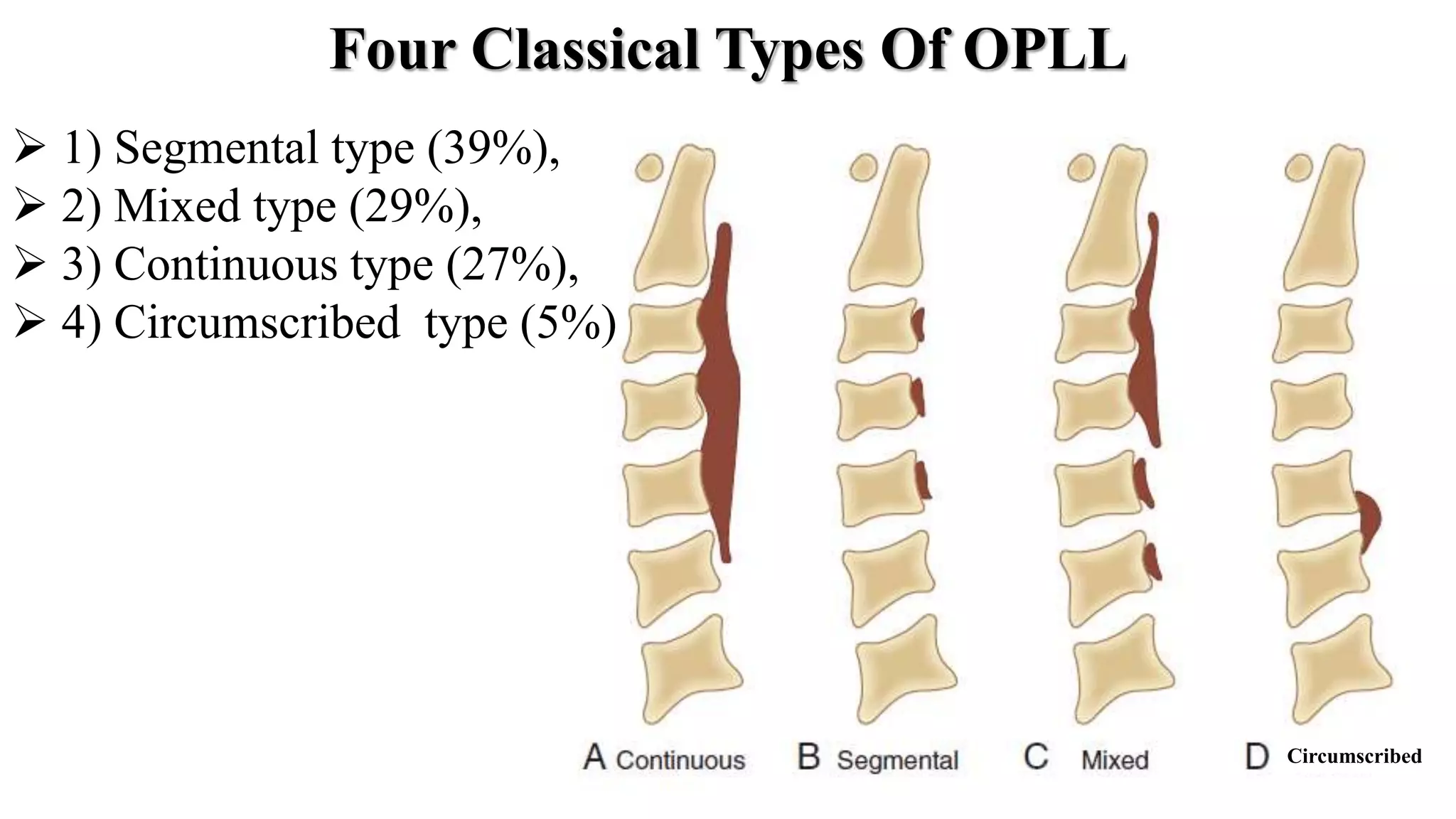
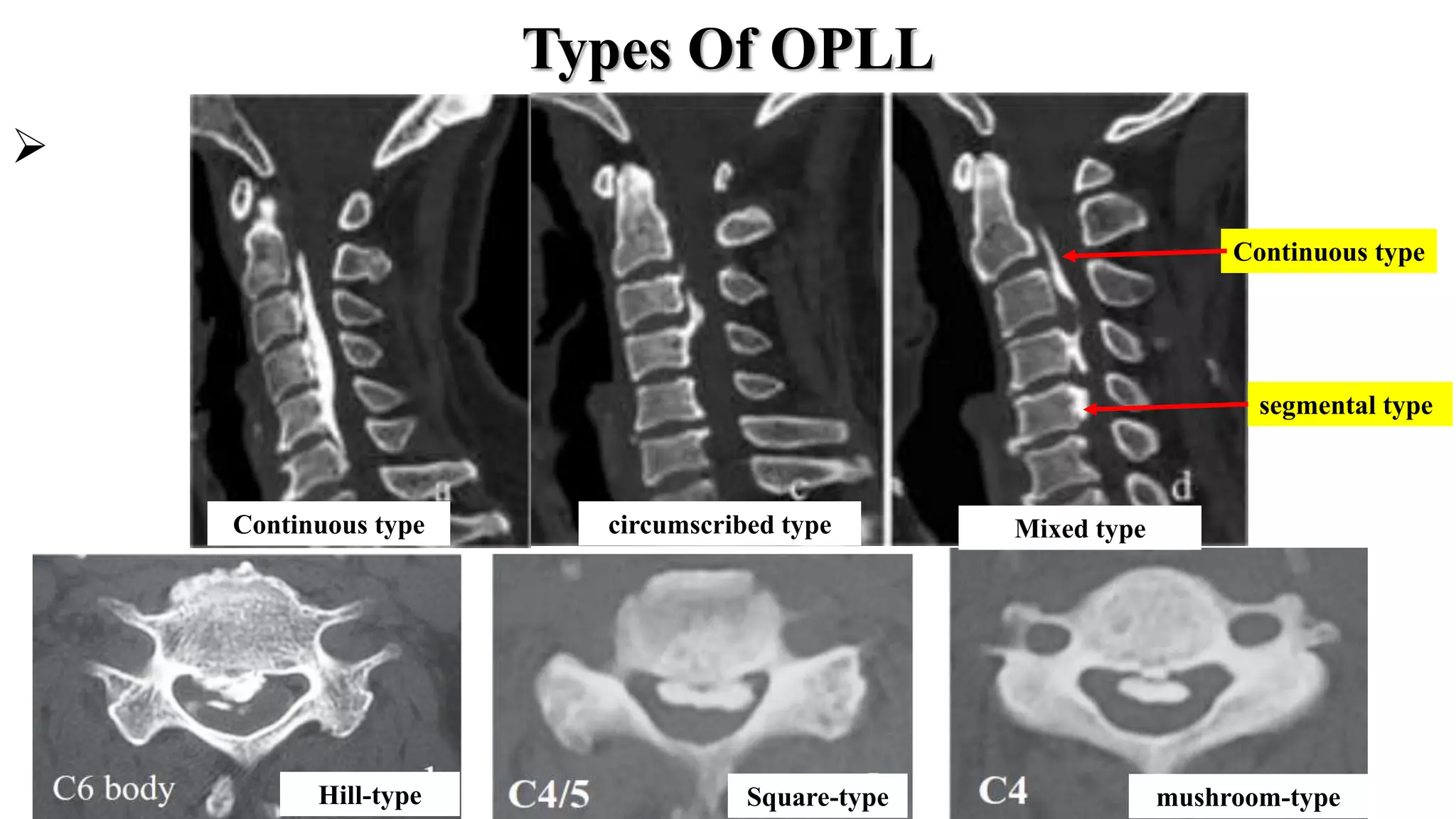
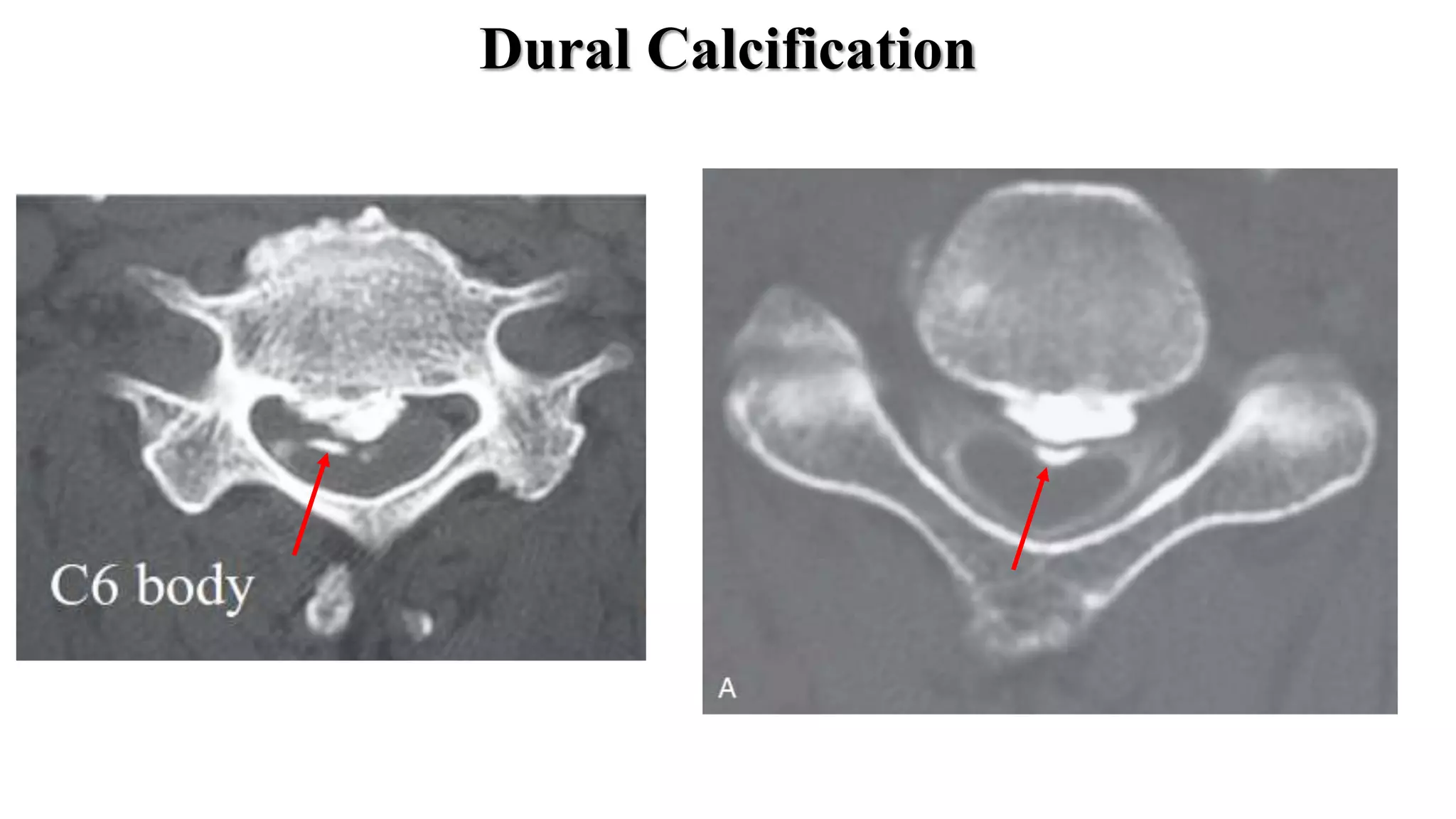
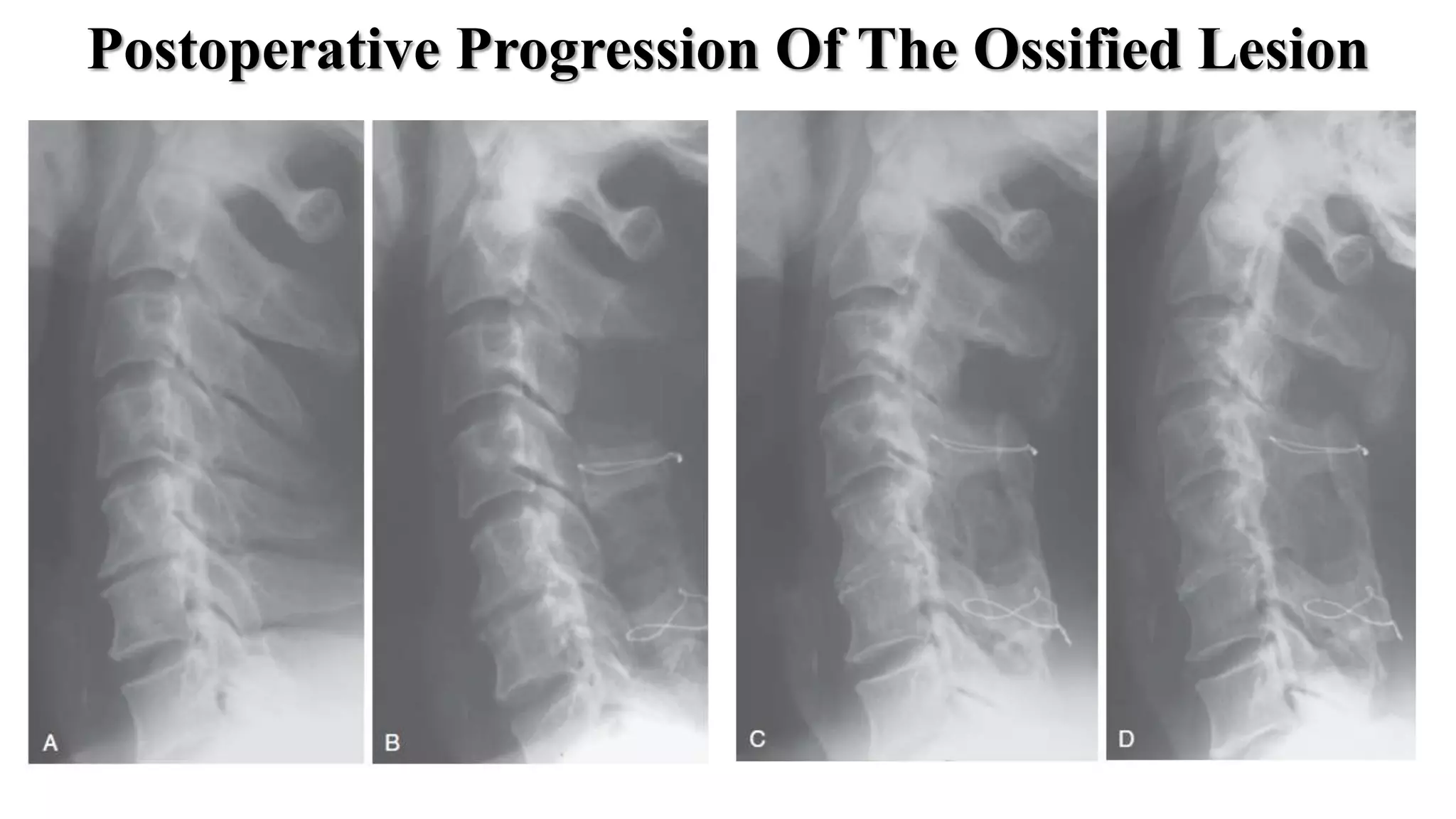
