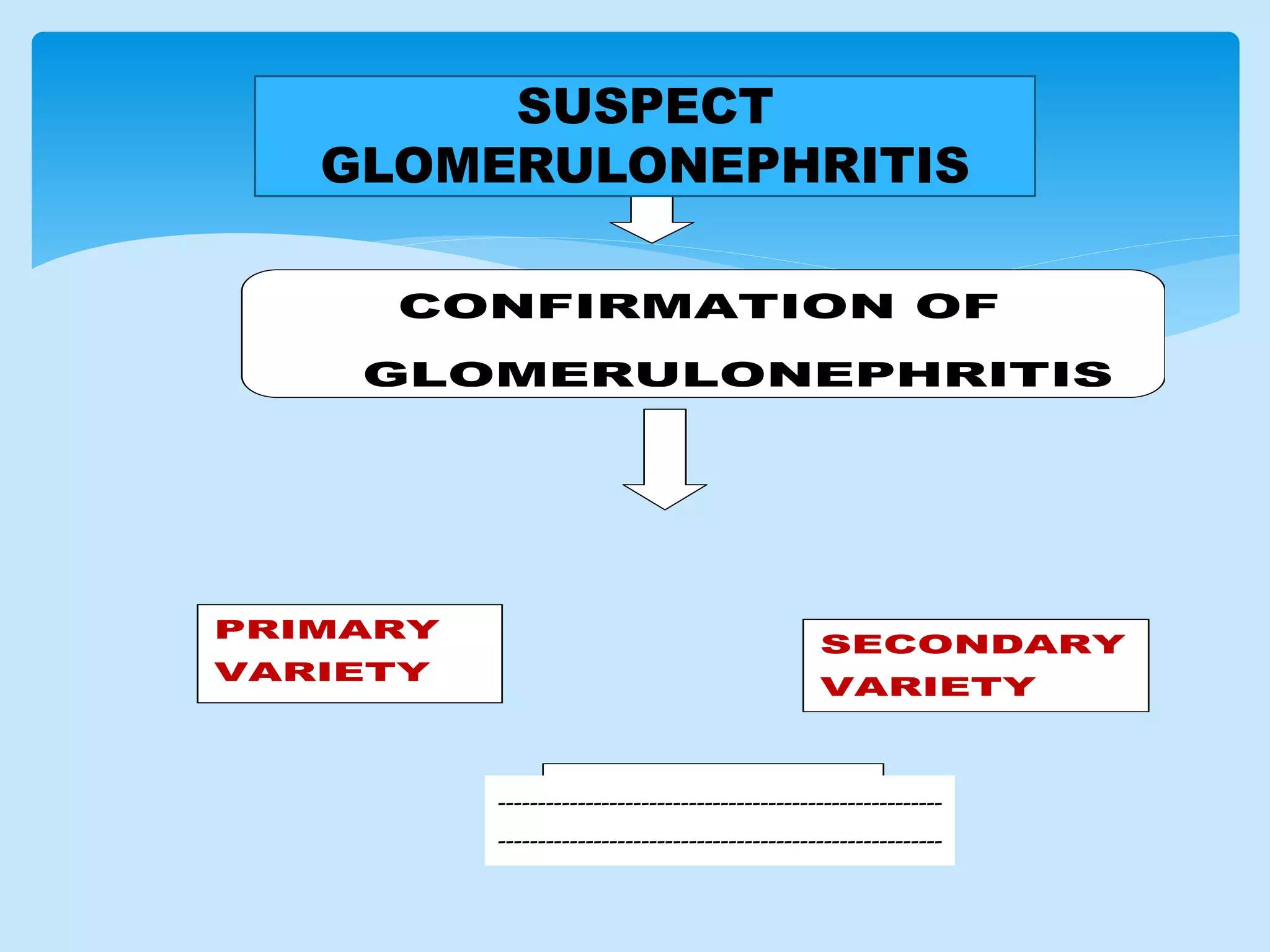
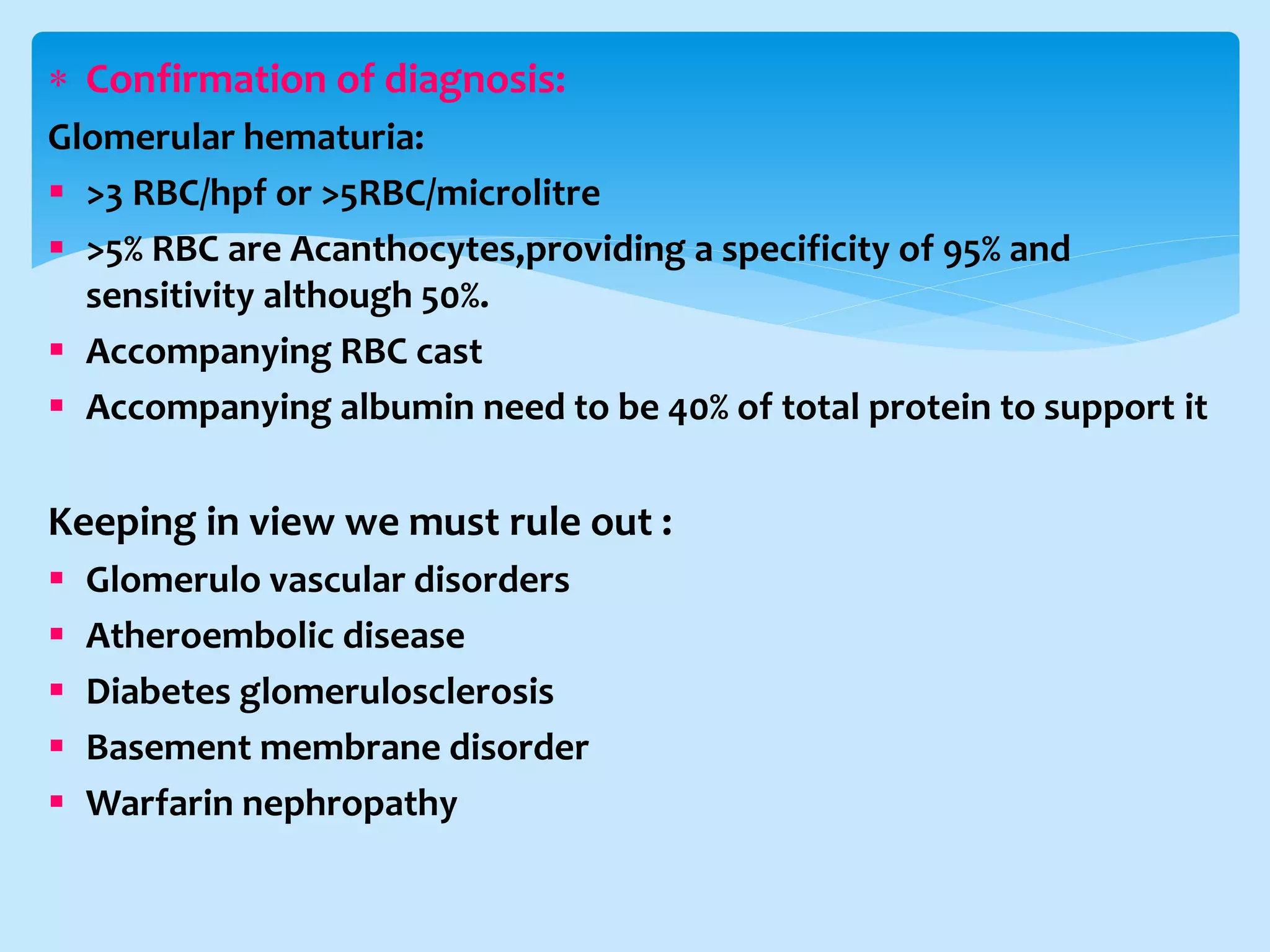
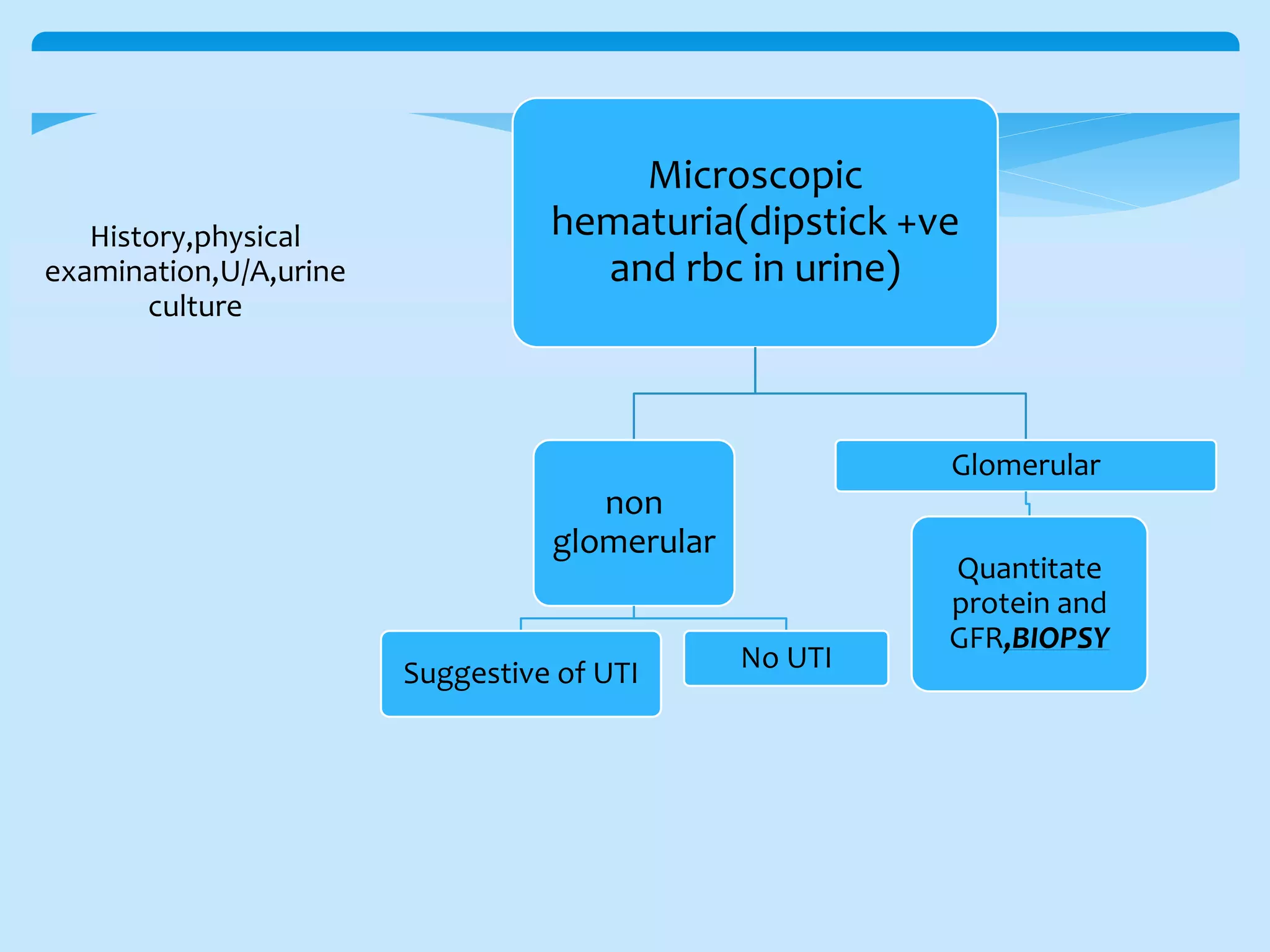
