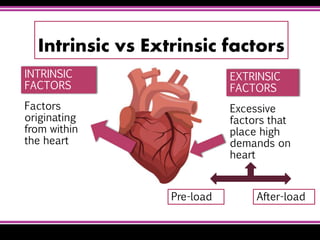
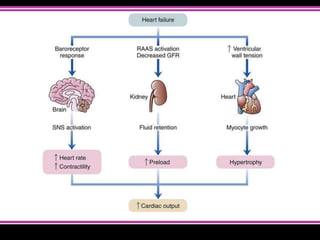
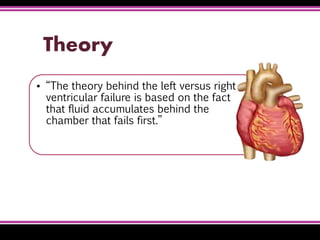
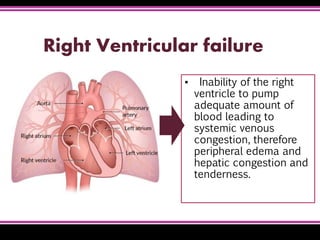
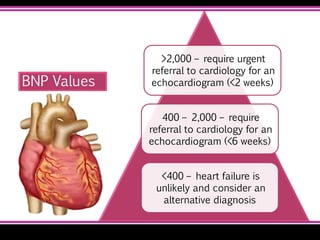
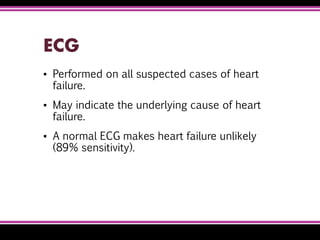
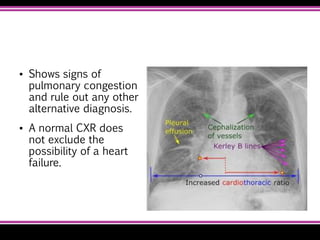
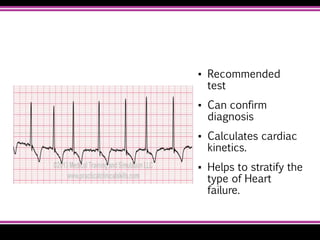
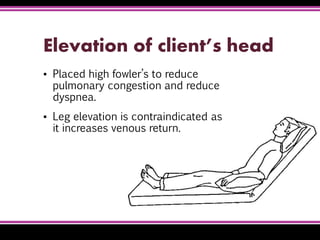
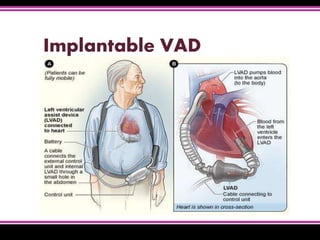
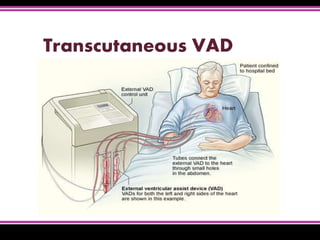
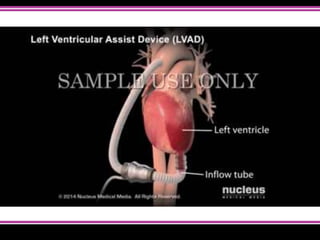
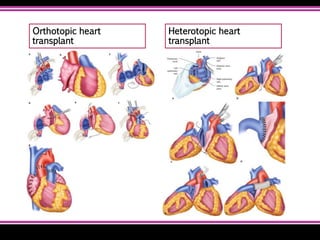
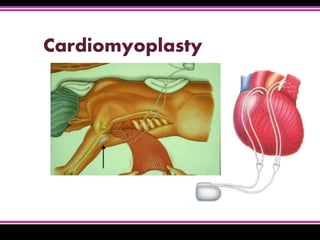
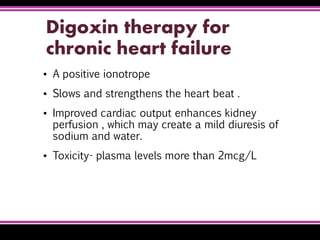
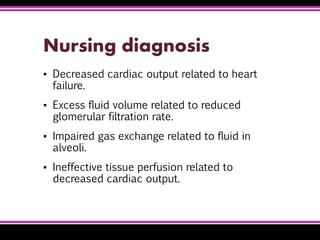
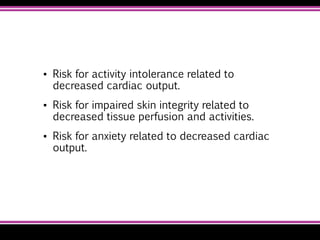
Heart failure is a condition where the heart cannot pump enough blood to meet the body's needs. It can be caused by conditions that weaken the heart muscles. Symptoms depend on whether the left or right side of the heart is affected but may include shortness of breath, fatigue, swelling of legs/abdomen. Diagnosis involves checking for elevated BNP, abnormalities on ECG/CXR, and reduced ejection fraction on echocardiogram. Treatment focuses on reducing pre/afterload, increasing cardiac output, restricting fluids/sodium, and controlling symptoms. For severe cases, devices, transplantation or specialized surgeries may be considered.