The document provides an overview of spinal anatomy including:
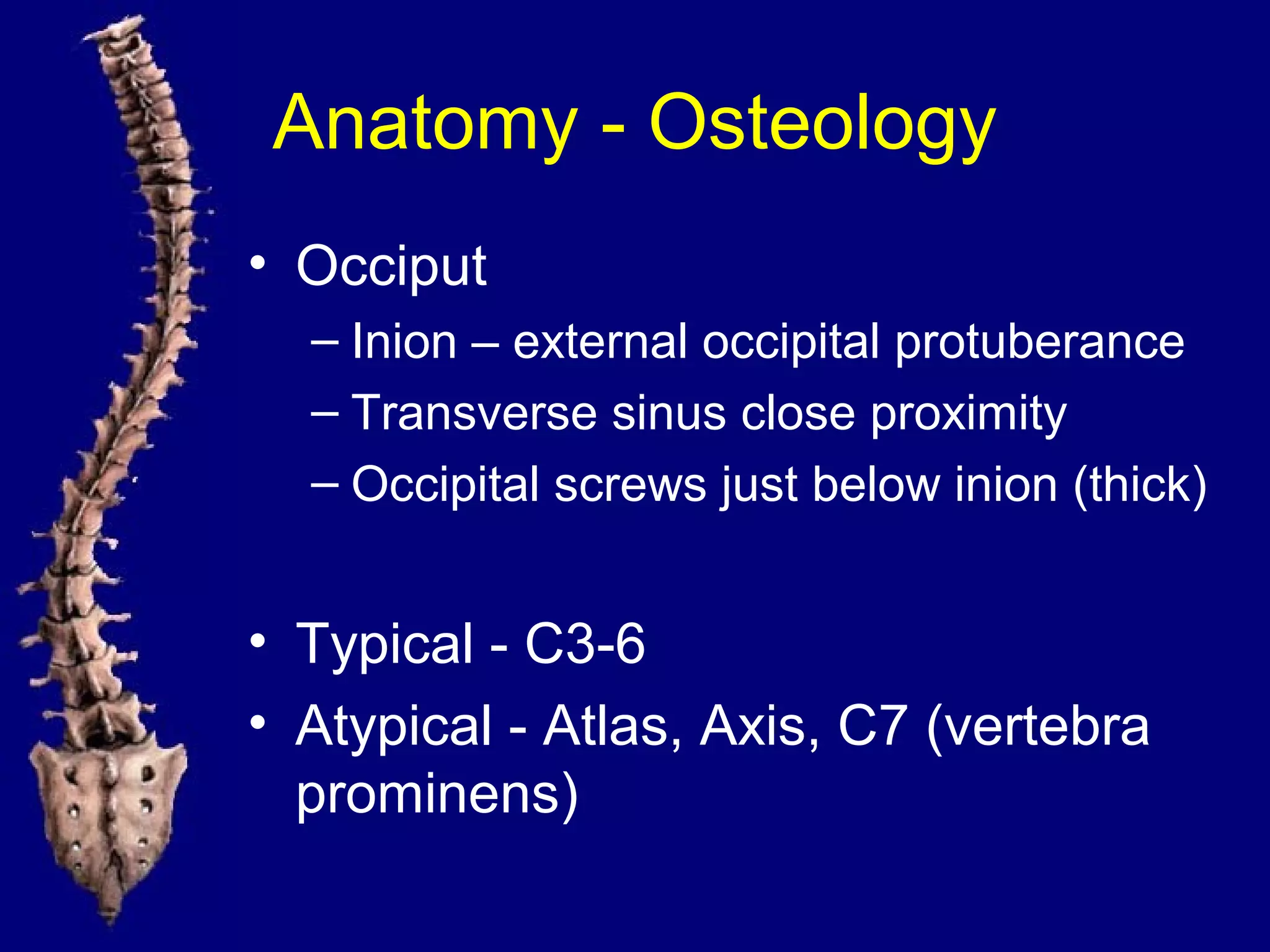
- The 7 cervical, 12 thoracic, 5 lumbar vertebrae and sacrum/coccyx bones that make up the spine.