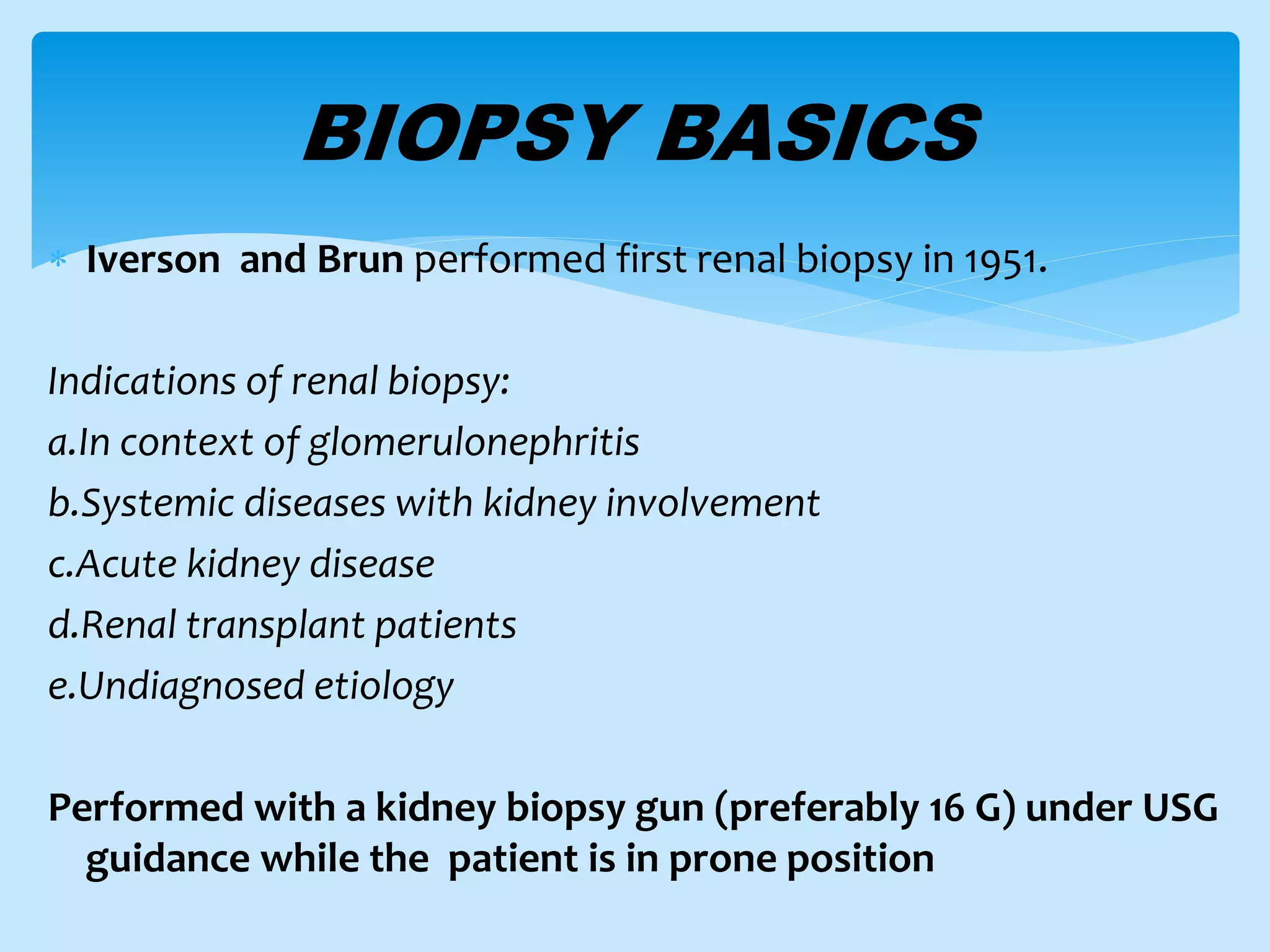
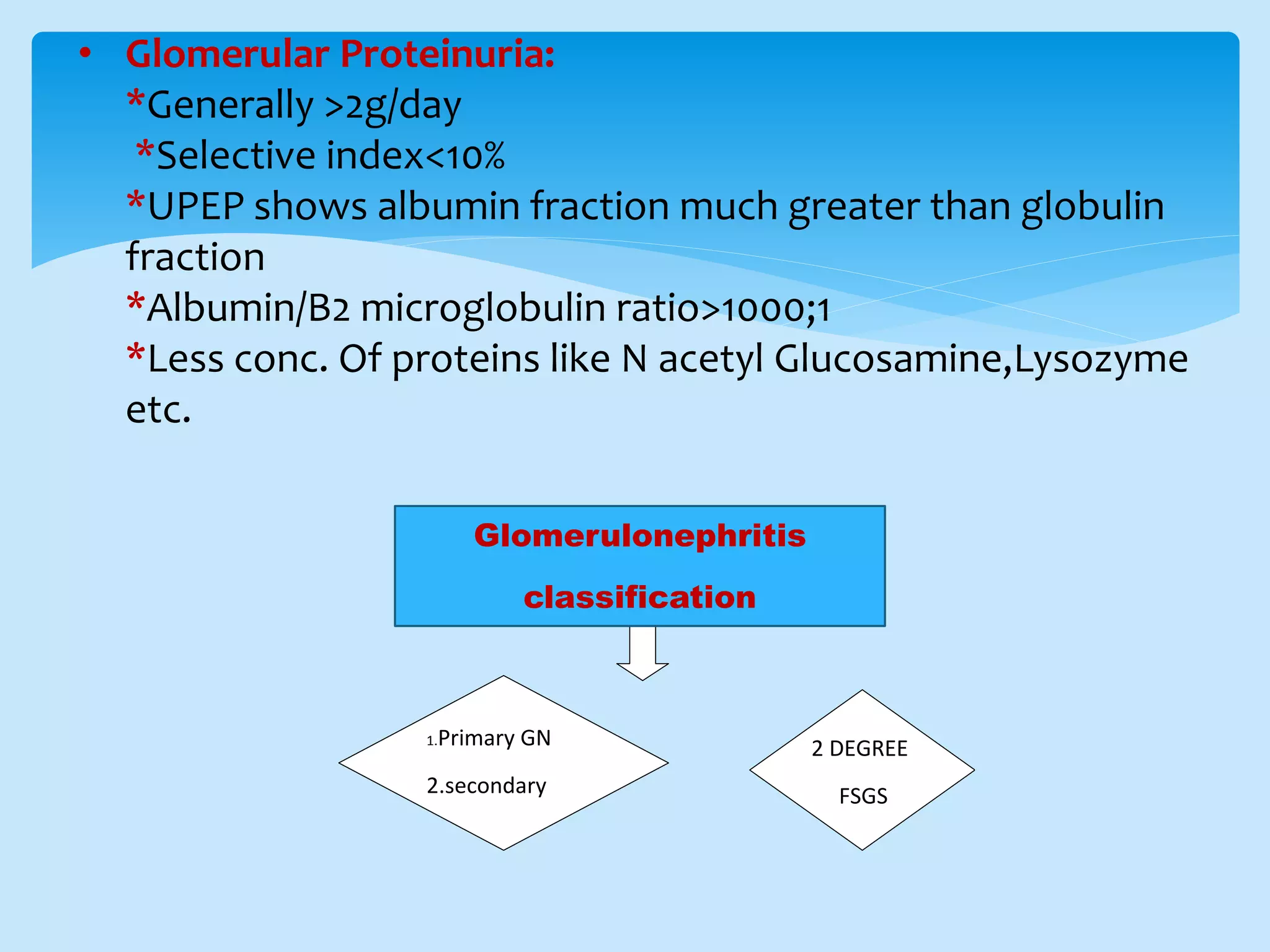
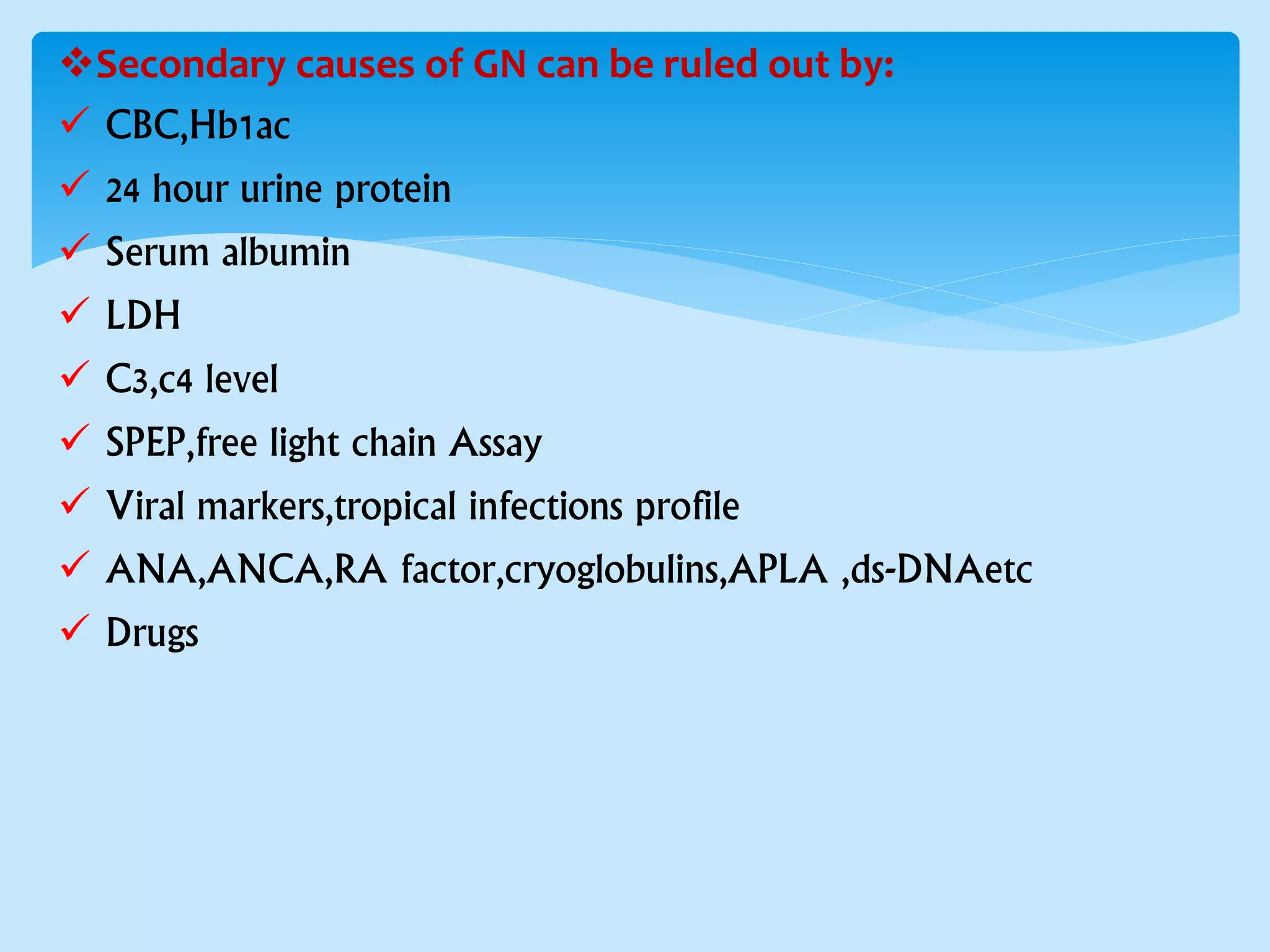
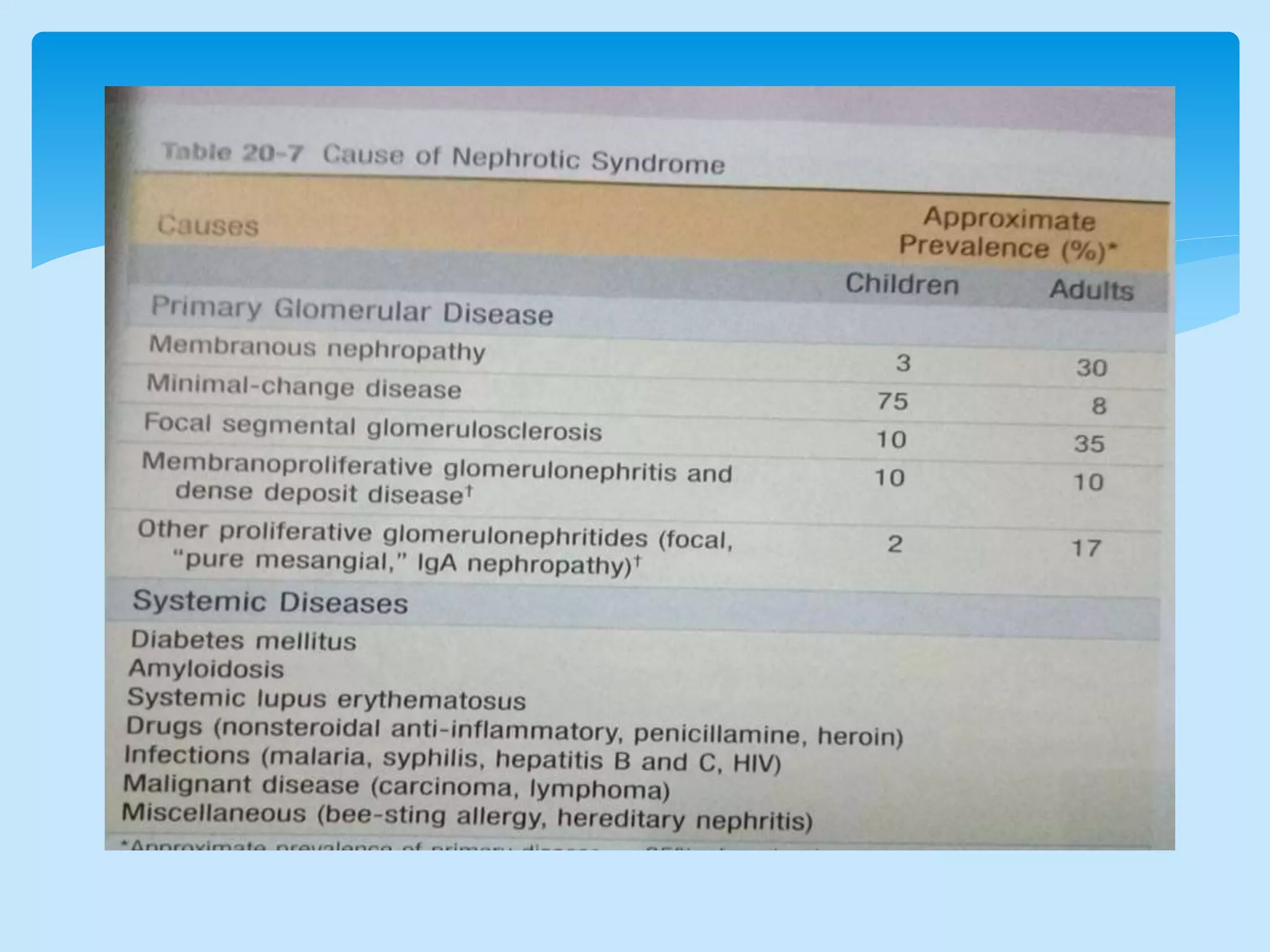
