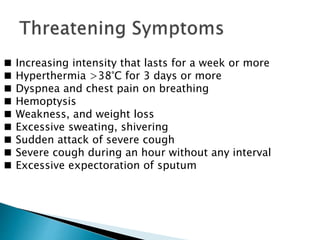
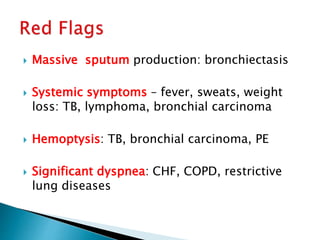
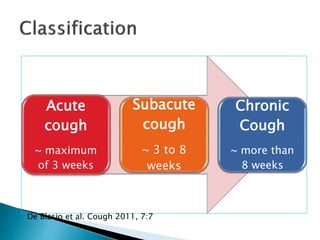
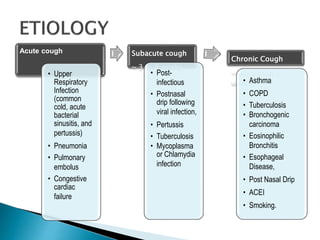
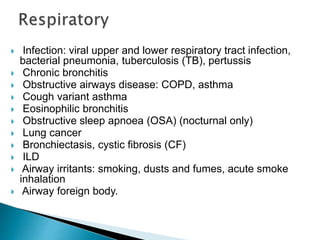
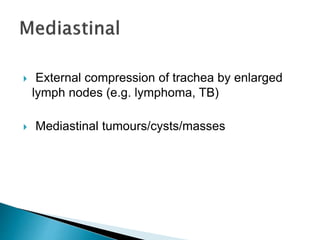
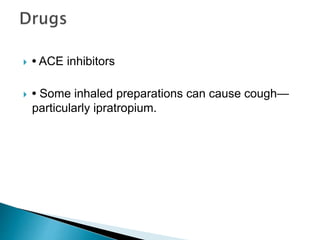
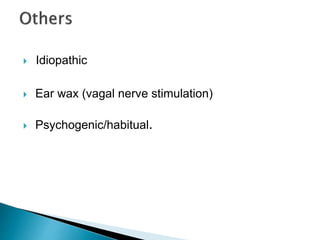
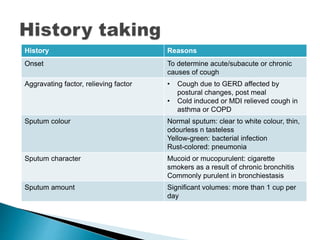
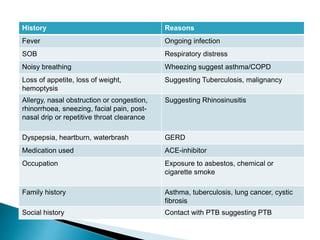
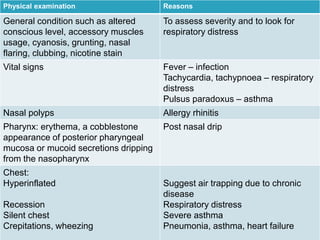
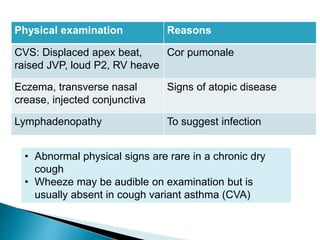
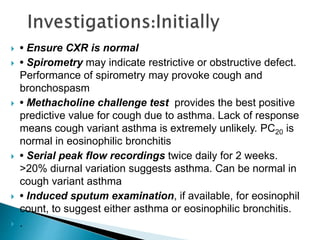
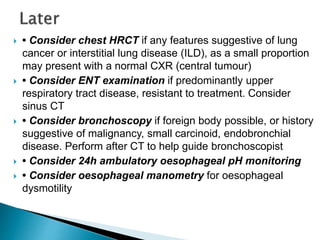
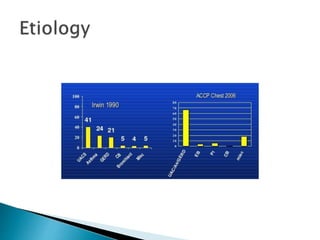
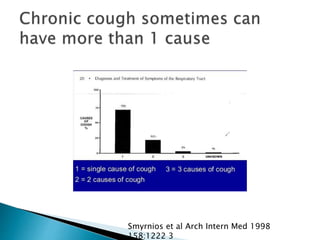
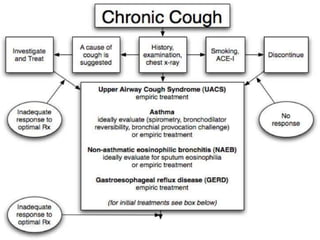
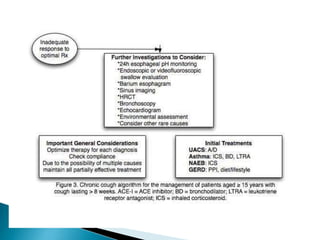
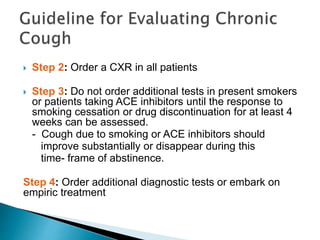
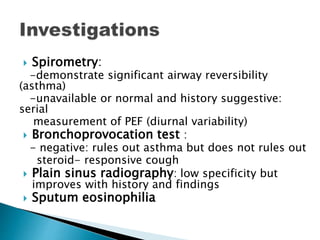
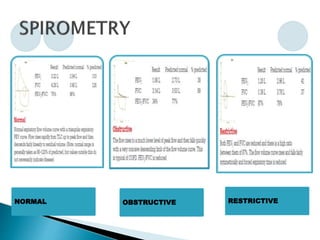
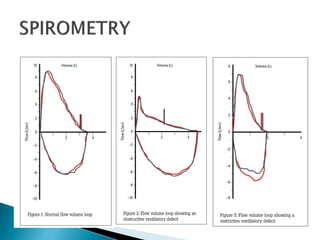
