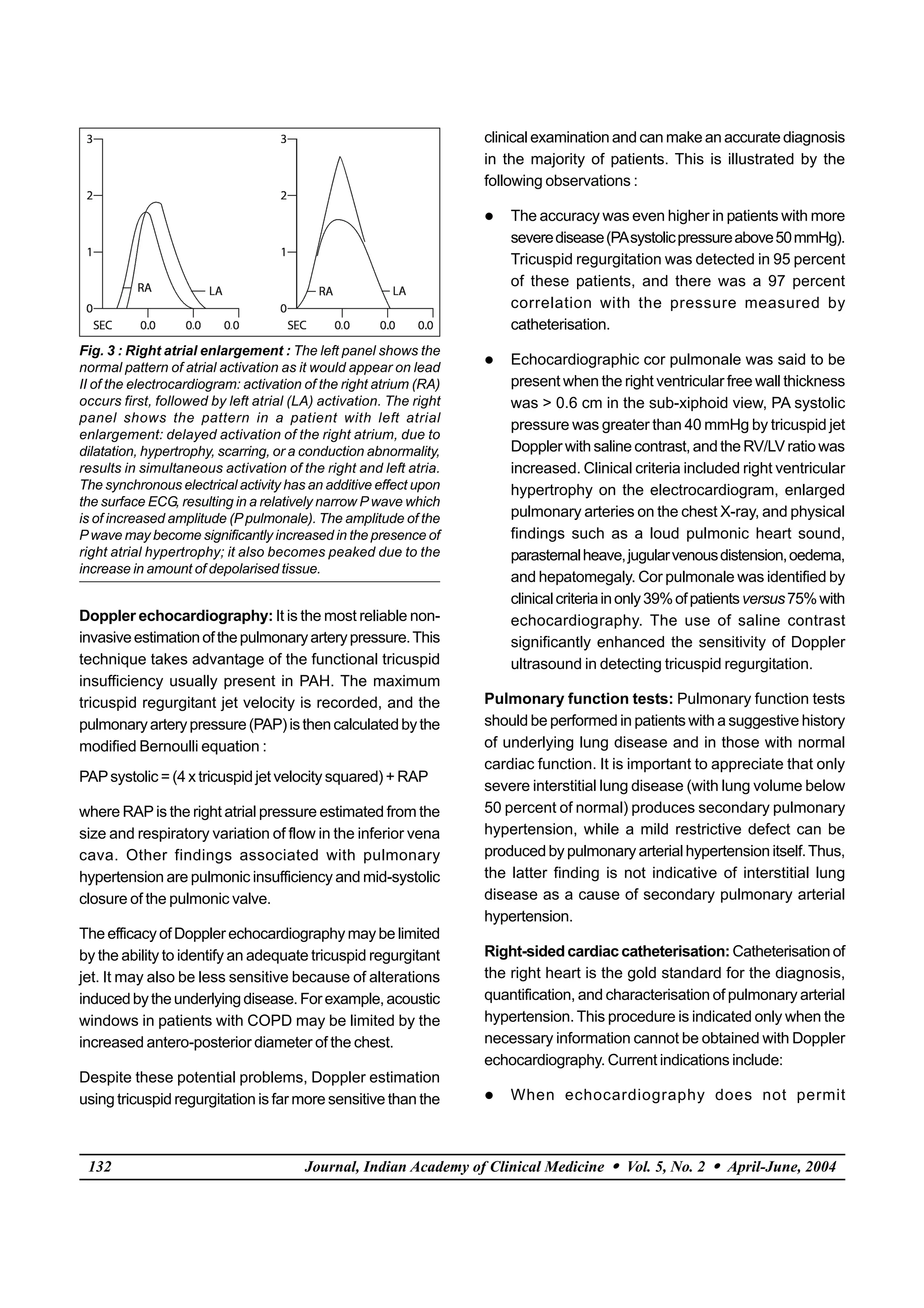
The document discusses cor pulmonale, which is enlargement and failure of the right ventricle caused by lung diseases that increase pulmonary hypertension. The most common cause is chronic obstructive pulmonary disease (COPD). Symptoms are nonspecific but include fatigue and exertional dyspnea. Physical exam may reveal signs of right heart failure like elevated jugular venous pressure. Diagnosis involves chest x-ray, ECG, echocardiogram and cardiac catheterization. Prognosis is poor if pulmonary hypertension and edema develop, with 5-year survival of 30% or less.