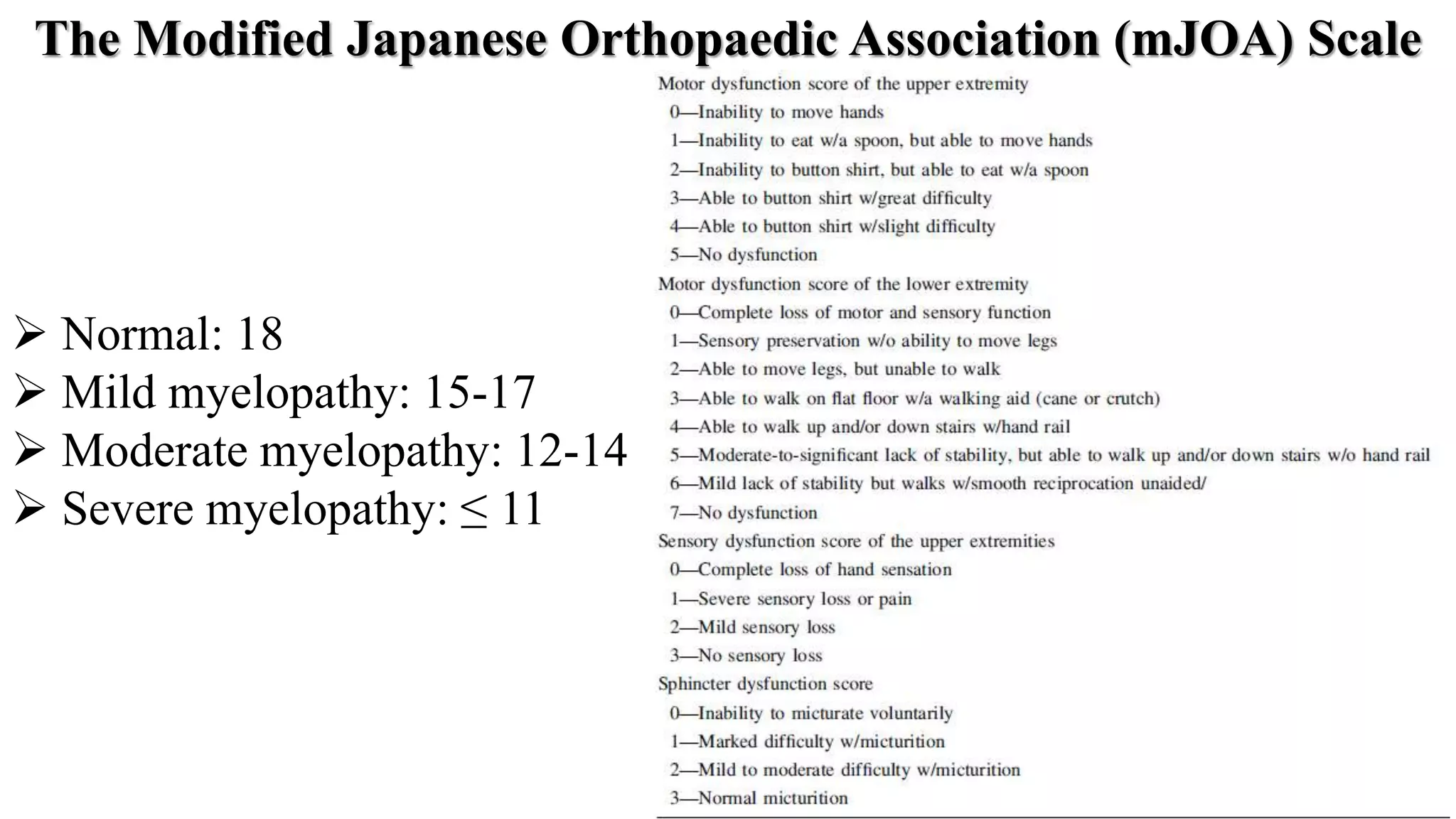
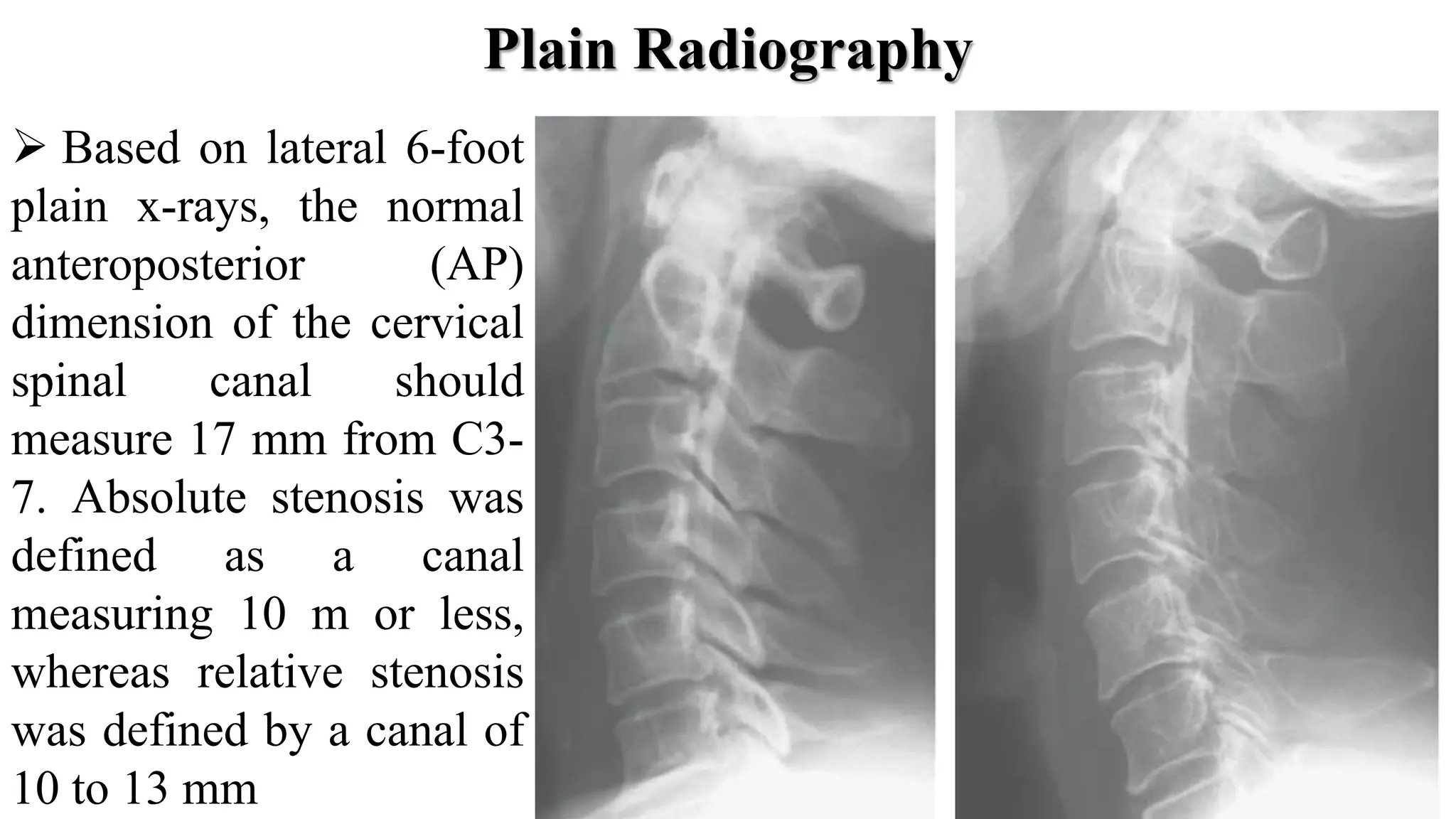
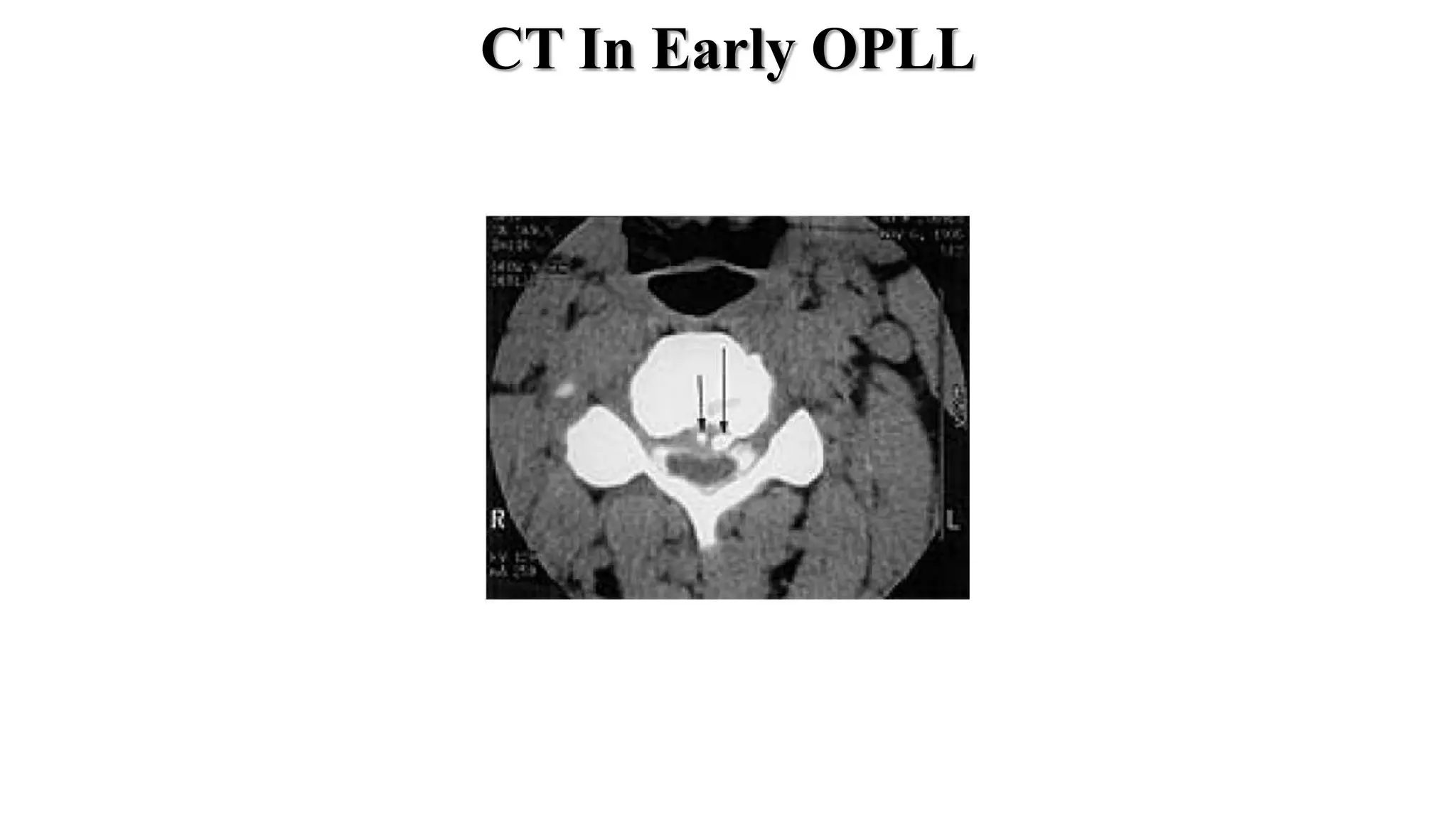
