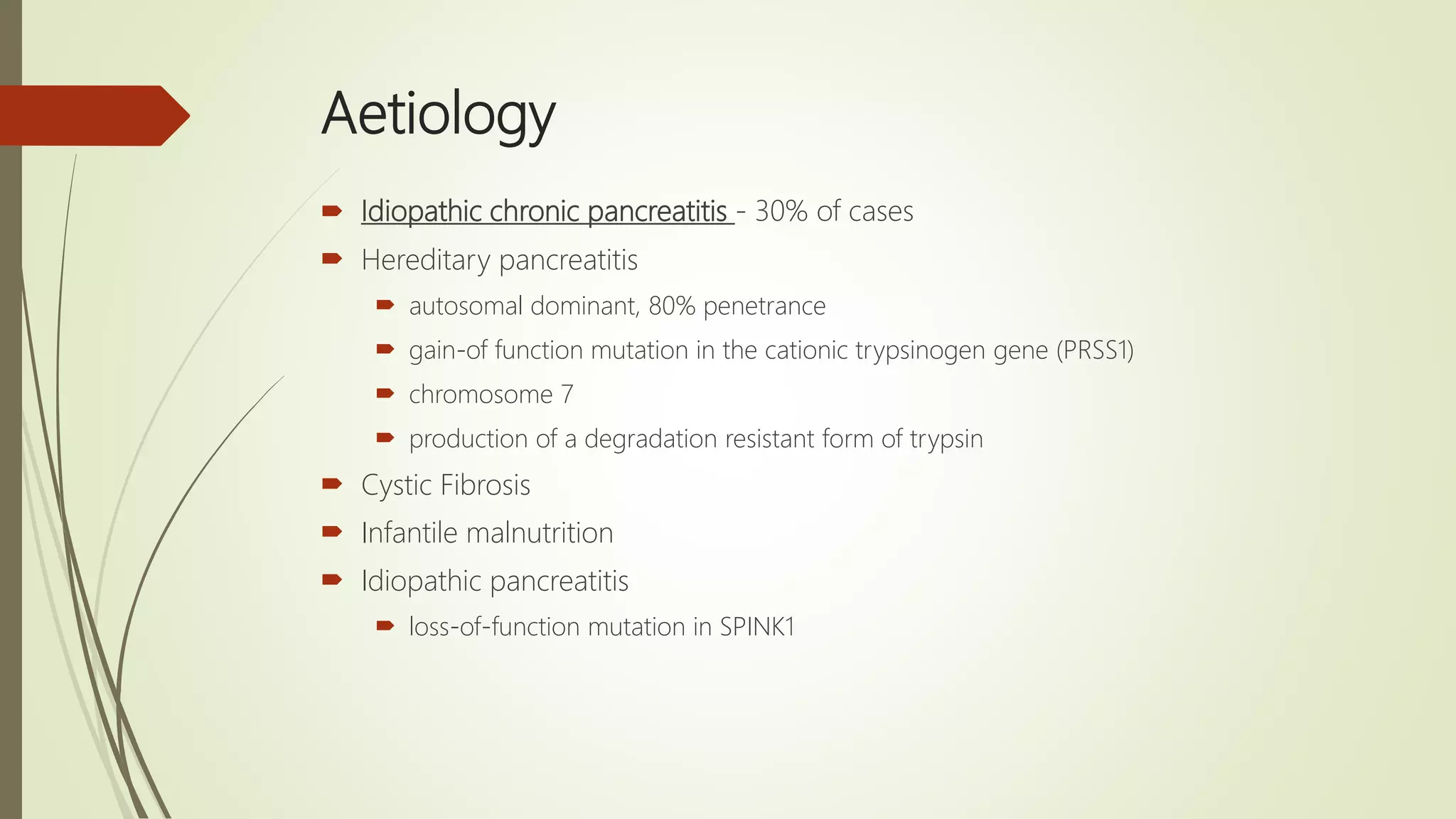
