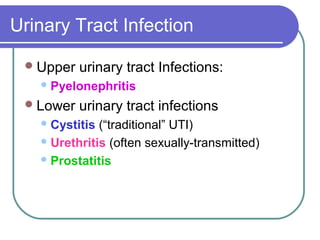
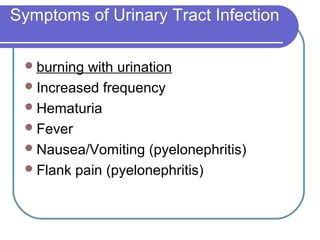
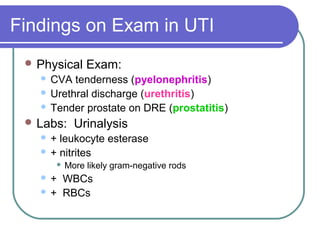
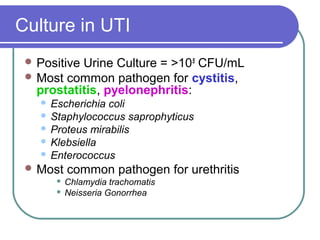
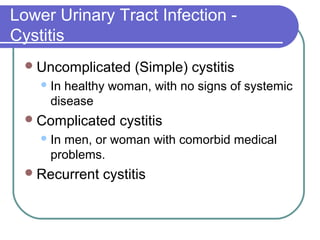
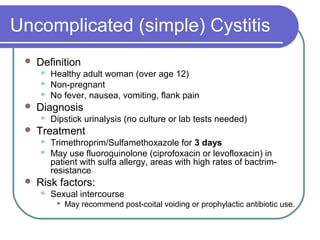
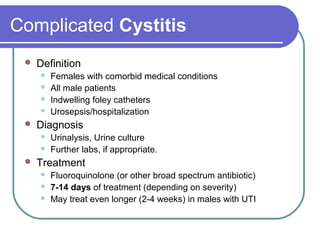
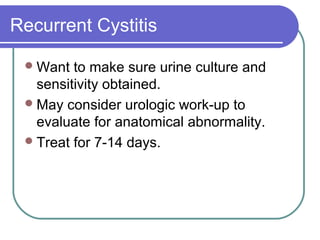
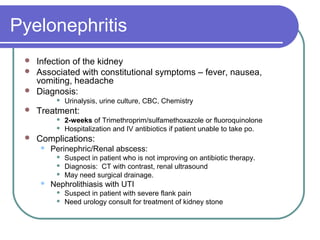
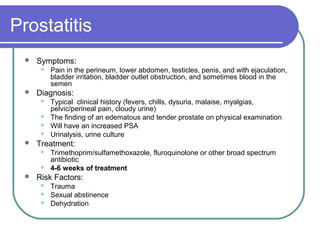
A urinary tract infection (UTI) can affect either the lower urinary tract (bladder and urethra) or upper urinary tract (kidneys and ureters). Common symptoms include burning during urination, increased frequency, and hematuria. Escherichia coli is the most frequent cause. Treatment depends on whether the infection is uncomplicated cystitis, complicated cystitis, recurrent cystitis, pyelonephritis, or prostatitis and involves antibiotics for varying durations.