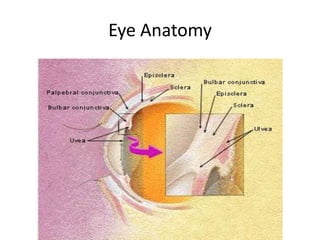
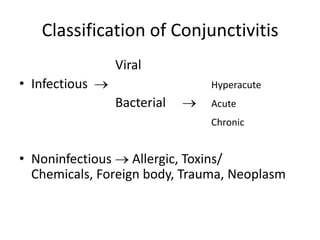
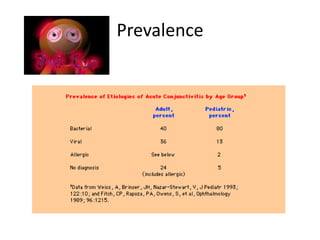
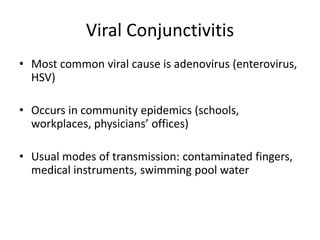
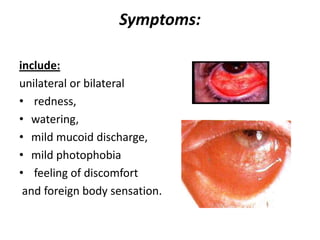
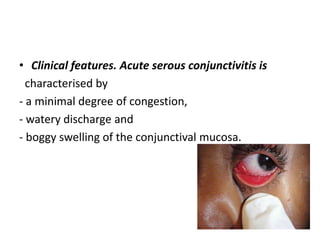
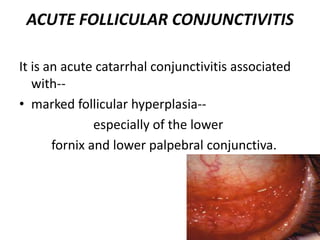
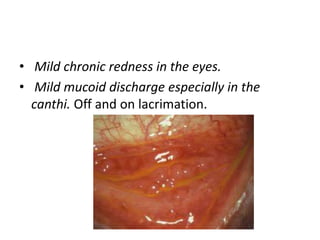
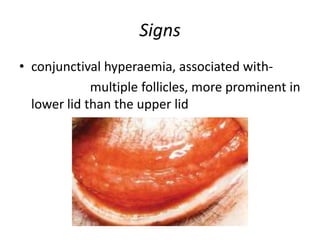
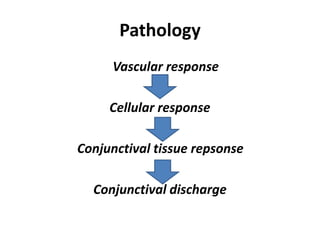
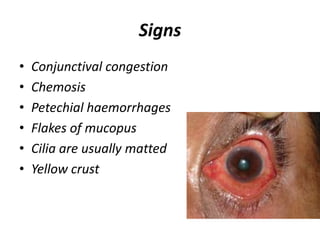
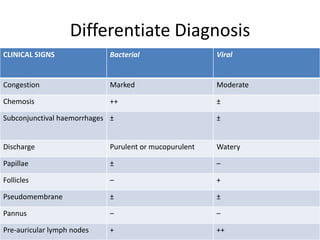
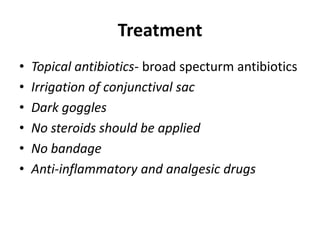
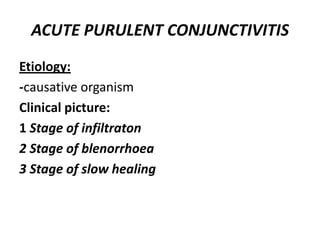
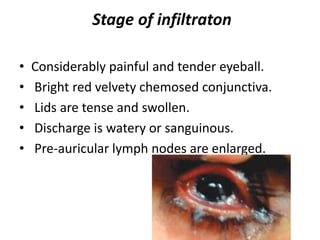
The document provides a detailed overview of conjunctivitis, including its definitions, classifications, and causes, with a focus on viral and bacterial forms. It describes the clinical presentations, symptoms, and treatments for various types of conjunctivitis such as acute serous, hemorrhagic, and follicular conjunctivitis, as well as bacterial forms like mucopurulent and purulent conjunctivitis. Additionally, it covers specific cases such as ophthalmia neonatorum and highlights the importance of prophylaxis and treatment strategies to prevent secondary infections.