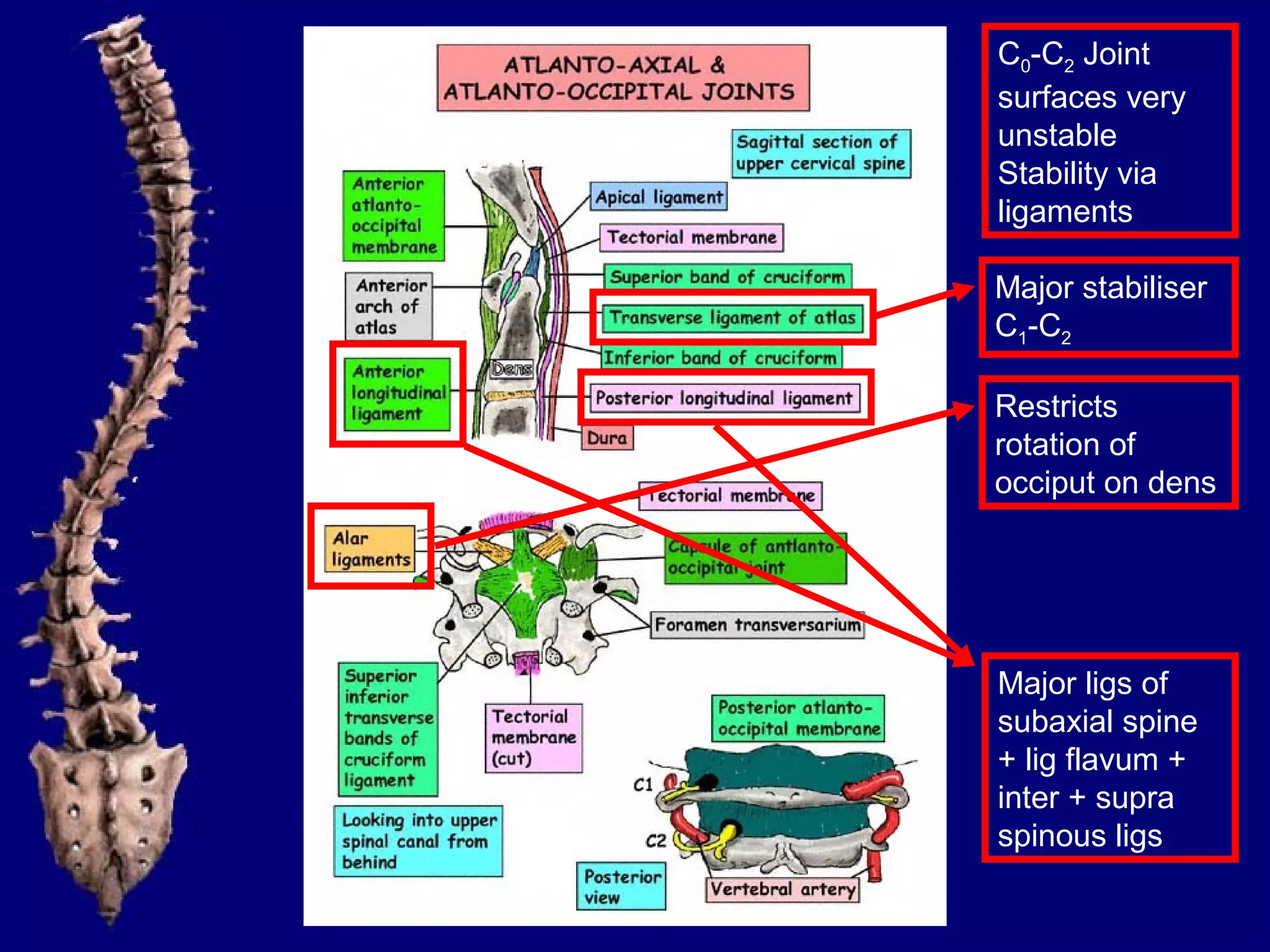
- Key structures like the anterior/posterior columns that provide compression/tension resistance.