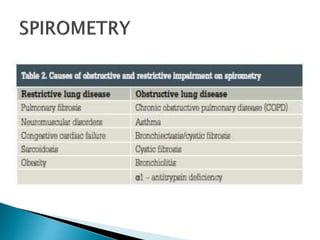
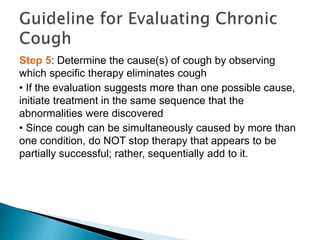
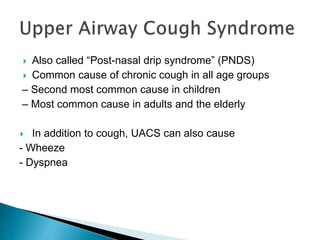
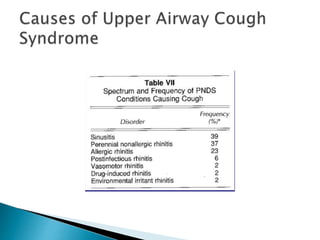
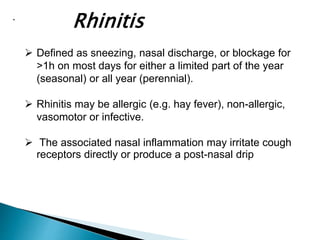
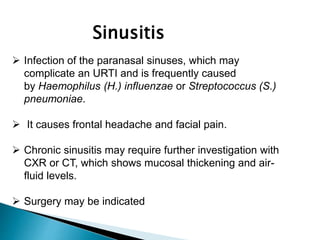
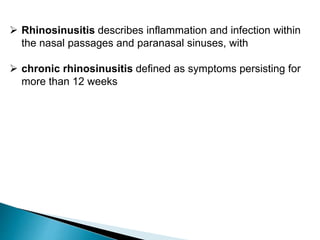
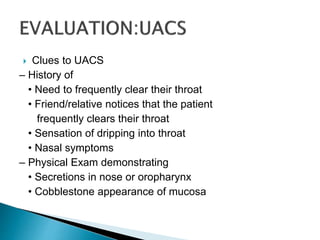
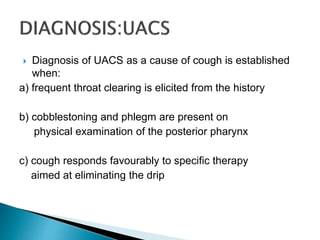
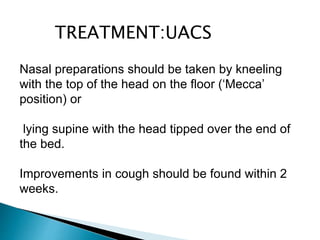
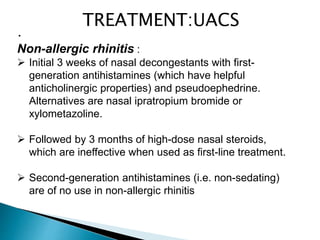
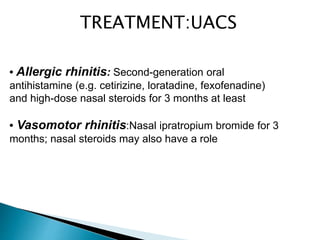
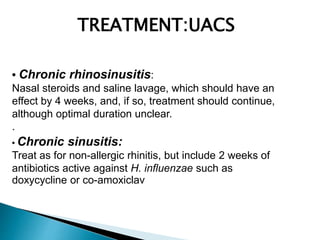
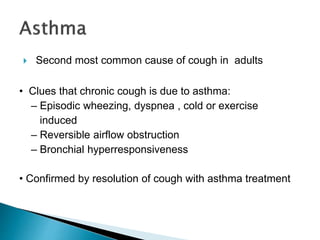
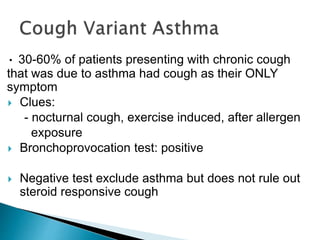
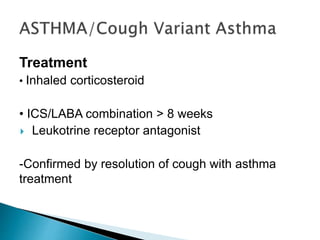
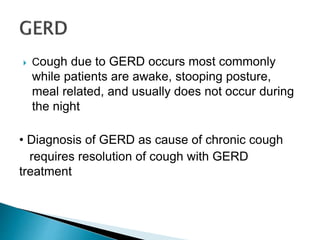
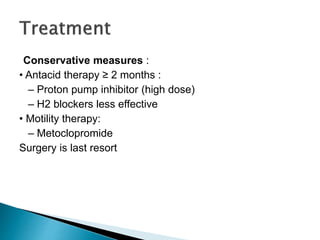
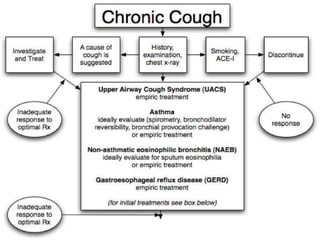
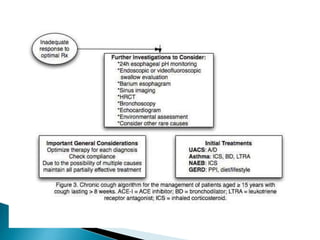
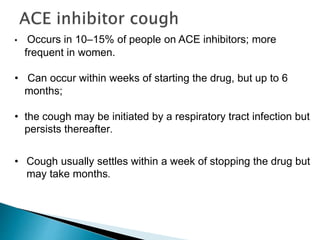
