The document discusses various types of glomerular and tubulointerstitial diseases:
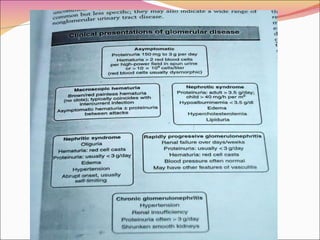
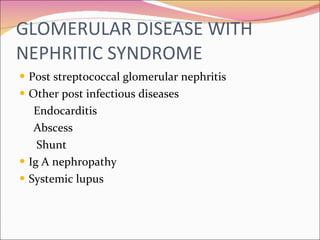
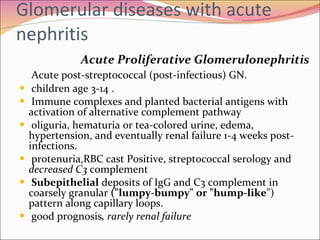
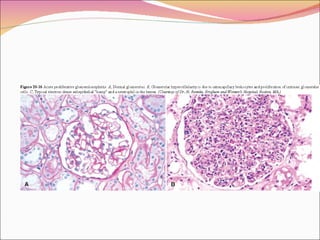
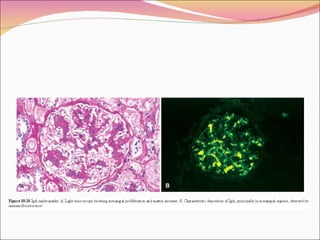
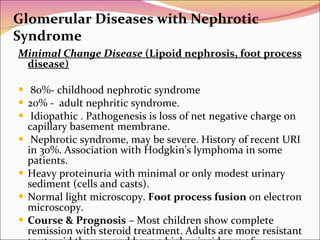
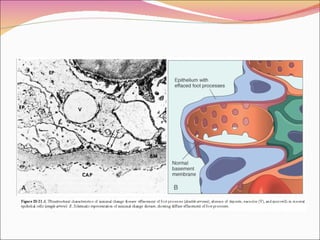
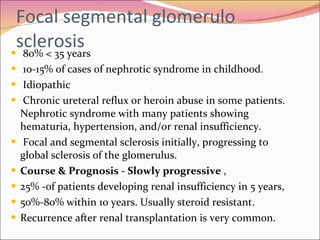
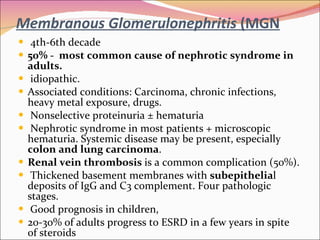
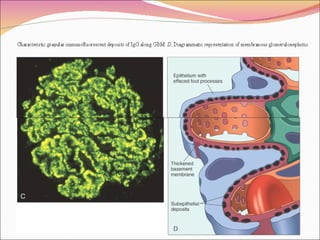
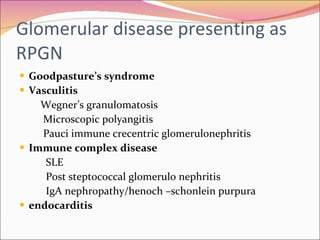
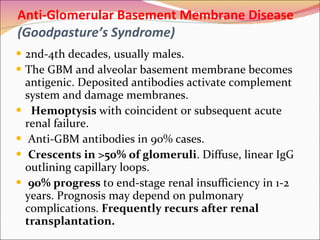
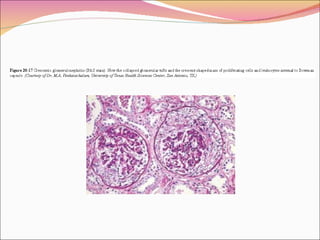
1. Glomerular diseases are caused by damage to the glomerulus and can manifest as nephritic syndrome, nephrotic syndrome, or hematuria. Common glomerular diseases include minimal change disease, membranous nephropathy, and focal segmental glomerulosclerosis.
