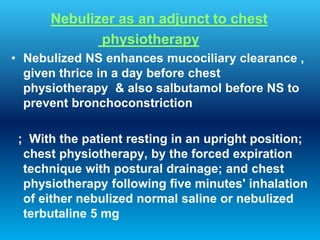
This document provides an overview of aerosol therapy. It discusses that aerosols are suspensions of fine liquid or solid particles in a gas, and that only 10% of drugs are deposited in the lungs. It describes different aerosol delivery systems including metered dose inhalers (MDIs), dry powder inhalers (DPIs), and nebulizers. MDIs are most widely used but have disadvantages like requiring coordination. Spacers can help with MDI use. DPIs do not require coordination but need high inspiratory flow. Nebulizers can deliver high doses and combinations of drugs and are useful for certain patients. The document outlines factors influencing aerosol deposition and characteristics of therapeutic