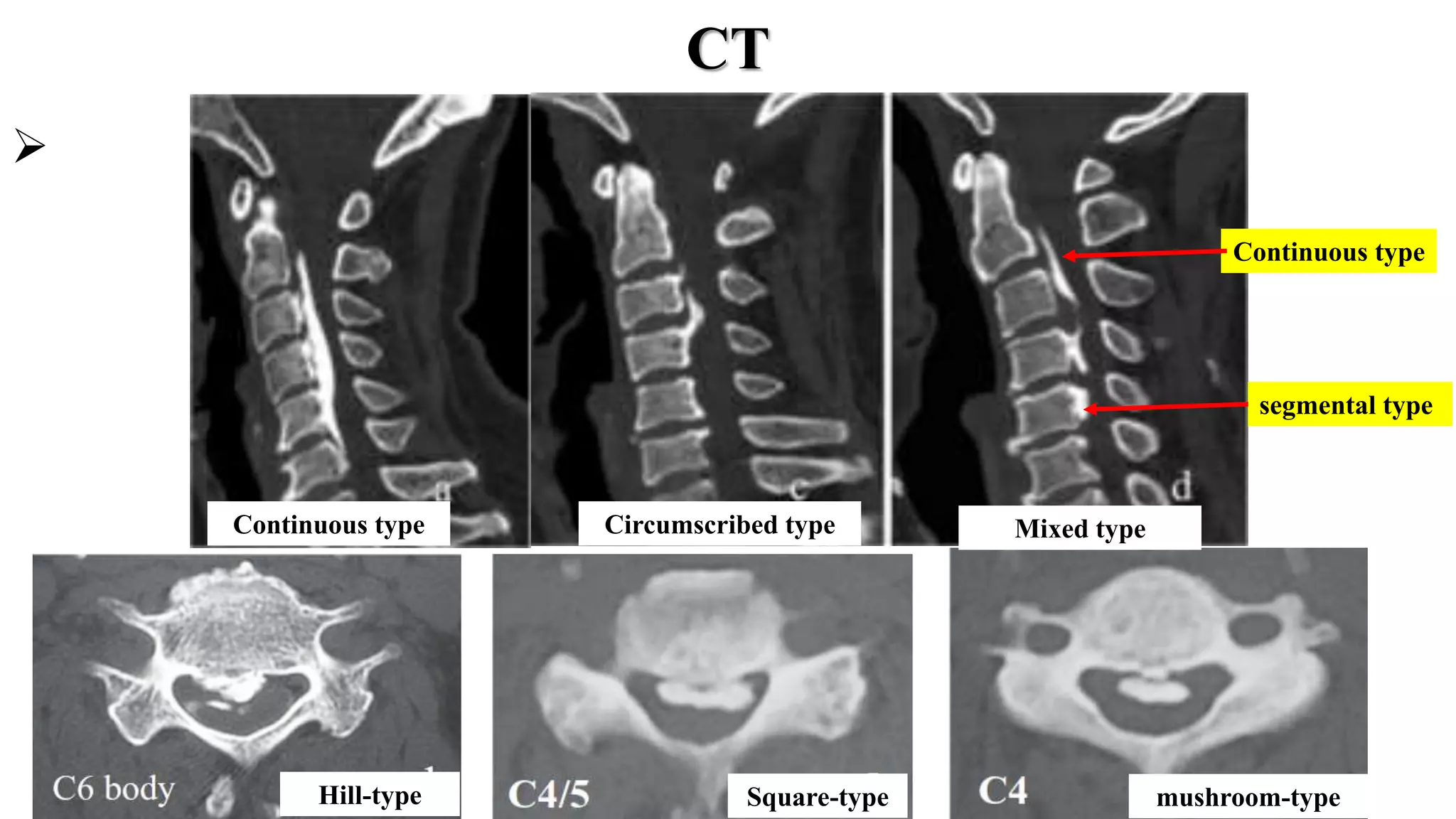
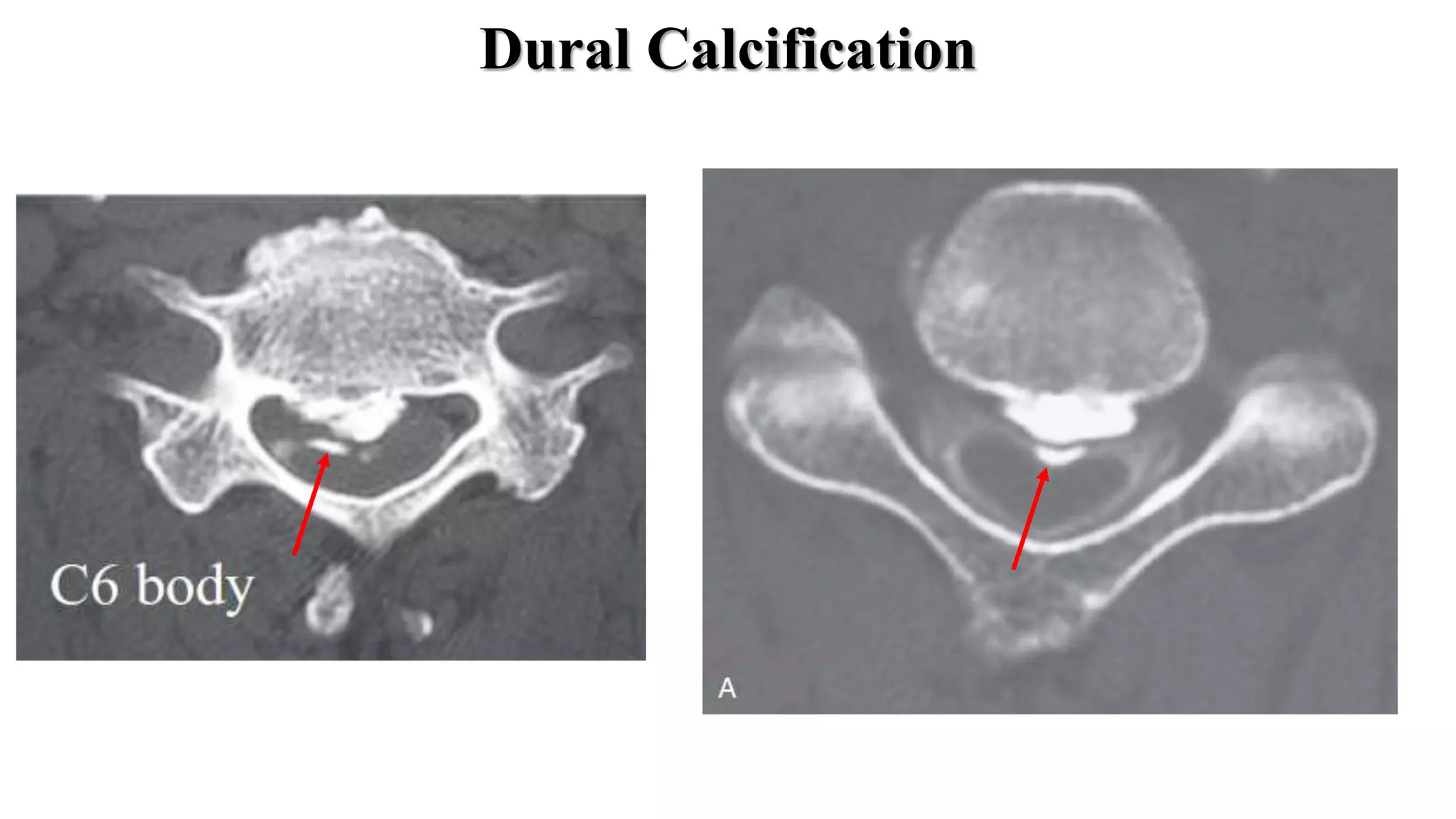
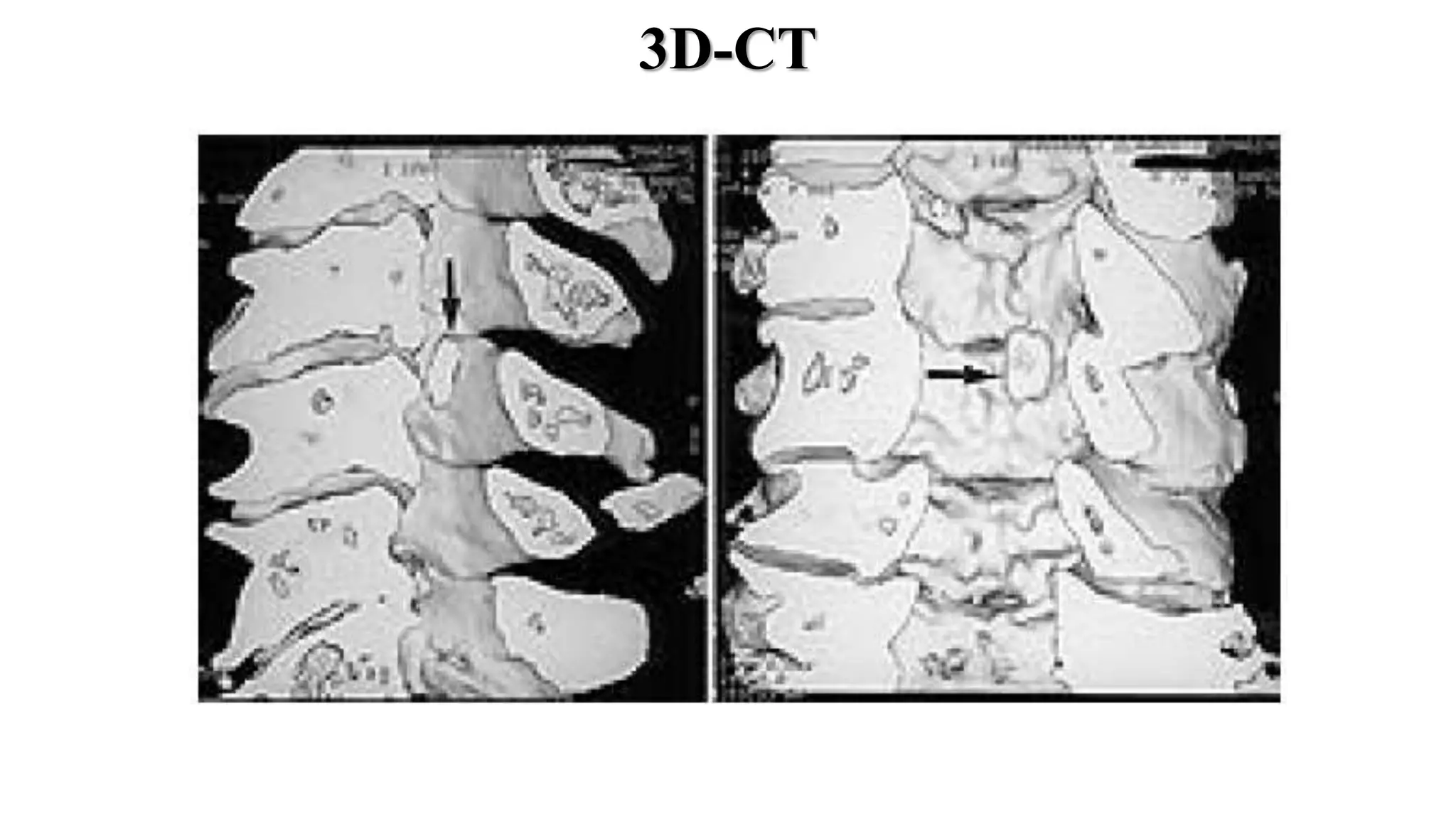
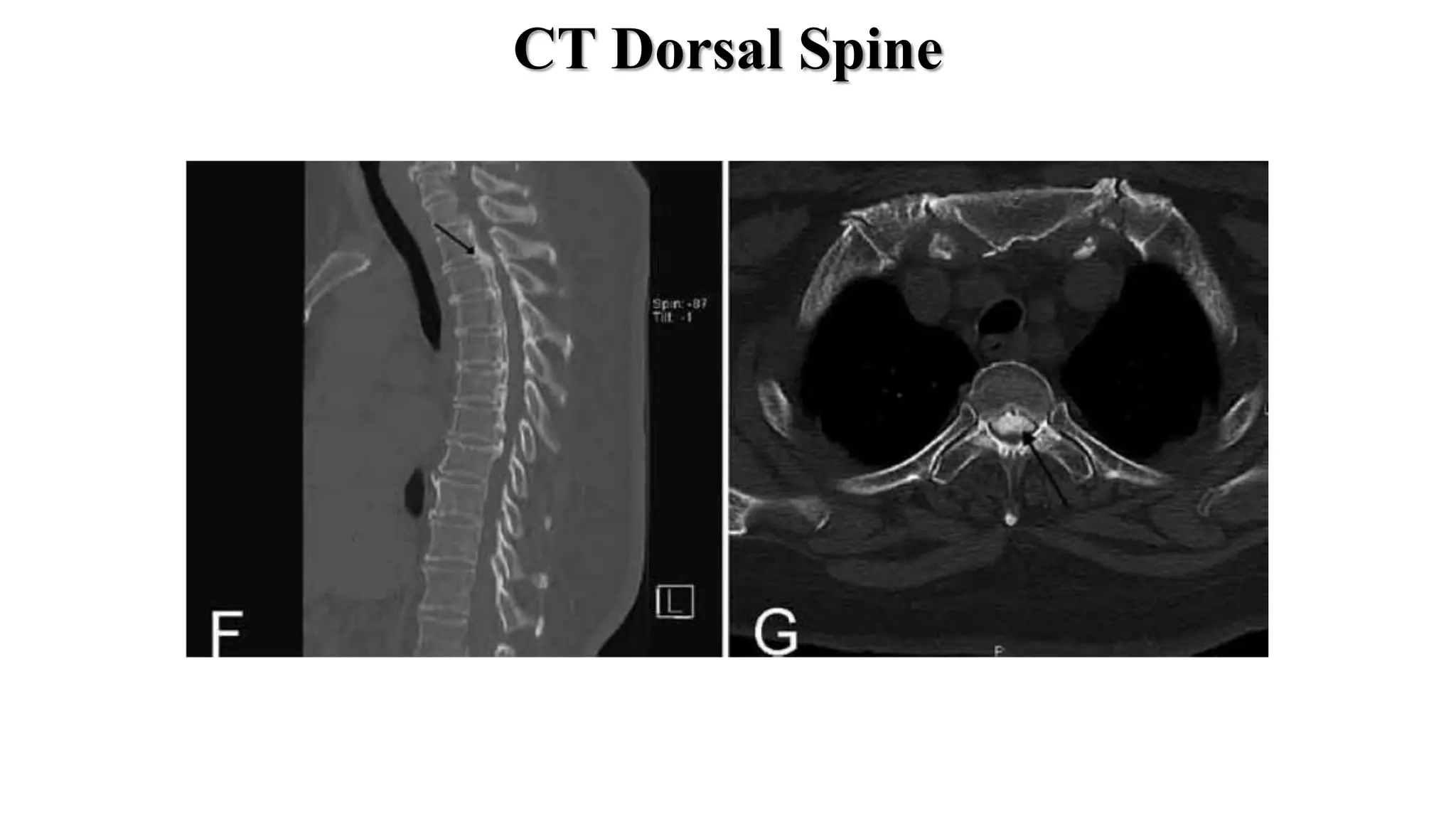