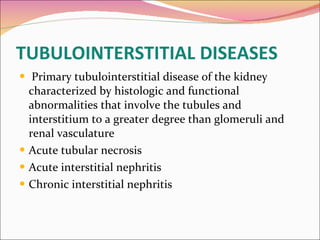
2. Tubulointerstitial diseases involve damage to the renal tubules and interstitium. Acute interstitial nephritis is often caused by drug reactions while chronic interstitial nephritis can result from various insults like drugs, infections, toxins, and inherited conditions.
3
![Pathogenesis of glomerular injury Antibody mediated injury In situ immune complex deposition Fixed intrinsic tissue antigens NC1 domain of collagen type4 antigen [anti GBM-nephritis] Heymann antigen [membranous nephropathy] Mesangial antigens Circulating immune complex deposition Endogenous antigen[DNA,Nuclear proteins,immunoglobulins,igA] Exogenous antigen [infectiousagents,drugs] Cytotoxic antibodies Cell mediated immune injury Activation of alternative complement pathway](https://image.slidesharecdn.com/glomer-101015091823-phpapp02/85/CME-Glomerular-Tubular-Disorders-3-320.jpg)

![G lomerular diseases with primary haematuria IgA Nephropathy (Berger’s Disease ] Most common primary glomerular disease. Mostly adolescents and young adults gross hematuria occurring coincidentally with or immediately following (24-48 hours), a viral upper respiratory infection, flu-like illness, gastrointestinal syndrome episodes of gross hematuria , microscopic hematuria . Focal and segmental glomerular mesangial proliferation, with IgA deposits. Increased serum IgA . Normal C3 complement. Prognosis – Generally benign 20% progress to renal insufficiency in 10 years. recurs after renal transplantation.](https://image.slidesharecdn.com/glomer-101015091823-phpapp02/85/CME-Glomerular-Tubular-Disorders-10-320.jpg)
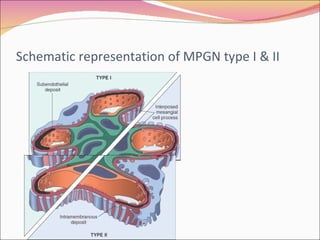
![M embrano proliferative glomerulo nephritis (MPGN) M esangiocapillary glomerulonephritis OR lobar glomerulonephritis 5-30 years Immune complex disease Associated conditions: Chronic infections (especially hepatitis C), cancer, heroin abuse, SLE, etc Usually nephrotic syndrome, less often acute nephritic syndrome. Recent history of URI in many patients. Hypertension and/or renal insufficiency may occur. Decreased serum complement levels. Hepatitis C serology should be obtained Glomerular hypercellularity with capillary basement membrane thickening and splitting [TRAM-TRACKING ]. Subendothelial deposits of C3 complement and sometimes IgG . Prognosis Progressive deterioration of renal function; Many patients develop end-stage renal insufficiency within 10 years.](https://image.slidesharecdn.com/glomer-101015091823-phpapp02/85/CME-Glomerular-Tubular-Disorders-16-320.jpg)
![Renal Amyloid Primary [AL ]amyloidosis – associated with multiple myeloma. Secondary[AA] amyloidosis – chronic infectious diseases (i.e., TB, osteomyelitis, leprosy) and chronic inflammatory diseases (i.e., rheumatoid arthritis, ankylosing spondylitis). Proteinuria, nephrotic syndrome, Hypertension is usual Amyloid deposited first in mesangium, small vessels, and later in glomerular capillary wall. " Apple" green birefringence of vessels and glomeruli when stained with Congo Red and polarized. Prognosis – Usually progresses to renal failure . secondary amyloidosis (e.g. cure of TB), improvement may occur. Renal failure is common cause of death in primary amyloidosis.](https://image.slidesharecdn.com/glomer-101015091823-phpapp02/85/CME-Glomerular-Tubular-Disorders-26-320.jpg)
