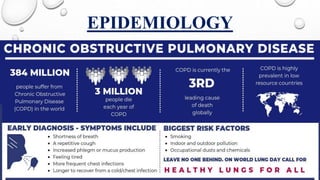
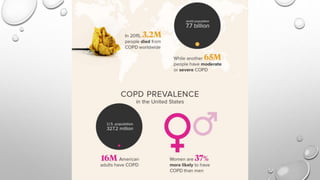
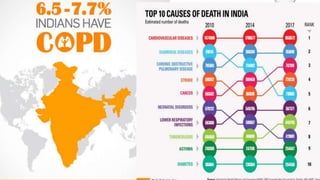
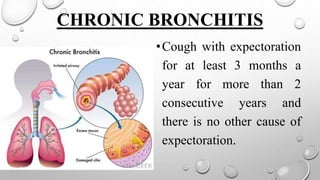
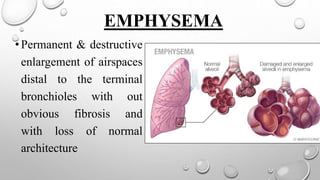
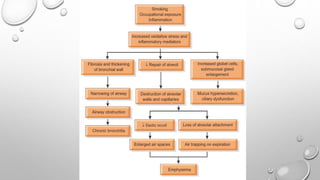
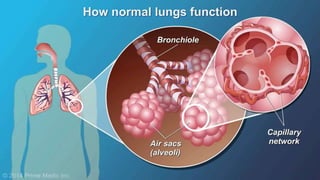
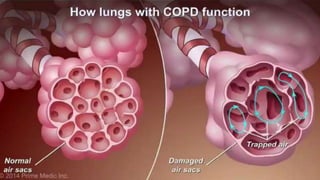
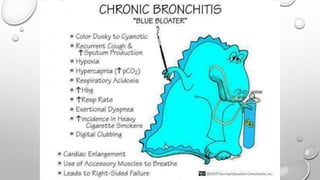
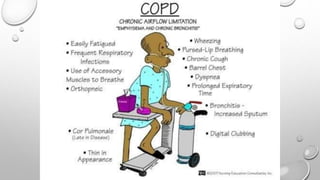
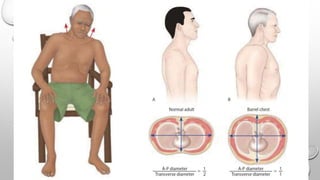
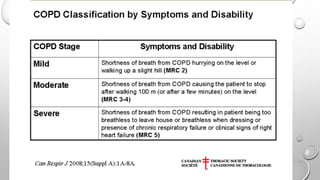
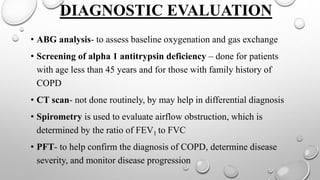
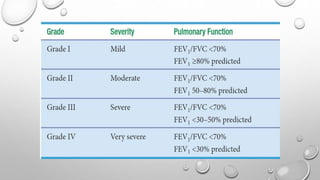
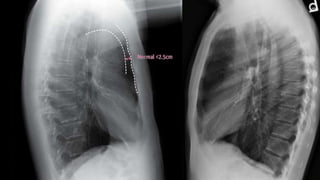
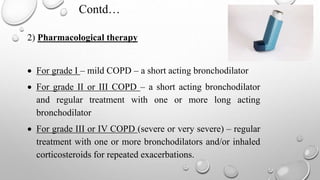
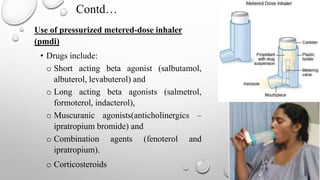
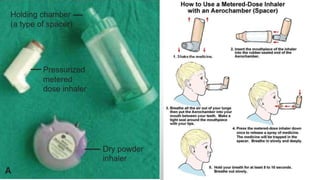
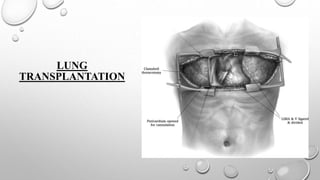
Chronic Obstructive Pulmonary Disease (COPD) is a progressive, preventable respiratory disease characterized by limited airflow and shortness of breath, with causes including chronic bronchitis and emphysema. Diagnosis involves patient history, physical assessment, and various tests like spirometry, with treatment options including pharmacological therapy, oxygen therapy, and surgical management when necessary. Effective management includes regular medication, exercise, vaccination, and lifestyle modifications to improve quality of life.