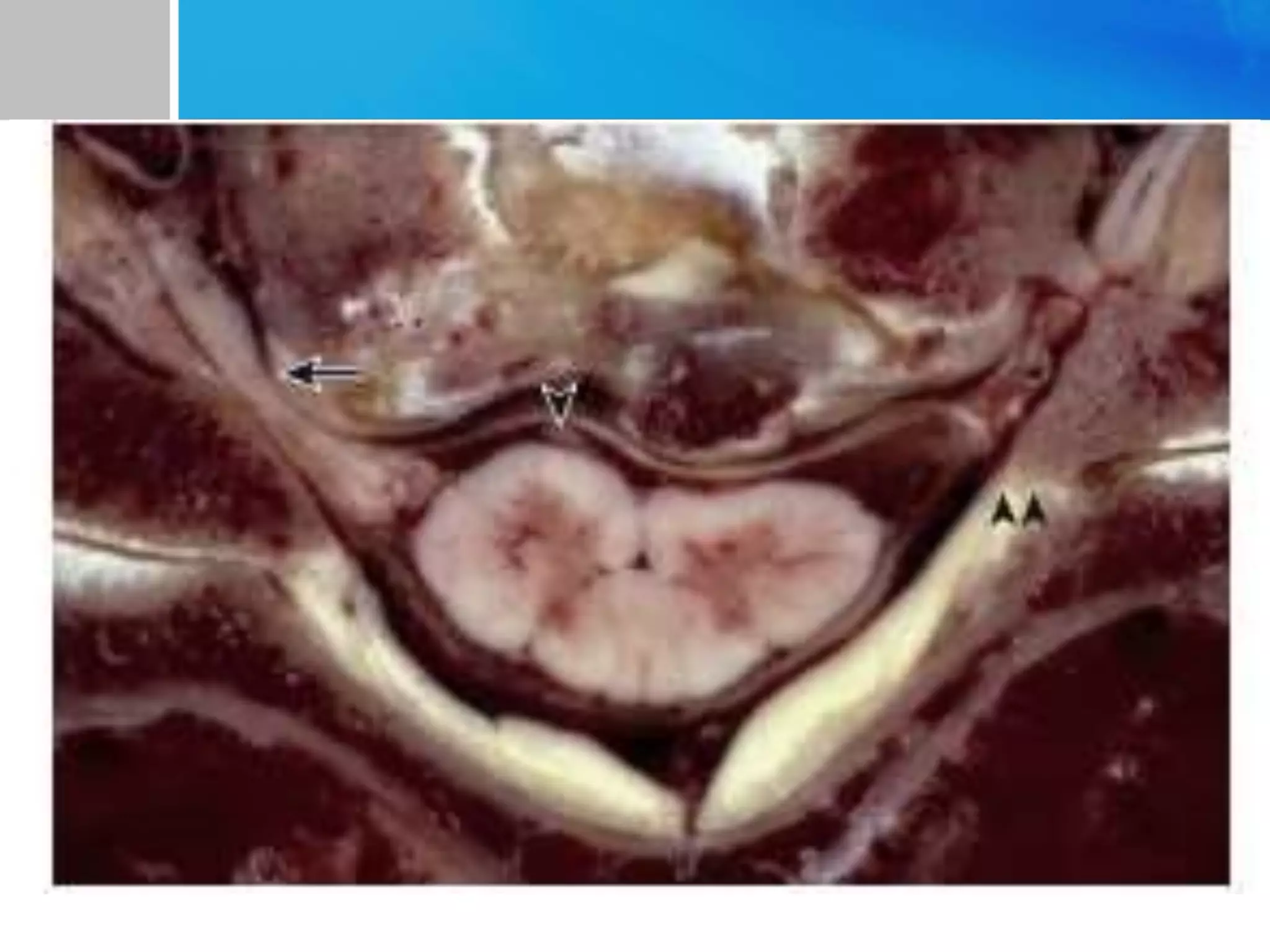
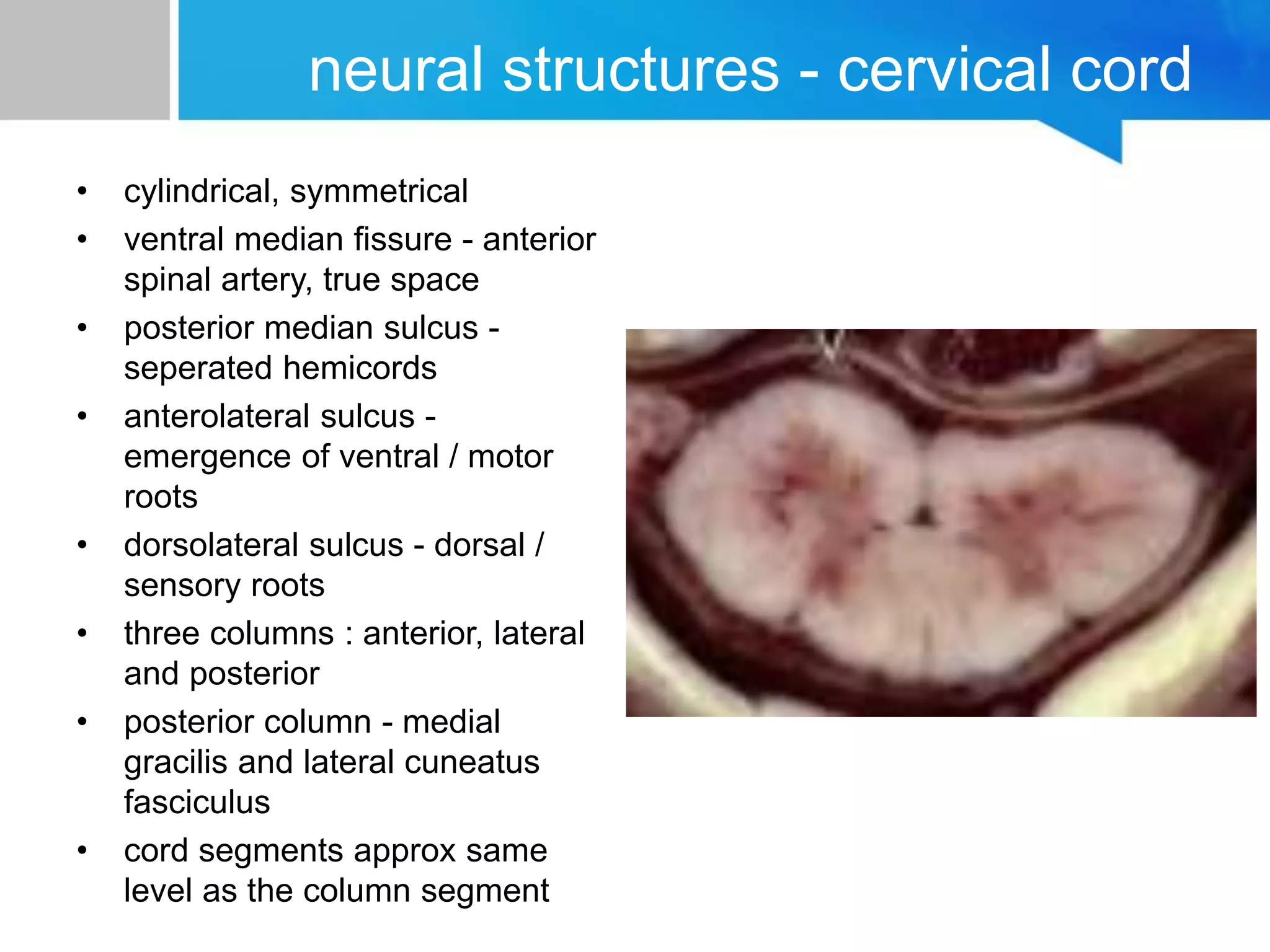
1) The cervical spine has 7 vertebrae connected by viscoelastic structures forming a flexible column for neuroprotection and support.