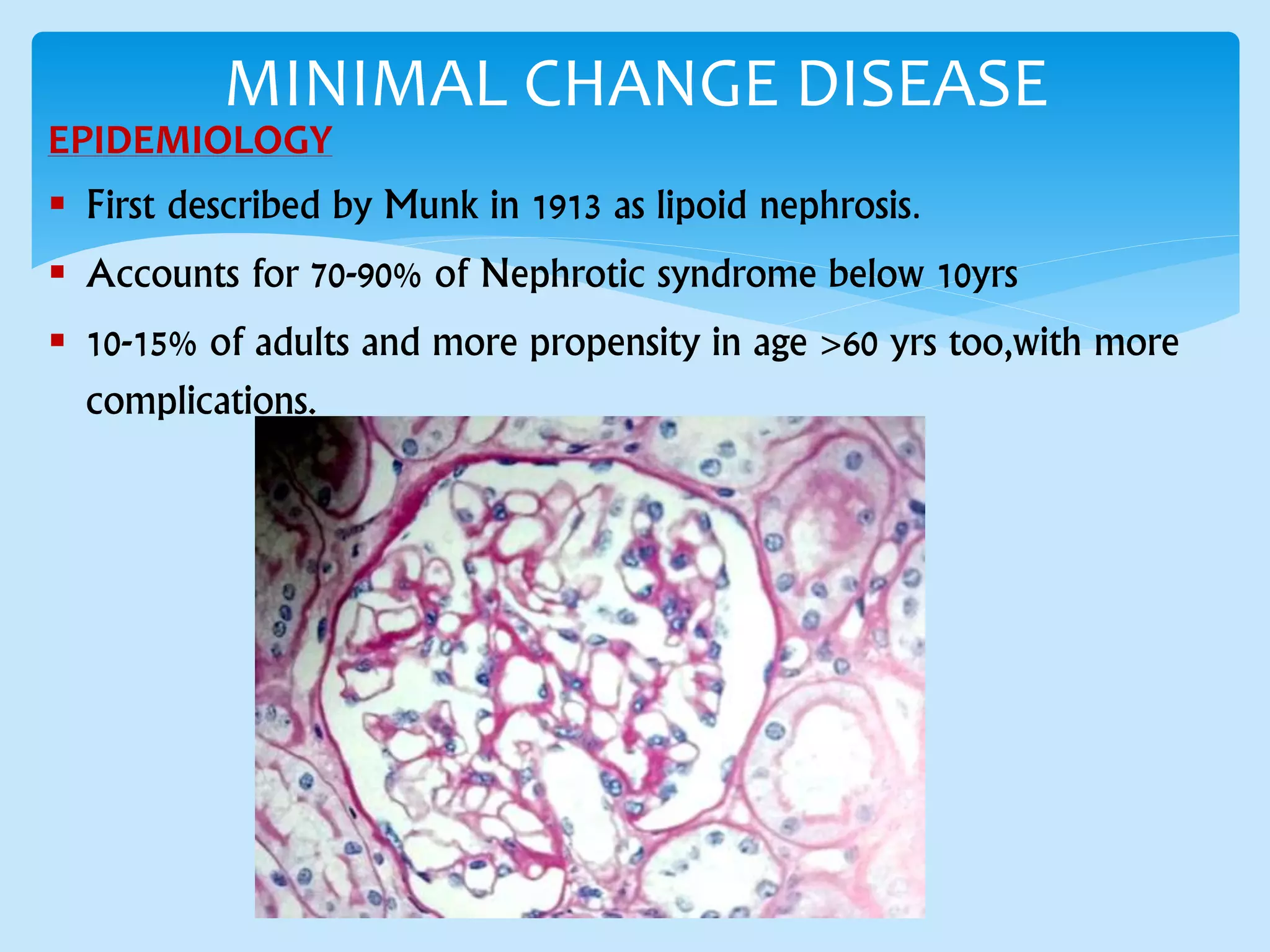
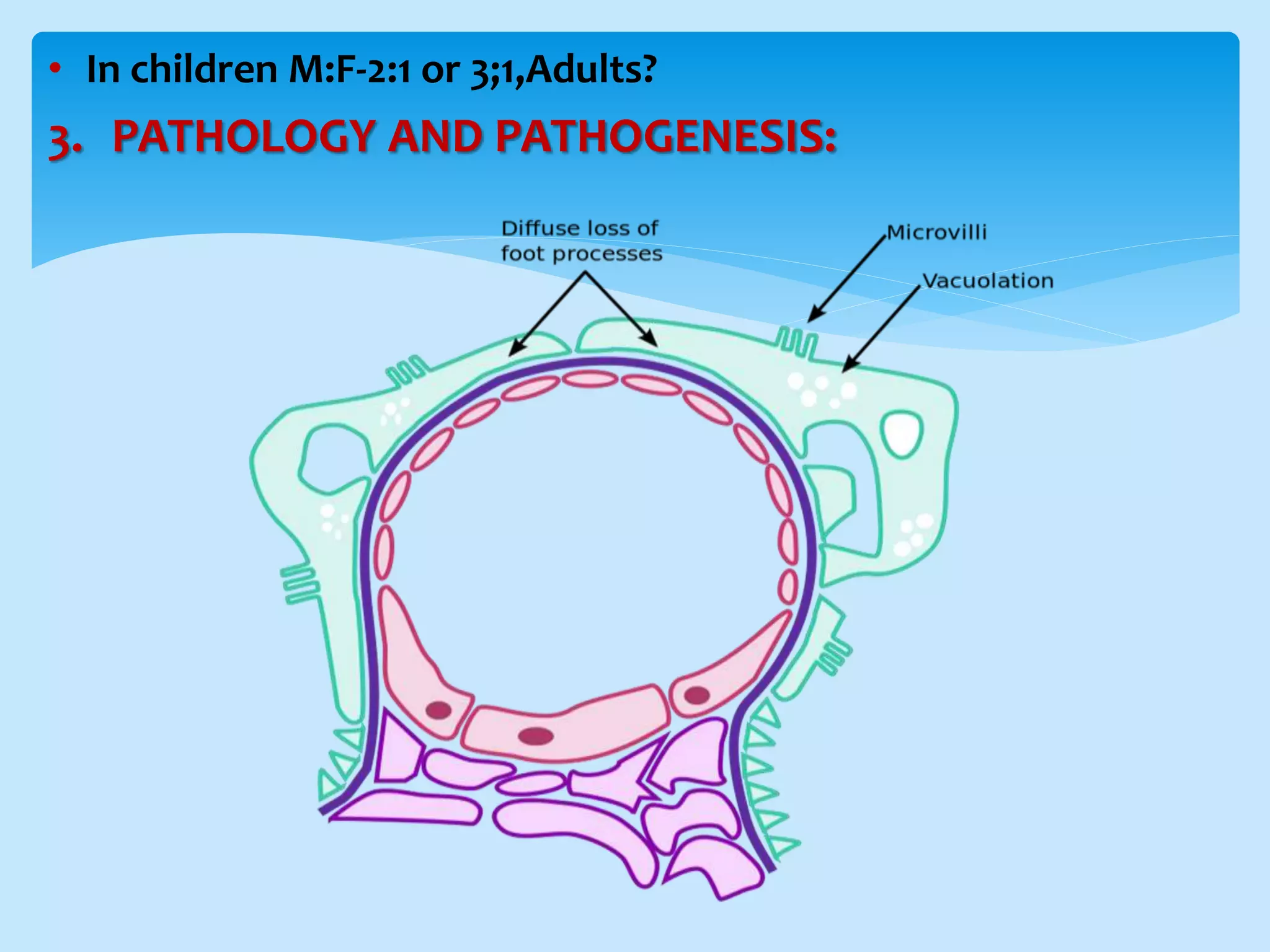
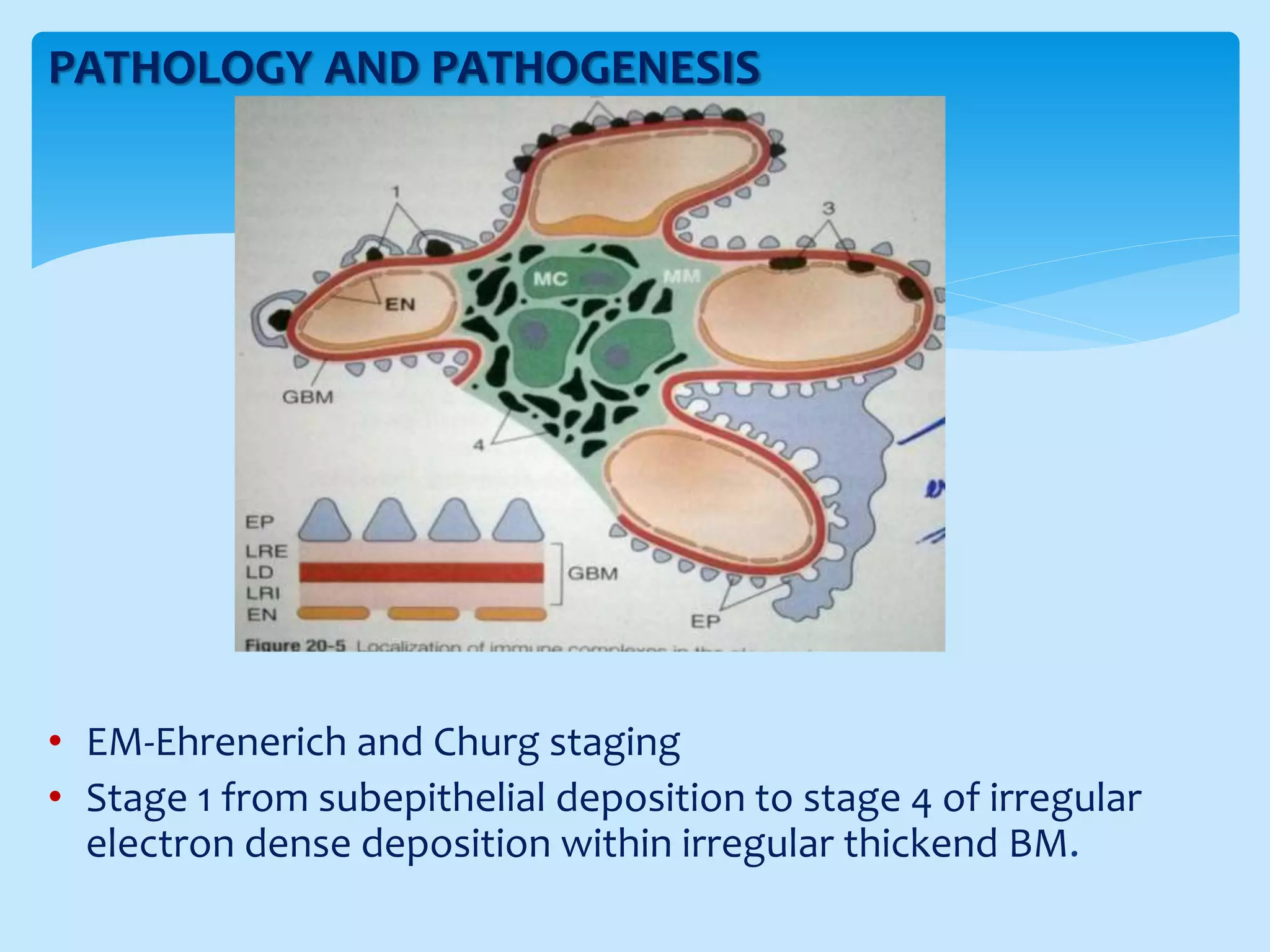