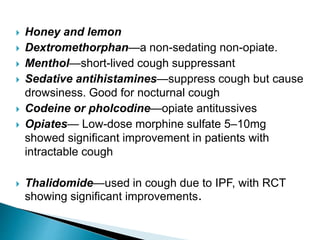
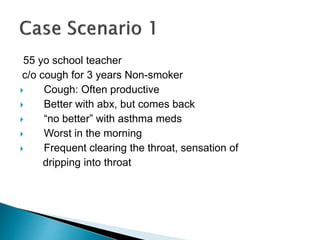
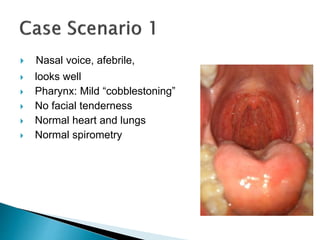
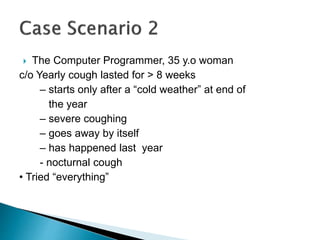
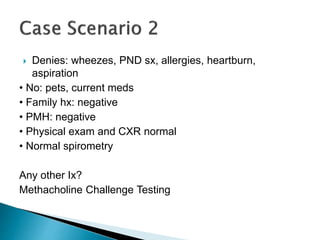
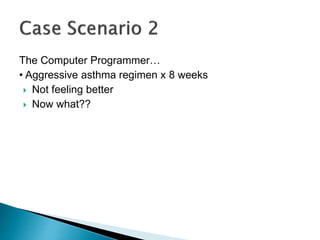
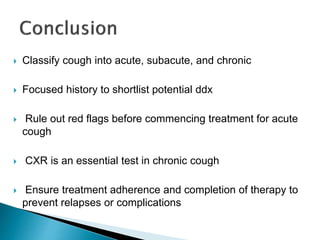
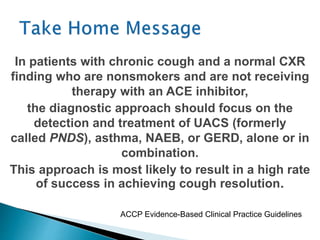
This document discusses cough and its evaluation and management. It defines cough as a protective reflex that clears secretions from the airways. It notes that cough can be acute, subacute, or chronic depending on duration. Common causes include infection, asthma, chronic bronchitis, and gastroesophageal reflux disease. A thorough history, physical exam, and initial tests like chest x-ray are important for evaluating cough. Further tests may be needed to identify specific causes and guide treatment. Upper airway cough syndrome is a common cause of chronic cough.