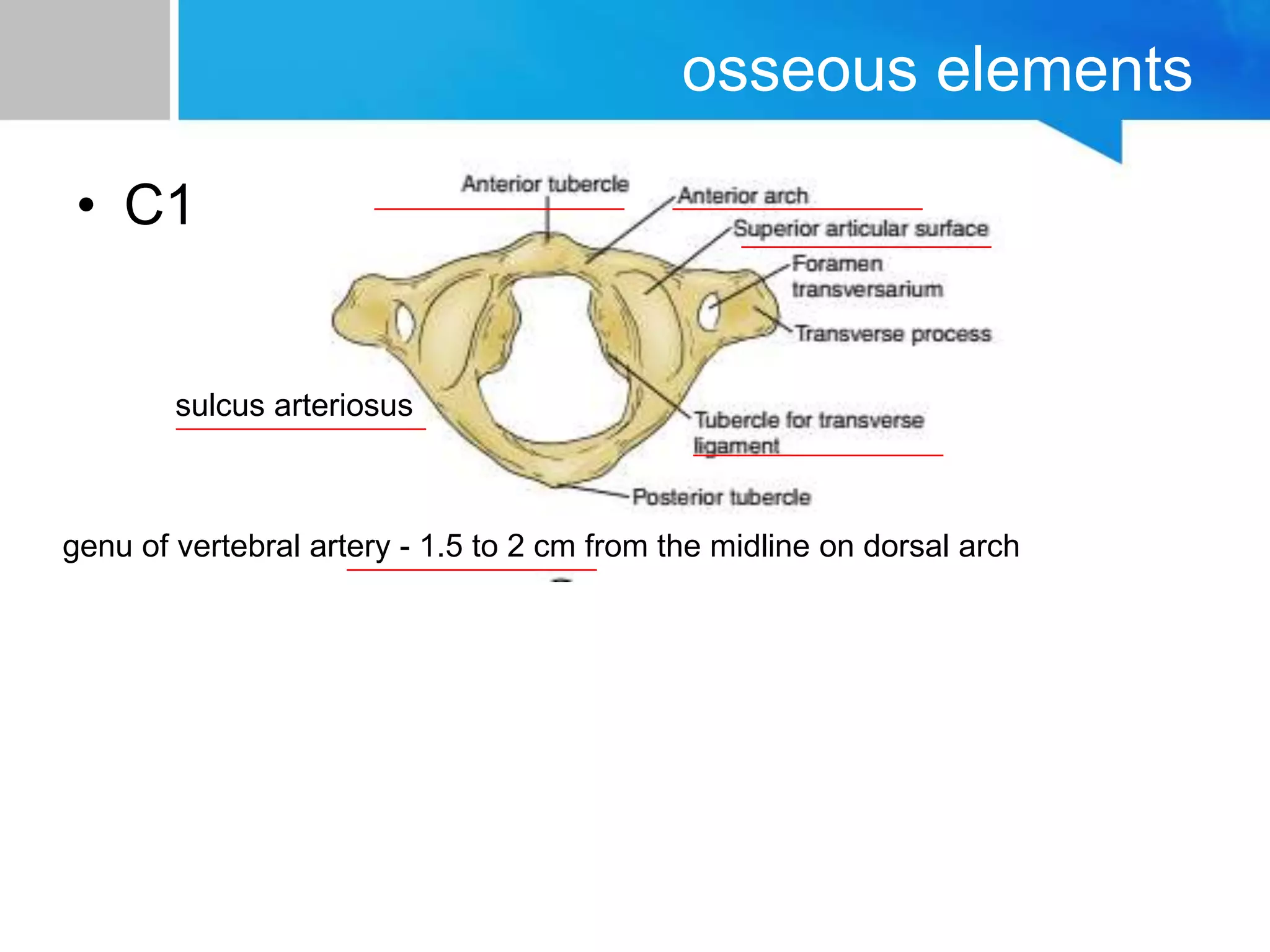
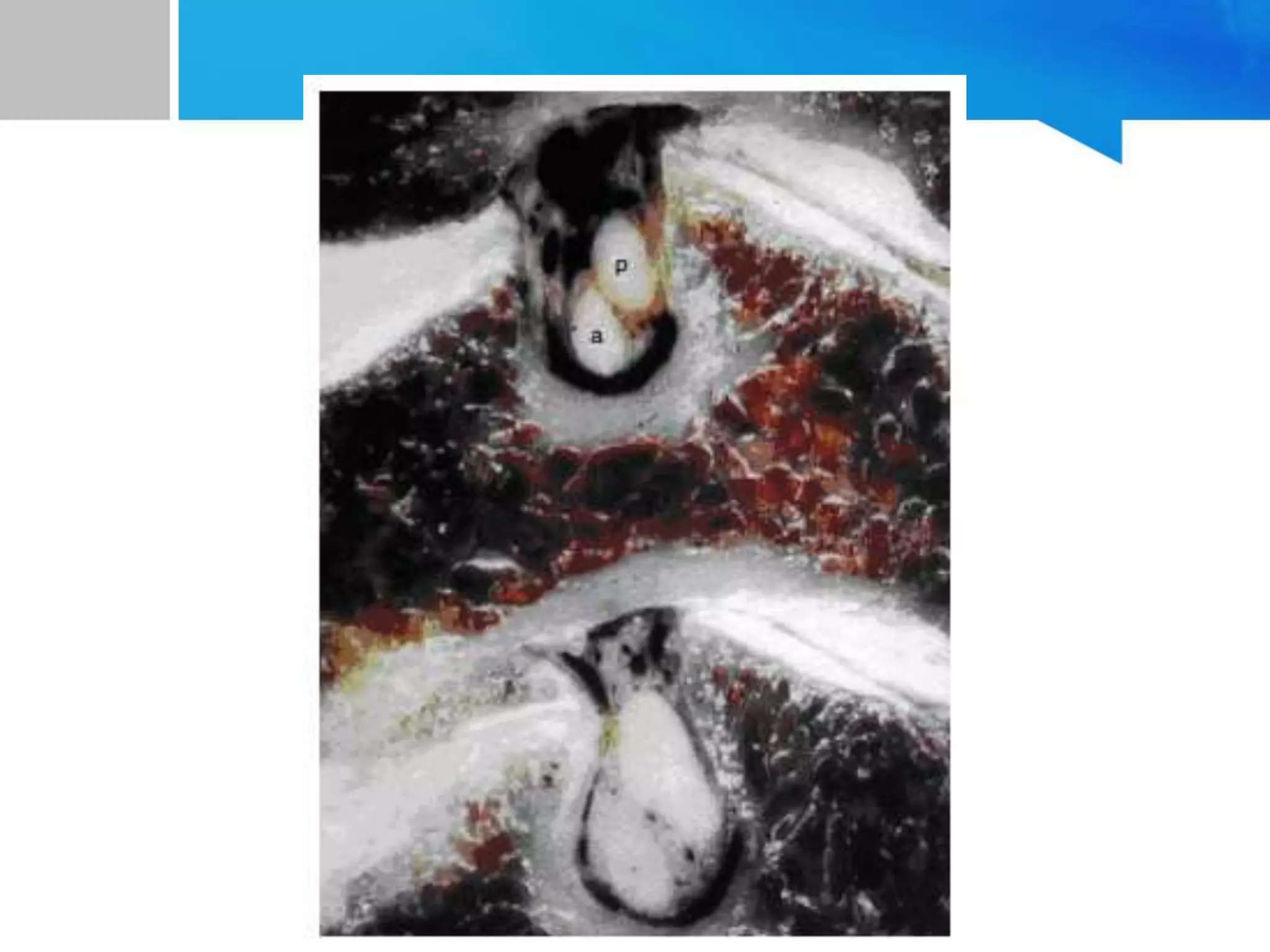
2) The C1 vertebra has anatomical landmarks including the sulcus arteriosus and the C2 vertebra has the odontoid process and transverse ligament.
