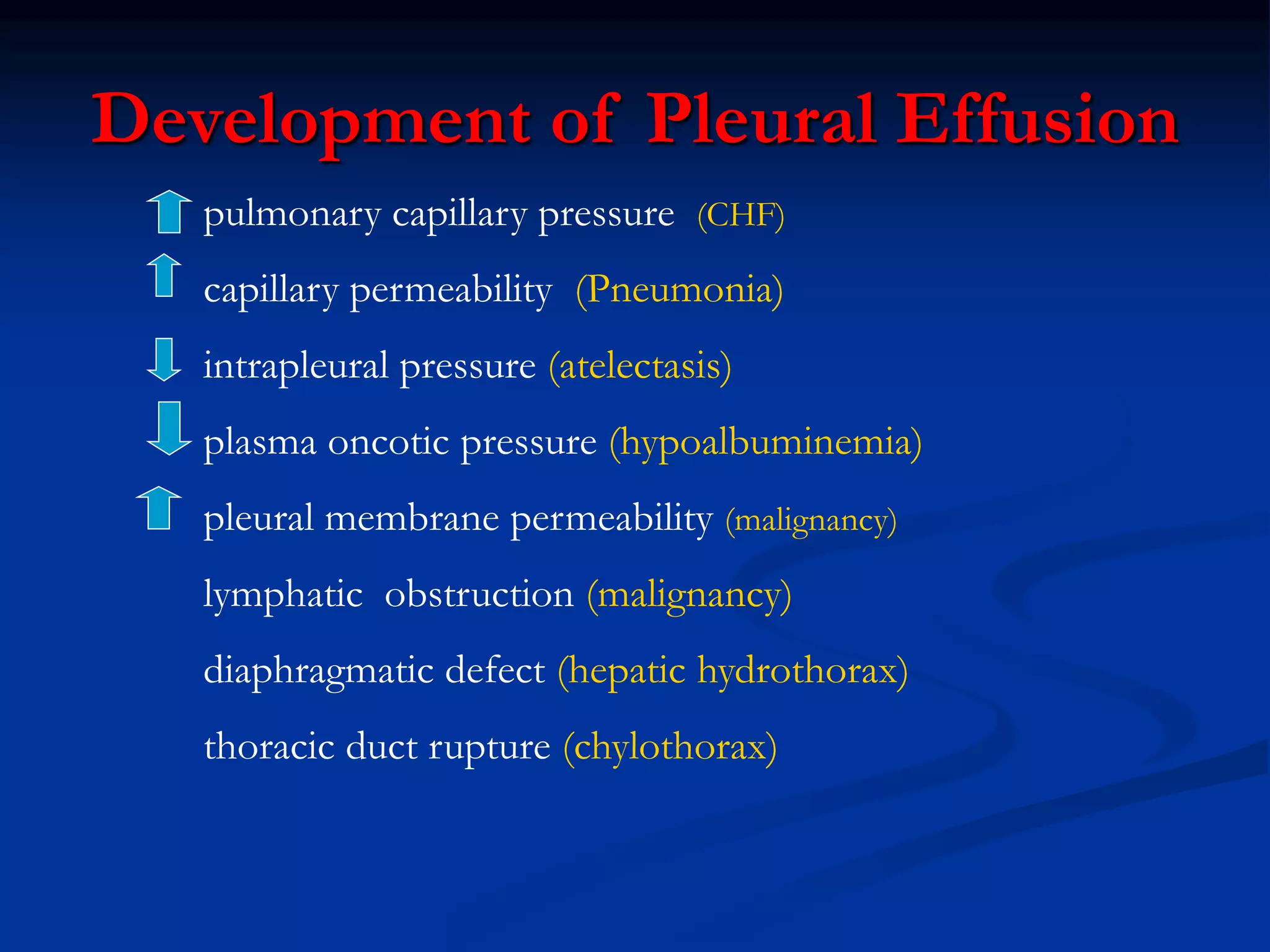
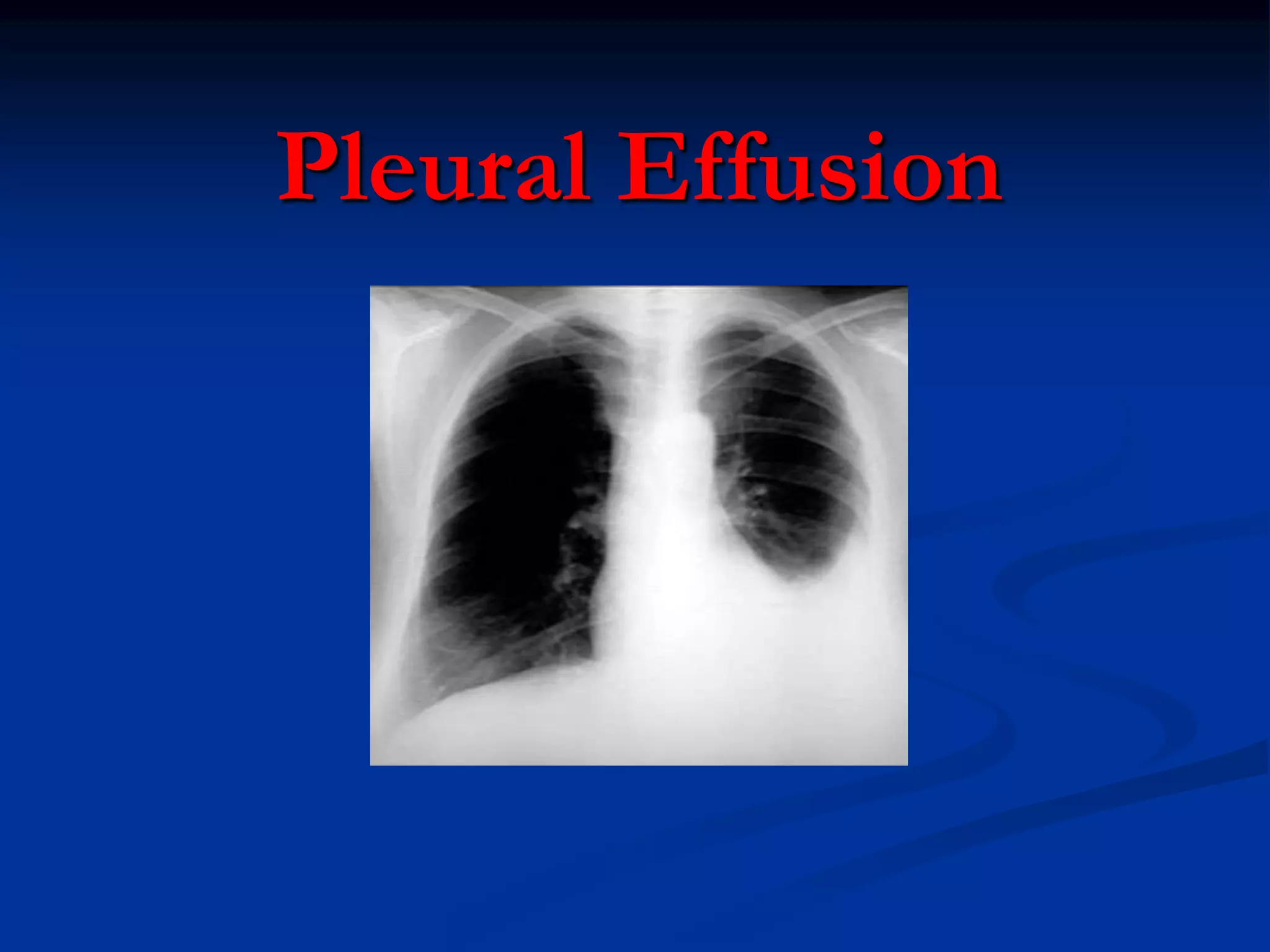
The document discusses pleural effusions, which are abnormal accumulations of fluid in the pleural space. Pleural effusions can be transudative or exudative in nature. Evaluation involves obtaining a history, physical exam, chest x-ray, and thoracentesis with pleural fluid analysis to determine the cause. Common causes include congestive heart failure, pneumonia, malignancy, and pulmonary embolism. Treatment depends on the underlying condition but may involve antibiotics, chest tube placement, or pleurodesis. Further tests like pleural biopsy or thoracoscopy may be needed if the cause is not clear from initial evaluation.




![6
Starling’s Law
Fluid movement
Starling’s law :
L . A [ (PCAP – PPl) – (CAP – Pl) ]
L: Filtration coefficient
A: Surface area
Cap: Capillary
Pl: Pleural](https://image.slidesharecdn.com/12-pleuraleffusion-220819023314-8718cd6c/75/12-PLEURAL-EFFUSION-ppt-6-2048.jpg)