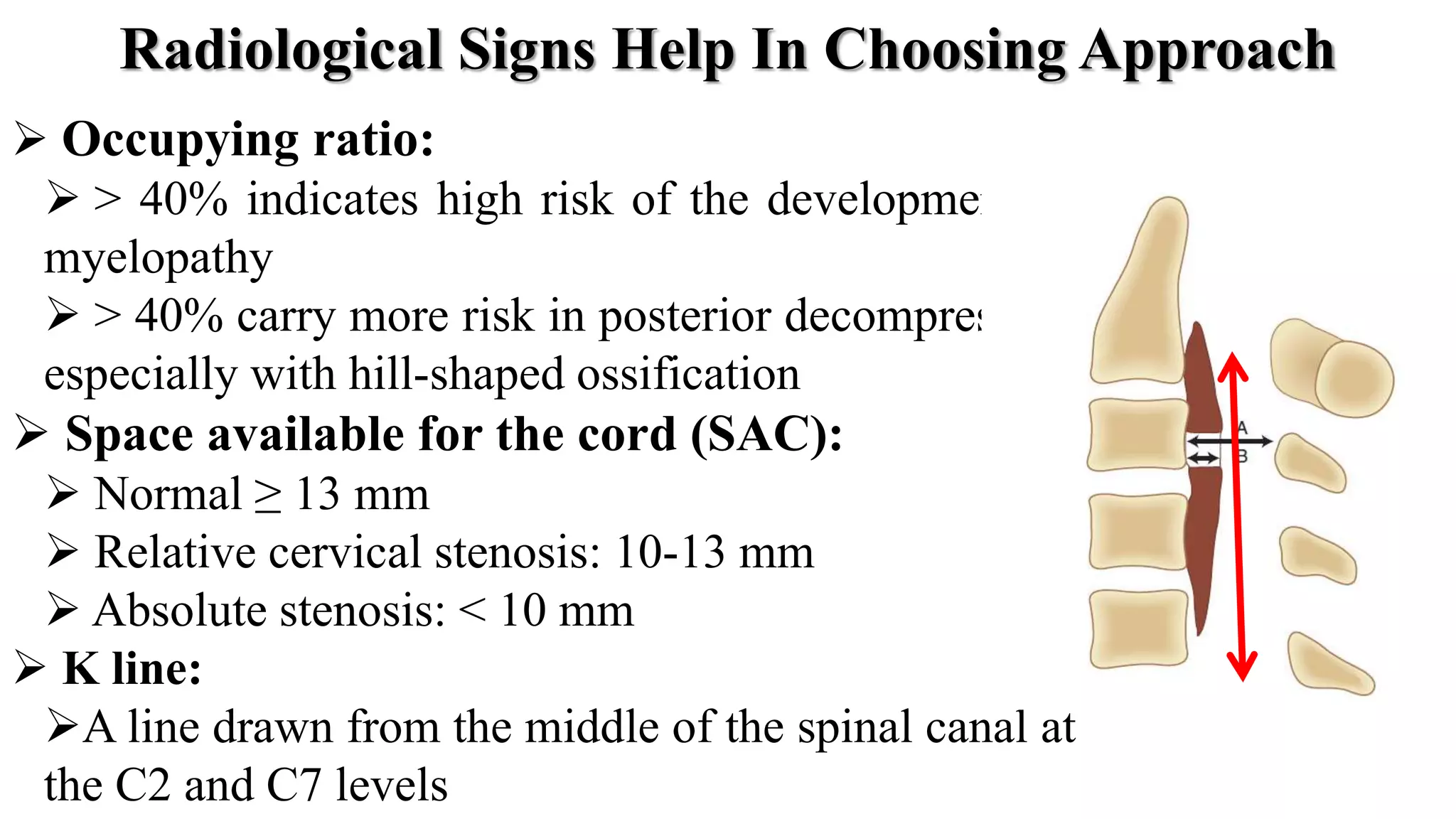
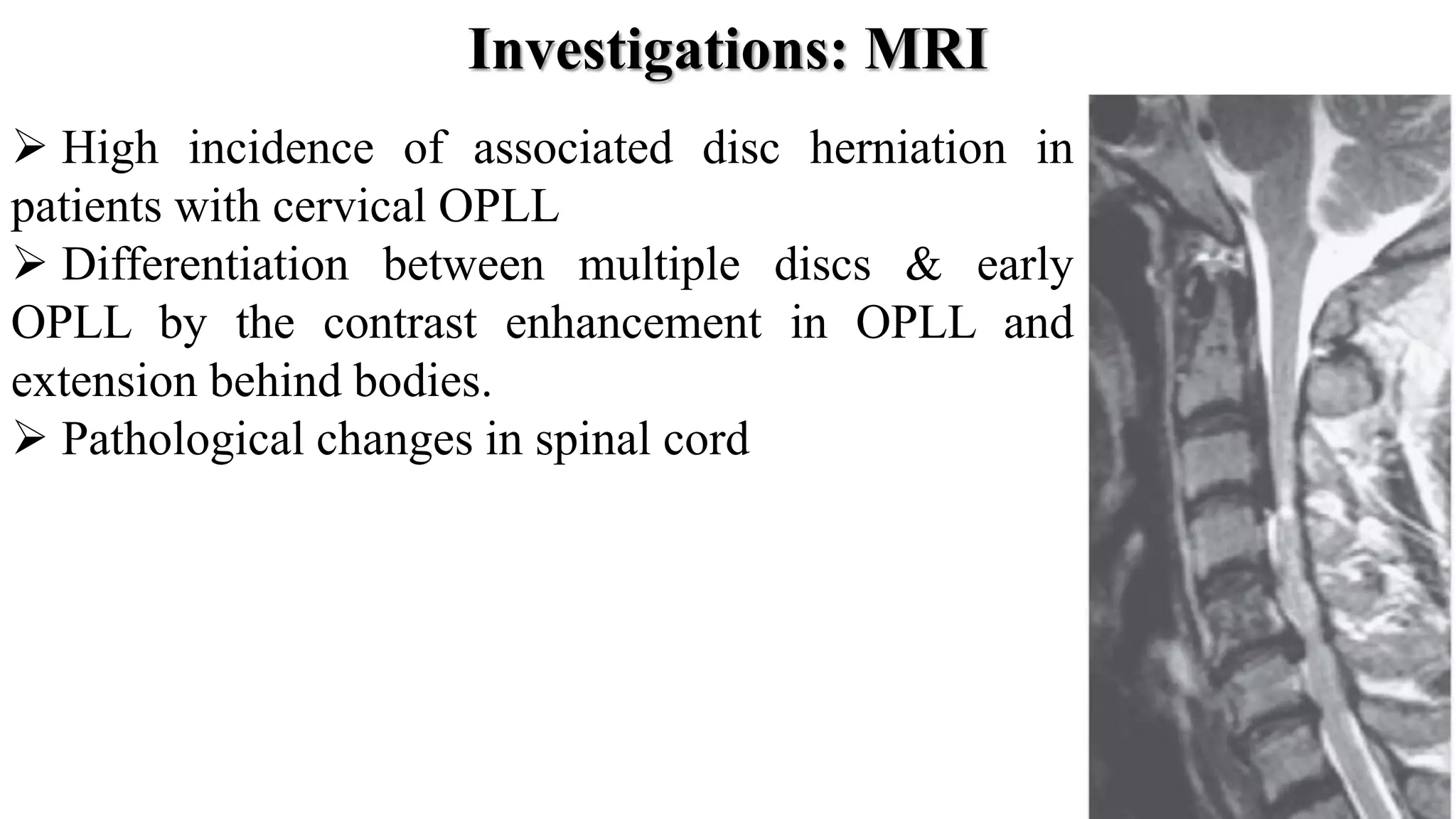
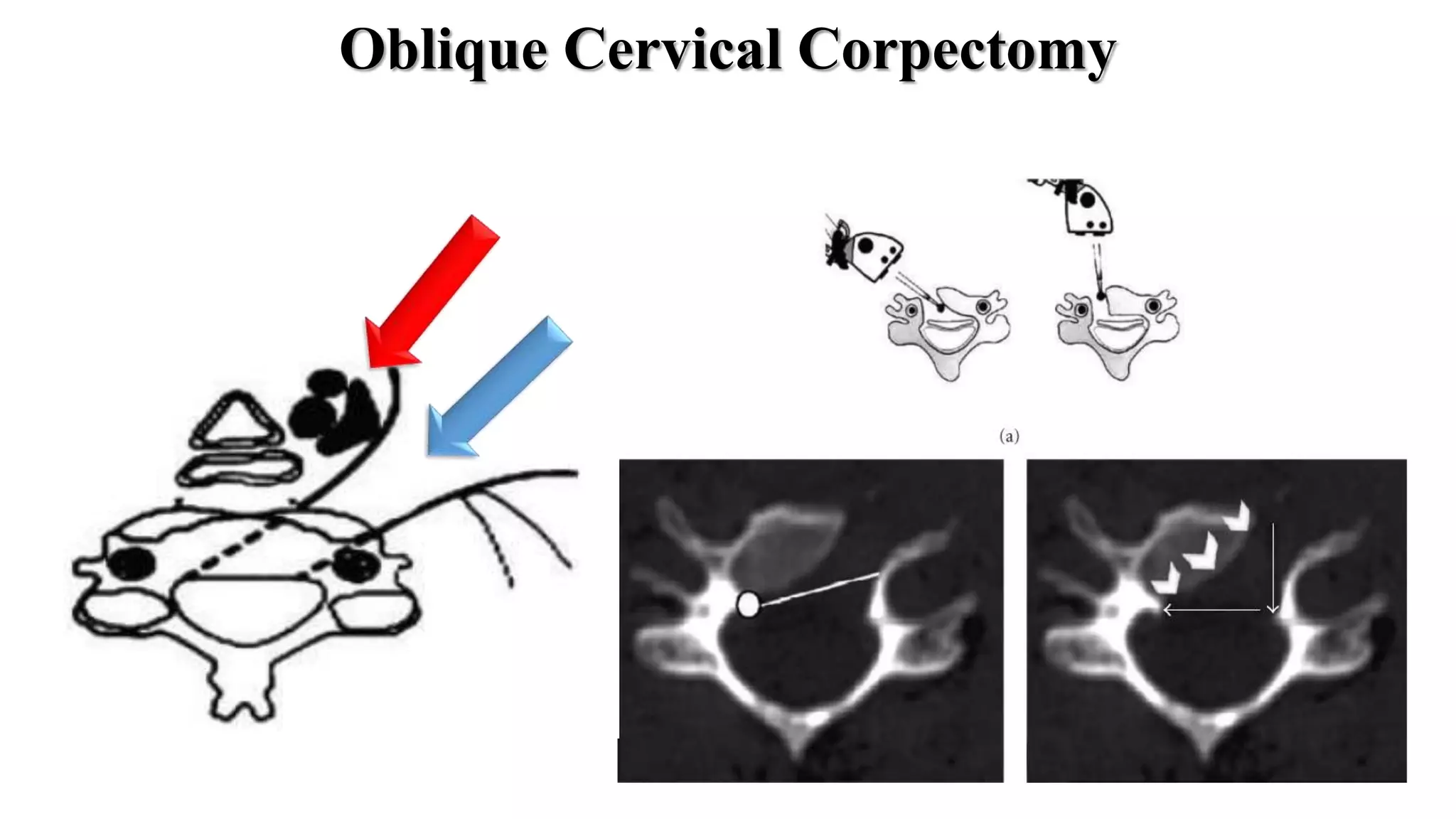
The document discusses the pathology, clinical presentation, diagnosis, and management of ossification of the posterior longitudinal ligament (OPLL). It covers the epidemiology, genetics, radiological features, and various surgical approaches for treating OPLL, including anterior corpectomy with fusion and posterior laminectomy with or without fusion. Anterior decompression is preferred for large occupying lesions or kyphosis, while posterior laminoplasty is an option for smaller lesions with a preserved lordosis. The goal of surgery is decompression with stabilization to prevent postoperative progression of OPLL.