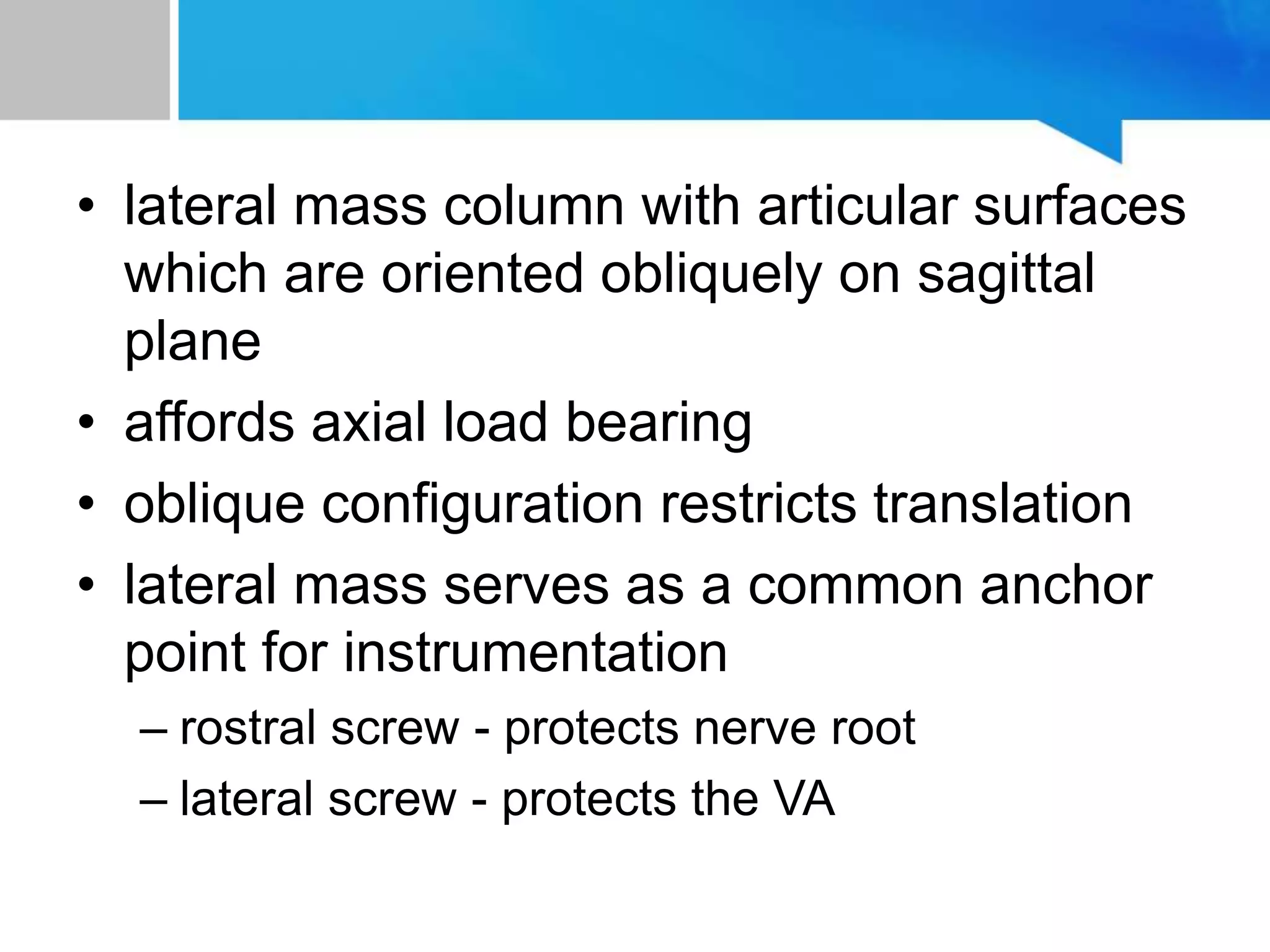
3) The subaxial vertebrae have vertebral bodies, transverse processes, and pedicles connecting to the dorsal arch.