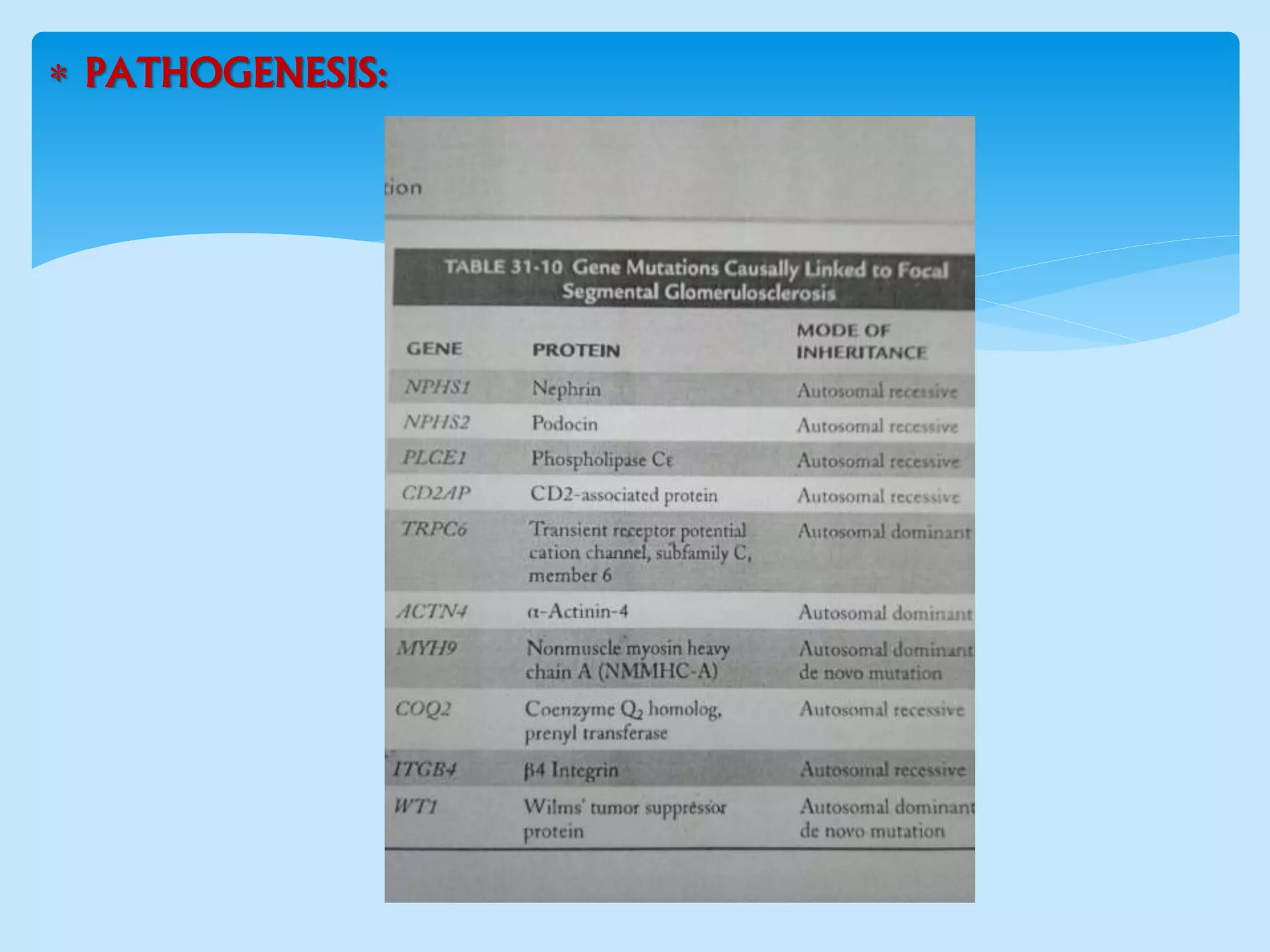
Primary glomerulonephritis refers to inflammation of the glomerular capillaries where the kidney is the only organ involved. It can present as acute nephritic syndrome, nephrotic syndrome, or isolated hematuria/proteinuria. Diagnosis involves ruling out secondary causes through labs and biopsy showing glomerular inflammation. Common primary glomerulonephritides include minimal change disease, IgA nephropathy, membranous glomerulopathy, and focal segmental glomerulosclerosis. Treatment involves controlling proteinuria and hypertension with steroids, immunosuppressants, or renin-angiotensin system blockers depending on disease classification and severity.