![ACUTE INTERSTITIAL NEPHRITIS DRUGS Antibiotics[betalactams,sulphonamides,vancomycin, erythromycin,minocycline] NSAID and cyclooxygenase 2inhibitor Diuretics [thiazides,frusemide,triamterine] Anti convulsions [phenytoin,phenobarbitol,CBZ,volproic acid] Misscelleneous [captopril,H2blockers,proton pump inhibitor] INFECTION Bacteria Viruses miscellaneous IDIOPATHIC Tubulointerstitial nephritis –uveitis syndrome Acute –tubule basement membrane disease sarcoidosis](https://image.slidesharecdn.com/glomer-101015091823-phpapp02/85/CME-Glomerular-Tubular-Disorders-28-320.jpg)
![CHRONIC INTERSTITIAL NEPHRITIS CAUSES KIDNEYS MACROSCOPICALLY NORMAL Drugs [lithim,cyclosporine,tacrolimus,indinavir,cisplatin] Metabolic [hyperuricemia,hypokalemia,hypercalcemia,hyperoxaluria,cystinosis] Heavy metals [lead,cadmium,arsenic,mercury,gold,uranium] Radiation Balkan nephropathy Immunemediated [SLE,sjogrens syndrome,sarcoidosis,wegner’s granulomatosis,other vasculitis] Vascular diseases [athero sclelotic kidney disease] Hematologic disturabances [multiple myeloma,light chain deposition disease, lymphoma, SCD,PNH] Progressive glomerular disease of all etiologies[glomerulonephritis, diabetes, hypertension] idiopathic](https://image.slidesharecdn.com/glomer-101015091823-phpapp02/85/CME-Glomerular-Tubular-Disorders-29-320.jpg)
![KIDNEYS MACROSCOPICALLY ABNORMAL Analgesic nephropathy Chronic obstruction Hereditary [nephronophtisis , medullary cystic disease , familial juvenile hyperuricemic nephropathy , ADPKD , ARPKD] Infection Chronic pylonephritis, malacoplakia,xanthogranulomatous pylonephritis]](https://image.slidesharecdn.com/glomer-101015091823-phpapp02/85/CME-Glomerular-Tubular-Disorders-30-320.jpg)
![FUNCTIONAL CONSEQUENCES OF TUBULO INTERSTITIAL DISEASE DEFECT CAUSES REDUCED GFR OBLITERATION OF microvasculature and obstruction of tubules FANCONI SYNDROME DAMAGE OF PROXIMAL TUBULAR REABSORBTION OF GLUCOSE , AMINOACIDS, PHASPHATE ,AND BICORBANATE HYPERCHOREMIC ACIDOSIS 1.REDUCED AMMONIA PRODUCTION 2.INABILITY TO ACIDIFY THE COLLECTING DUCT [DISTAL RTA] 3.PROXIMAL BICORBANATE WASTING TUBULAR OR SMALL MOLECULAR WEIGHT PROTENURIA FAILURE OF PROXIMAL TUBULE PROTEIN REABSORBTION POLYURIA ,ISOTHENUIA DAMAGE TO MEDULLARY TUBULES AND VASCULATURE HYPERKALEMIA POTTASIUM SECRETARY DEFECTS INCLUDING ALDOSTERONE RESISTANCE](https://image.slidesharecdn.com/glomer-101015091823-phpapp02/85/CME-Glomerular-Tubular-Disorders-31-320.jpg)
![Analgesic nephropathy Heavy users of analgesics mixtures containing phenacetin combination with aspirin acetoaminophen,or coffeine,. Clinical features; renal insufficiency,non nephrotic proteinuria,or sterile pyuria Hypertension, anemia and impaired urinary concentration –renal insufficiency Flank pain and hematuria-pappillary necrosis Diagnosis ;1]history 2 ] CT - signs decreased renal size pappillary calcifications More prone for transitional cell carcinoma](https://image.slidesharecdn.com/glomer-101015091823-phpapp02/85/CME-Glomerular-Tubular-Disorders-32-320.jpg)