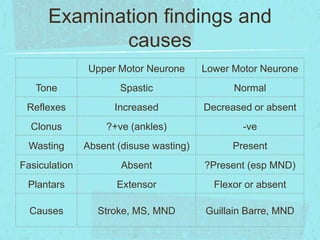
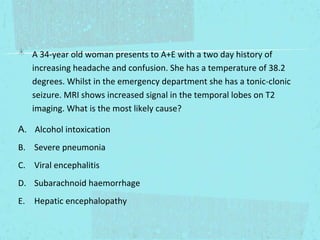
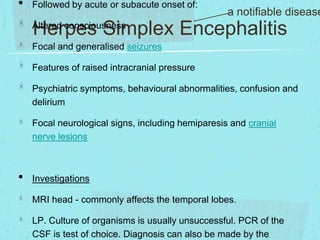
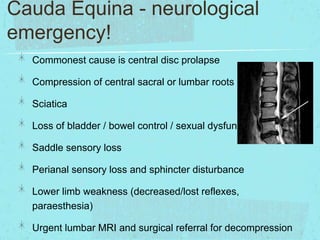
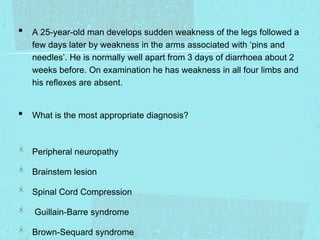
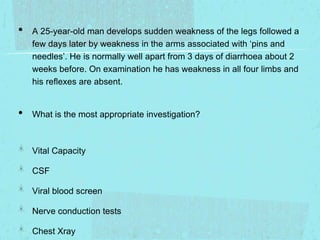
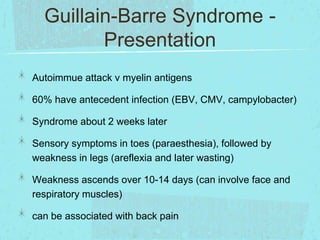
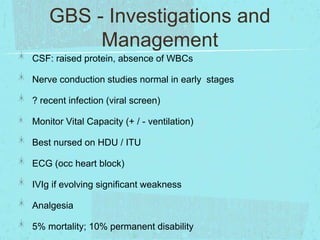
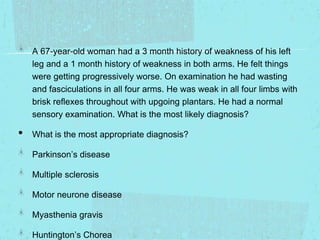
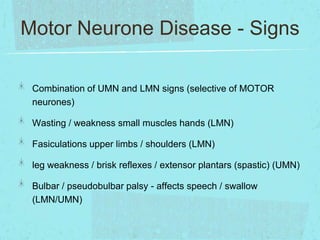
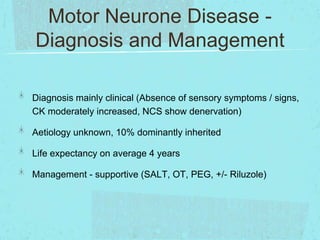
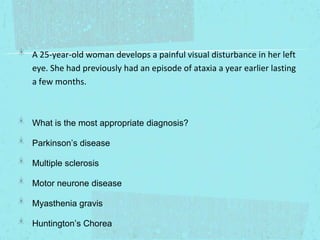
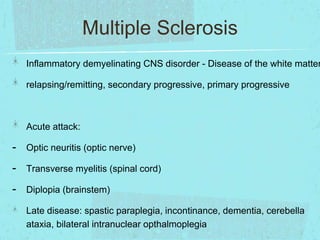
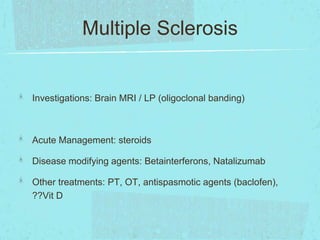
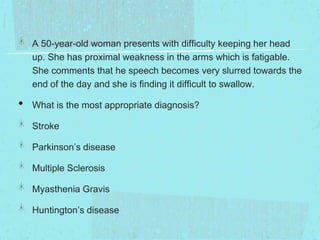
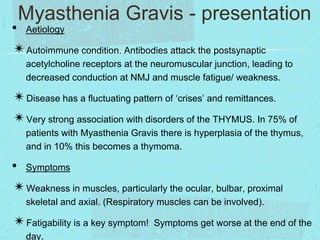
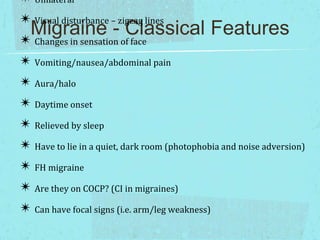
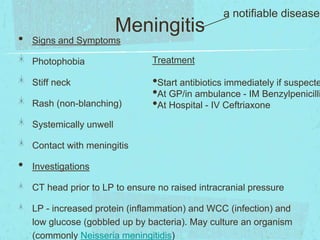
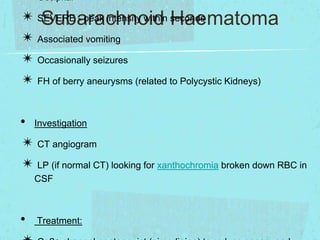
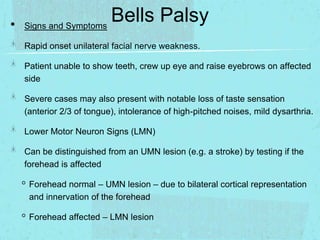
This document provides a summary of clinical syndromes and neurological conditions for medical students. It includes tables comparing upper and lower motor neuron signs. It also provides descriptions of various conditions like herpes simplex encephalitis, Guillain-Barre syndrome, cauda equina syndrome, multiple sclerosis, motor neuron disease, myasthenia gravis, Parkinson's disease, and Bell's palsy. Example cases are presented and the appropriate diagnosis and investigations are discussed for each case. Overall the document serves as a review of key neurology topics for medical students.