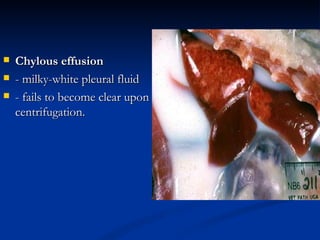
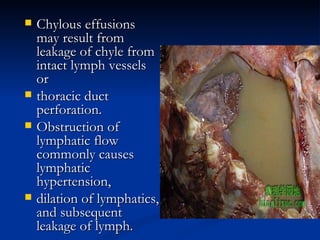
Chylothorax occurs when chyle, or lymph fluid containing fatty acids, leaks into the pleural space surrounding the lungs. It is uncommon in dogs and cats and usually secondary to other conditions like trauma, cancer, or heart disease. Diagnosis involves identifying milky white fluid in the chest that contains high levels of triglycerides. Treatment aims to drain the fluid and reduce lymph flow through dietary changes, medications, or duct ligation surgery, but prognosis is generally poor.