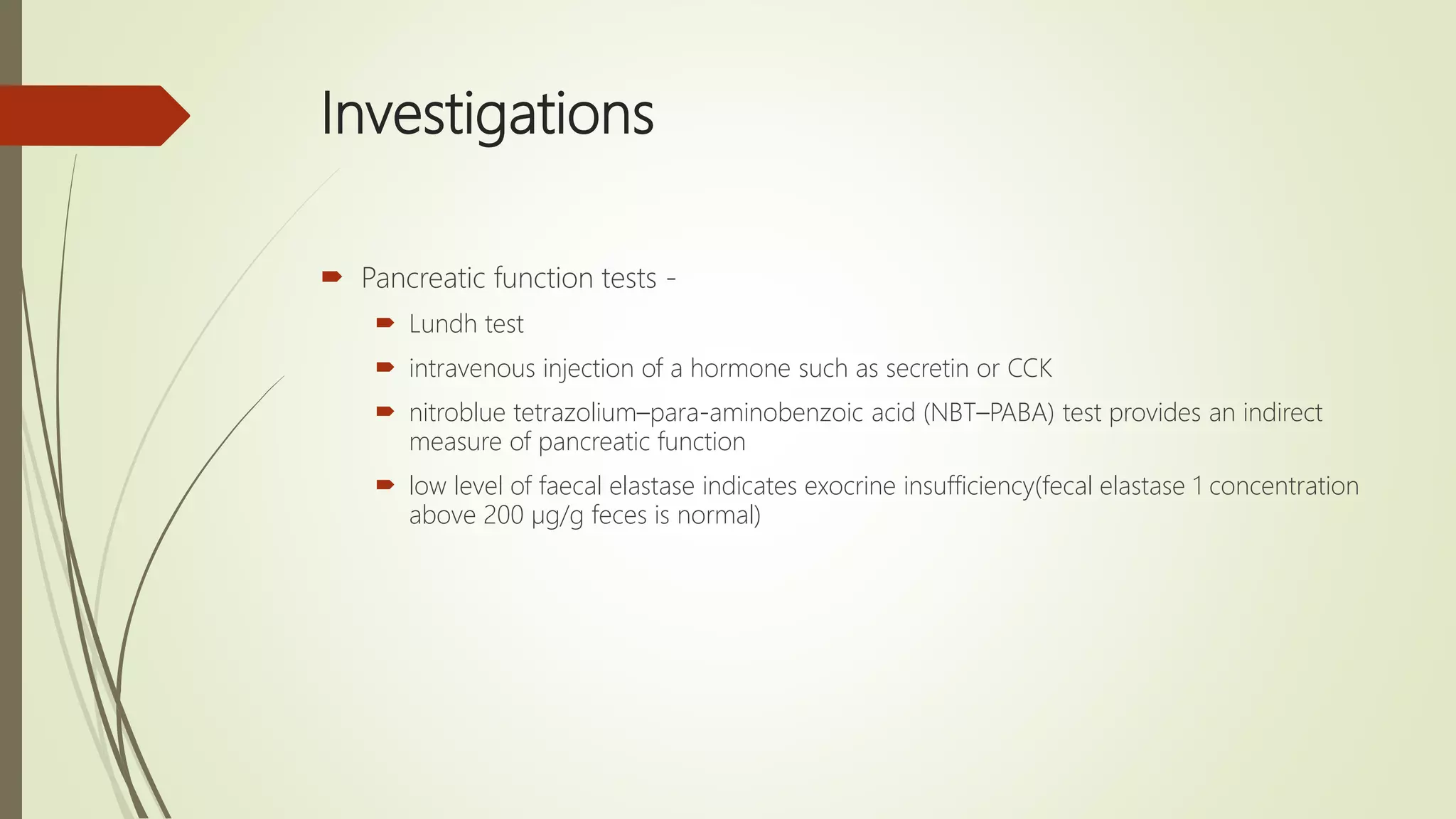
