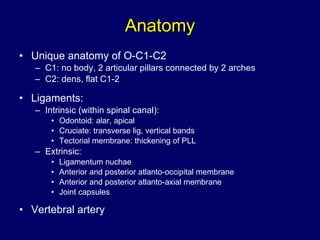
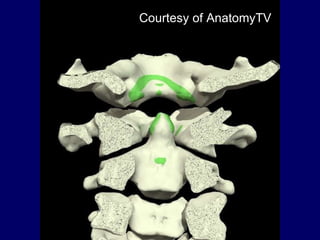
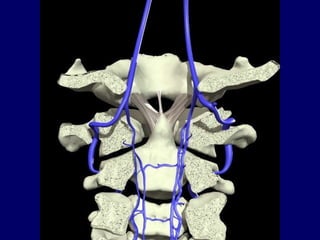
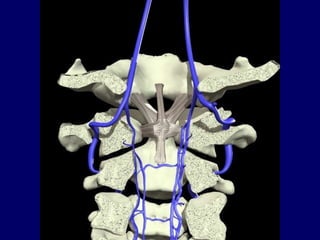
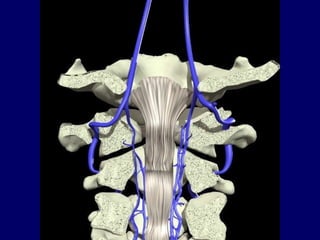
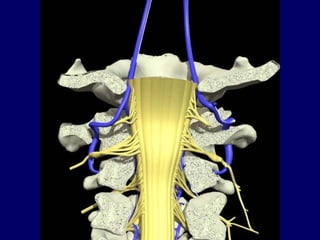
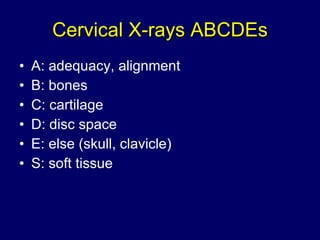
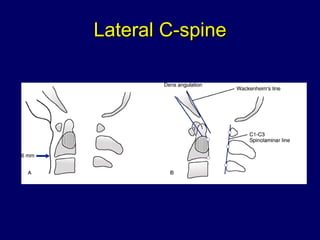
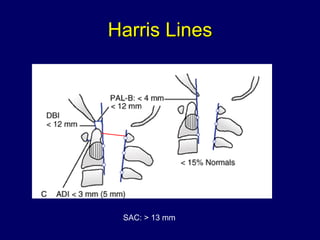
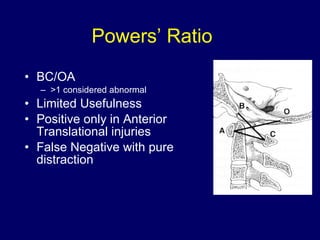
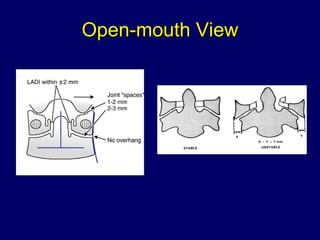
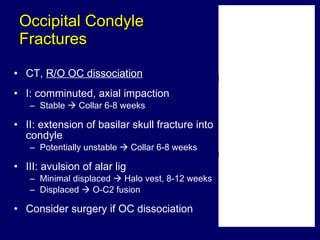
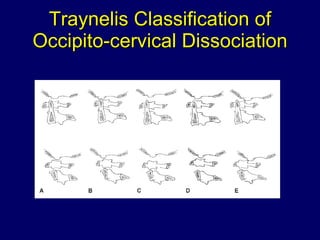
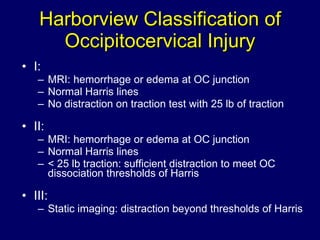
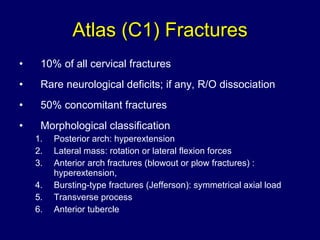
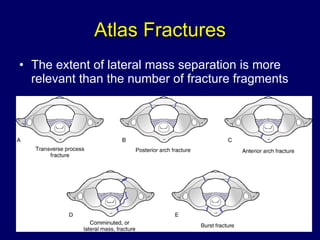
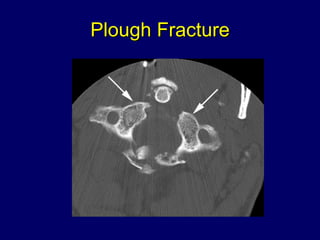
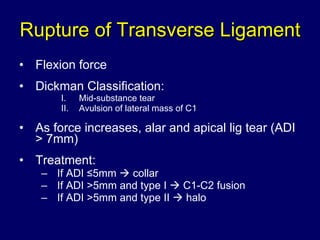
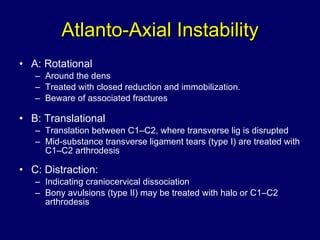
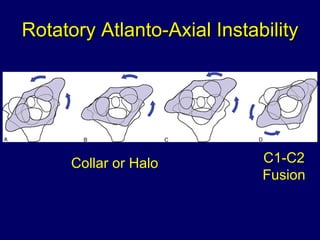
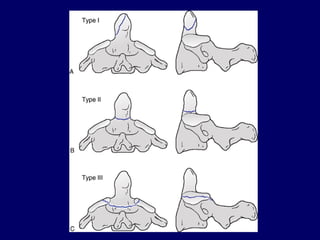
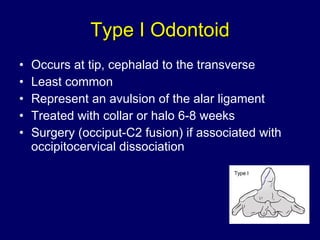
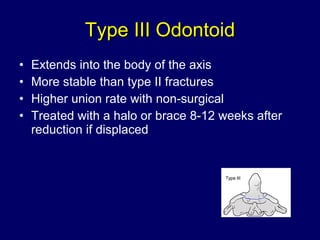
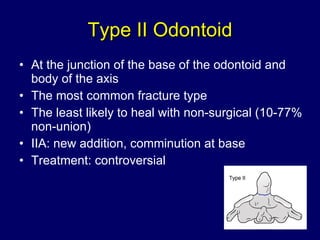