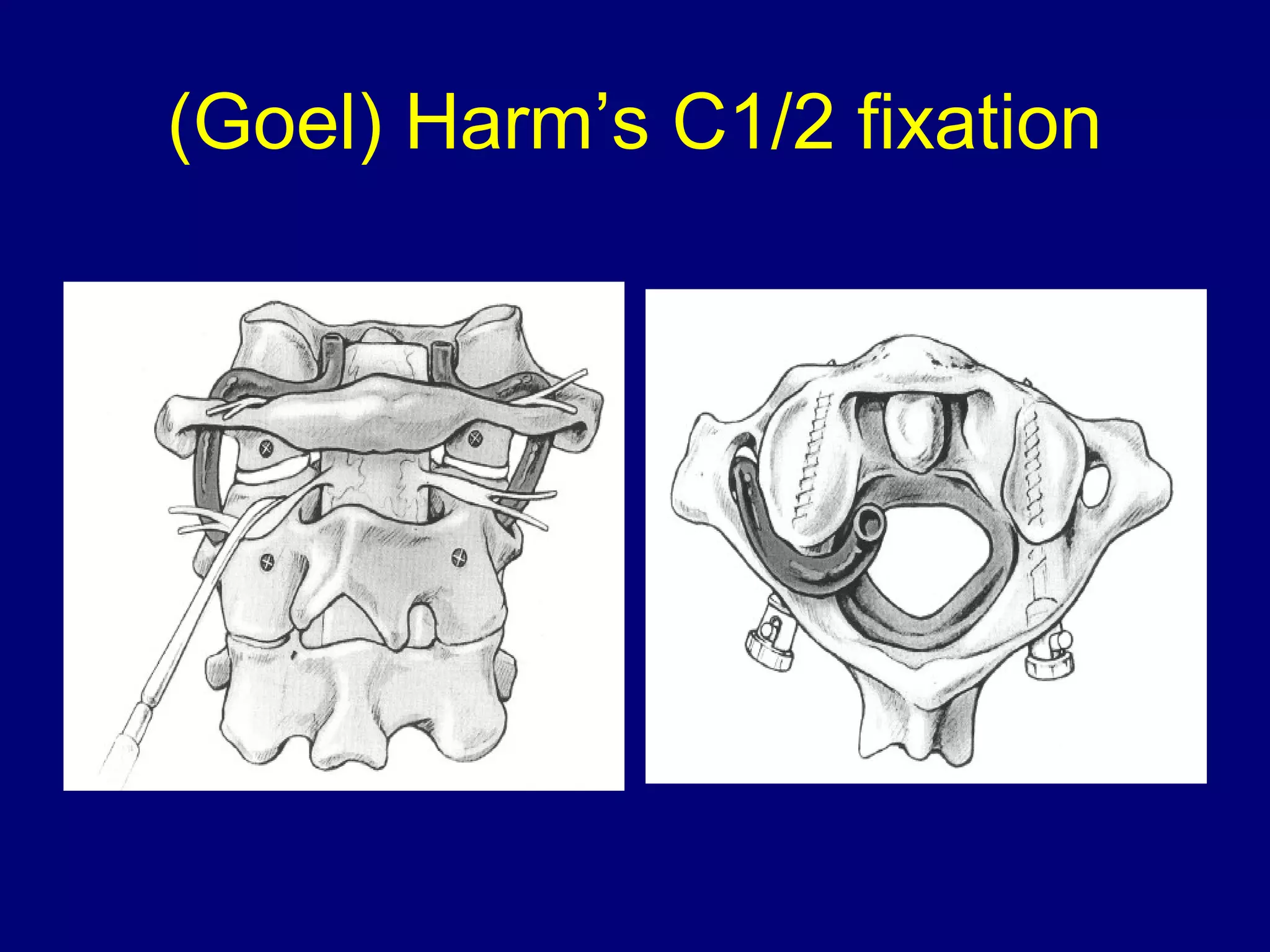
- Facet joints that resist rotation and displacement.
