This document discusses chronic pancreatitis, including its causes, pathogenesis, classification, clinical presentation, diagnostic evaluation, complications, and surgical and non-surgical management. Some key points include:
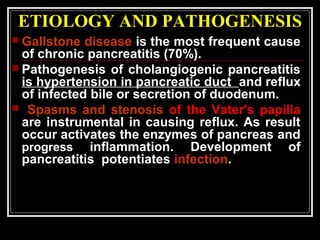
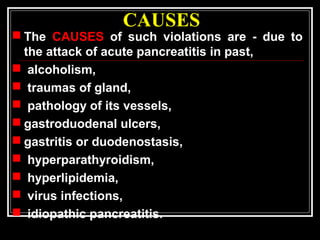
- Gallstone disease is the most common cause, accounting for 70% of cases. Other causes include alcoholism, trauma, genetic factors.
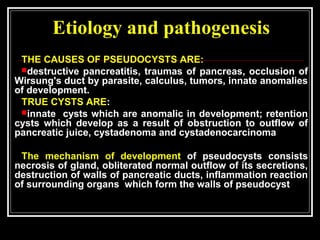
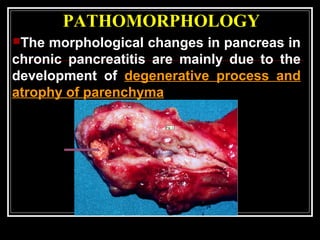
- Pathogenesis involves reflux of infected bile or duodenal contents into the pancreatic ducts, causing inflammation and activation of pancreatic enzymes.
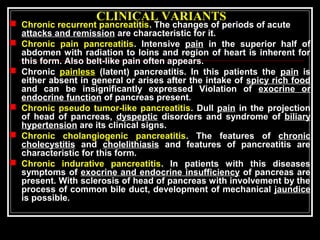
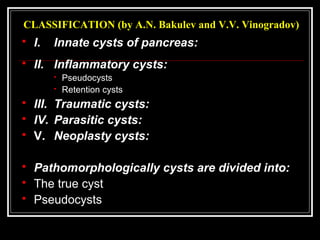
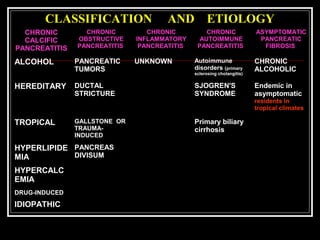
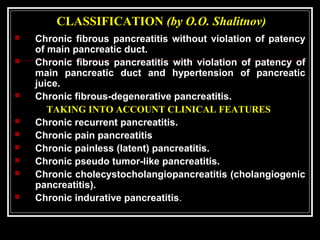
- Classification is based on etiology, presence of pancreatic duct obstruction, and clinical features such as pain pattern.
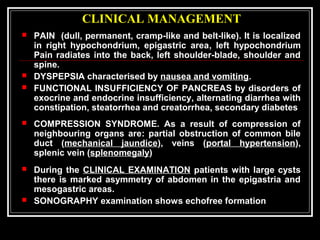
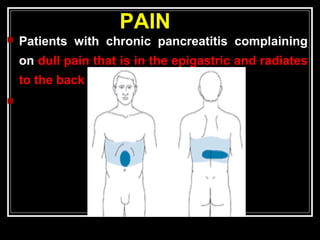
- Presentation includes recurrent upper abdominal pain, weight loss from malabsorption, and endocrine and exocrine pancreatic insufficiency
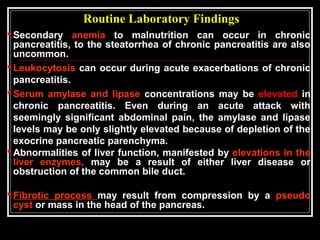
![TESTS FOR CHRONIC PANCREATITIS
MEASUREMENT OF PANCREATIC PRODUCTS IN BLOOD
I A Enzymes
B Pancreatic polypeptide
MEASUREMENT OF PANCREATIC EXOCRINE SECRETION
II A Direct measurements
1 Enzymes
2 Bicarbonate
B Indirect measurement
1 Bentiromide test
2 Schilling test
3 Fecal fat, chymotrypsin, or elastase concentration
4 [14
C]-olein absorption
IMAGING TECHNIQUES
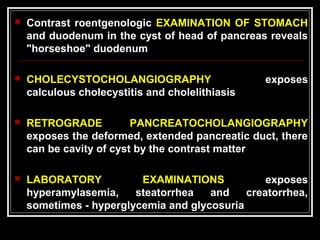
III A Plain film radiography of abdomen
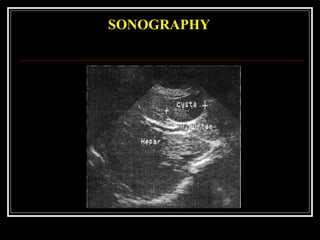
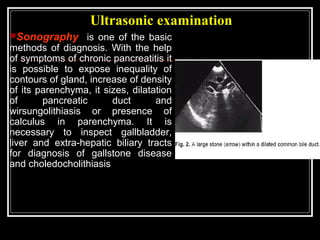
B Ultrasonography
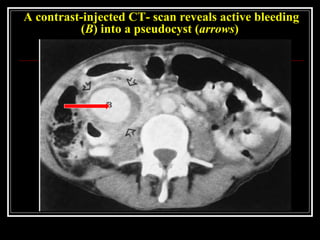
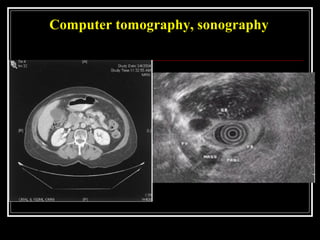
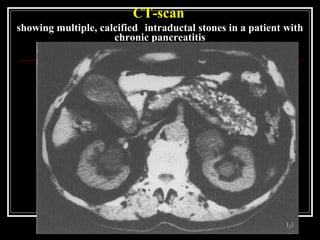
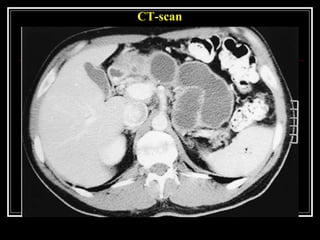
C Computed tomography
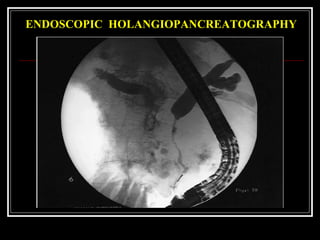
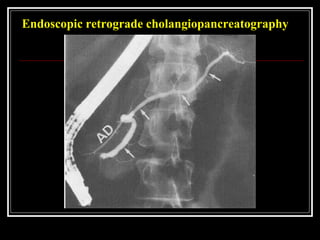
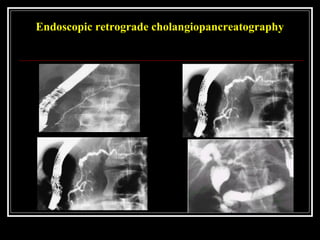
D Endoscopic retrograde cholangiopancreatography
E Magnetic resonance cholangiopancreatography
F Endoscopic ultrasonography
G Relaxation duodenogram](https://image.slidesharecdn.com/lecturechronicpancreatitis2-160124125826/85/Lecture-chronic-pancreatitis-20-320.jpg)