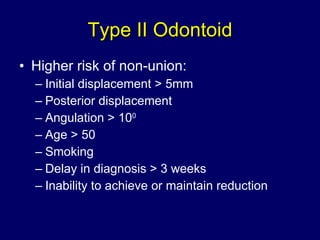
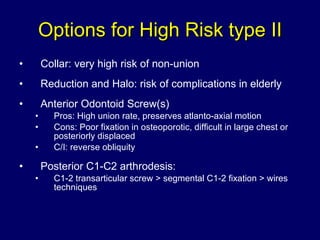
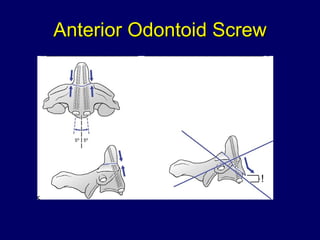
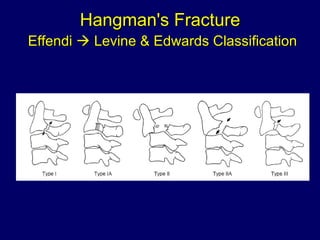
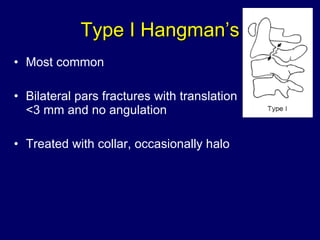
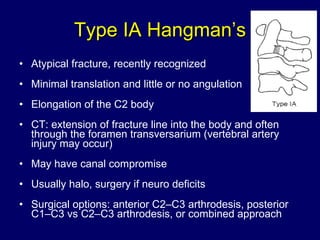
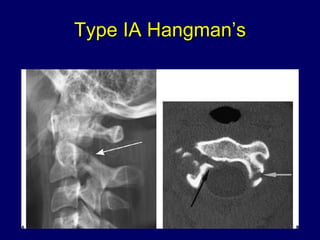
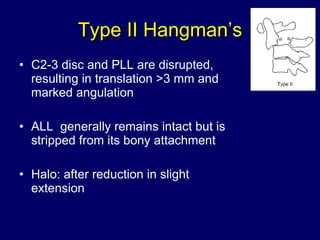
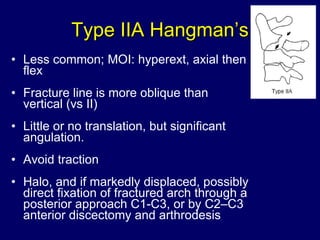
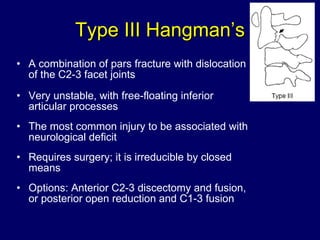
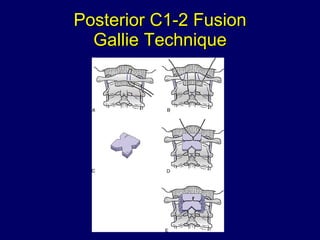
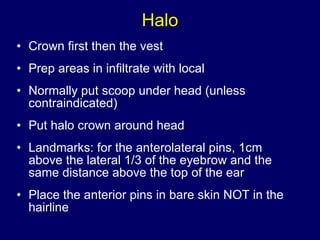
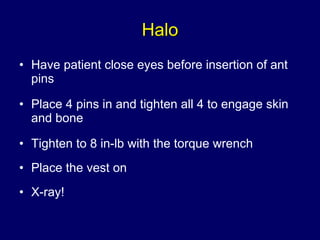
The document discusses upper cervical trauma, highlighting the anatomy, types of fractures, and their associated treatment protocols. It emphasizes the importance of early recognition, appropriate pre-hospital care, and specific radiographic evaluations for better management of cervical injuries. Various classifications and treatment options for different types of cervical fractures, including odontoid and hangman's fractures, are also outlined.