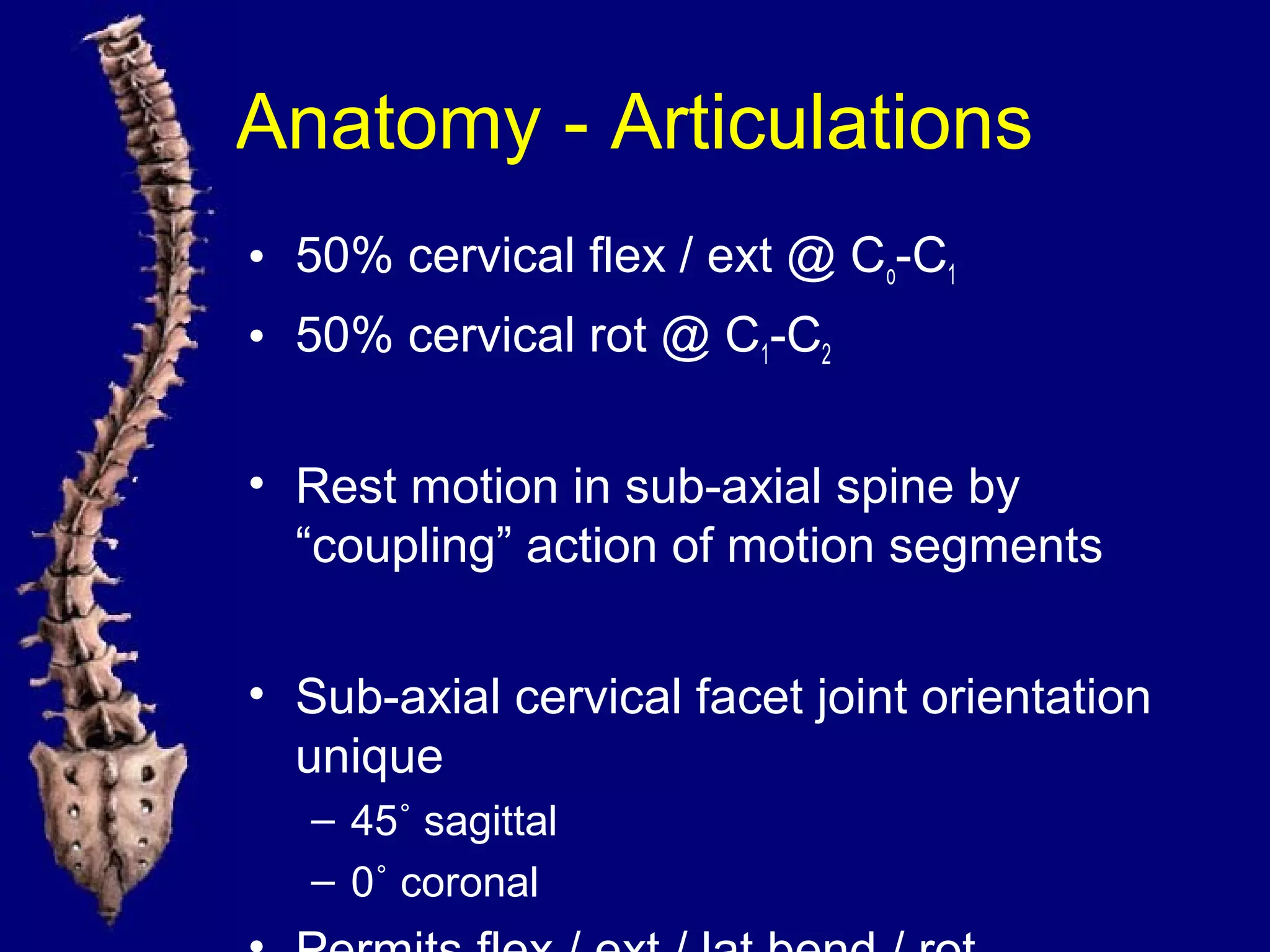
- Important anatomical features of each region like the cervical facet orientation and thoracic transverse processes.
- Neural structures like the spinal cord, nerves and nerve roots.
- Key concepts like clinical instability and relationships between structures.