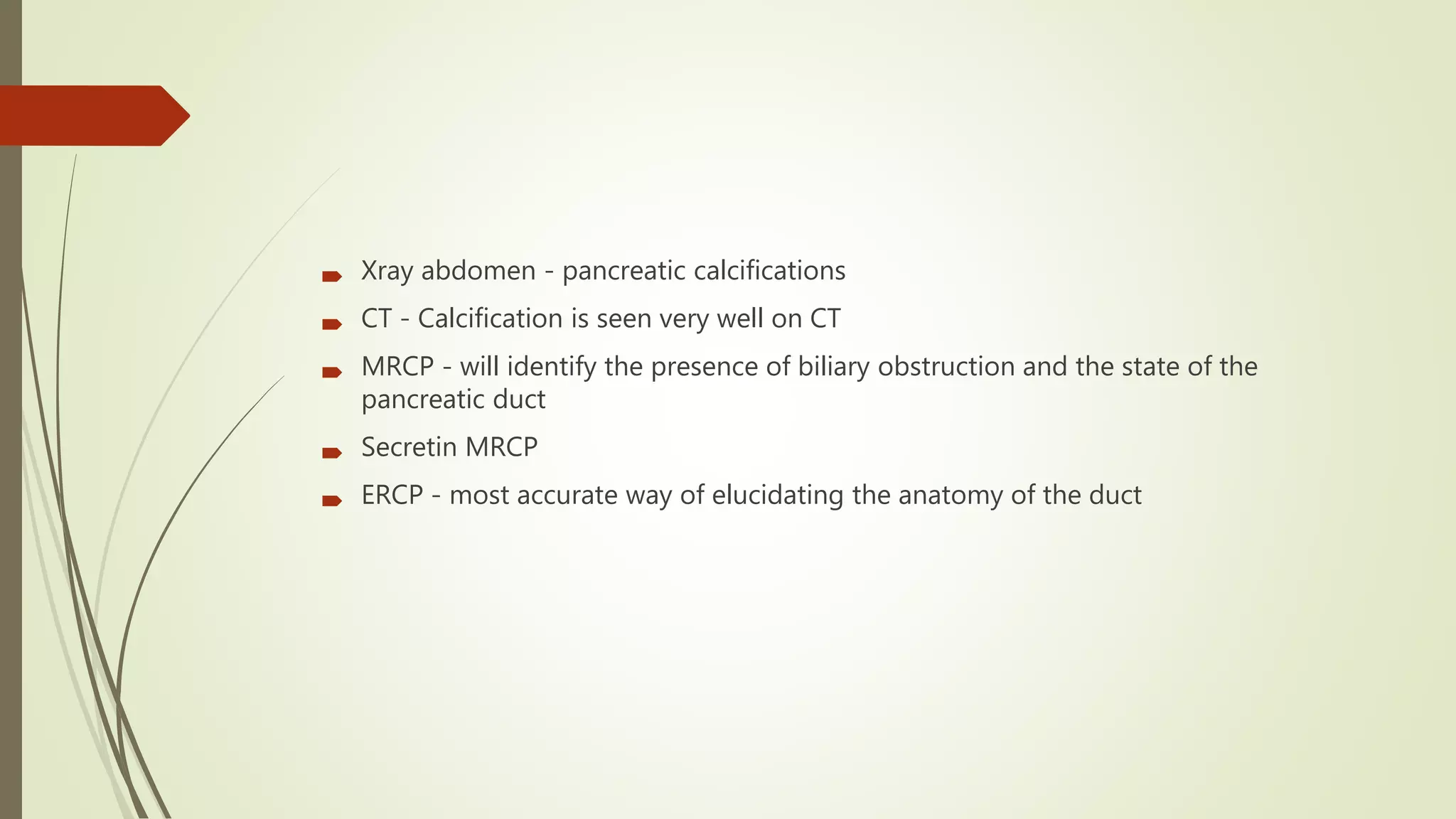
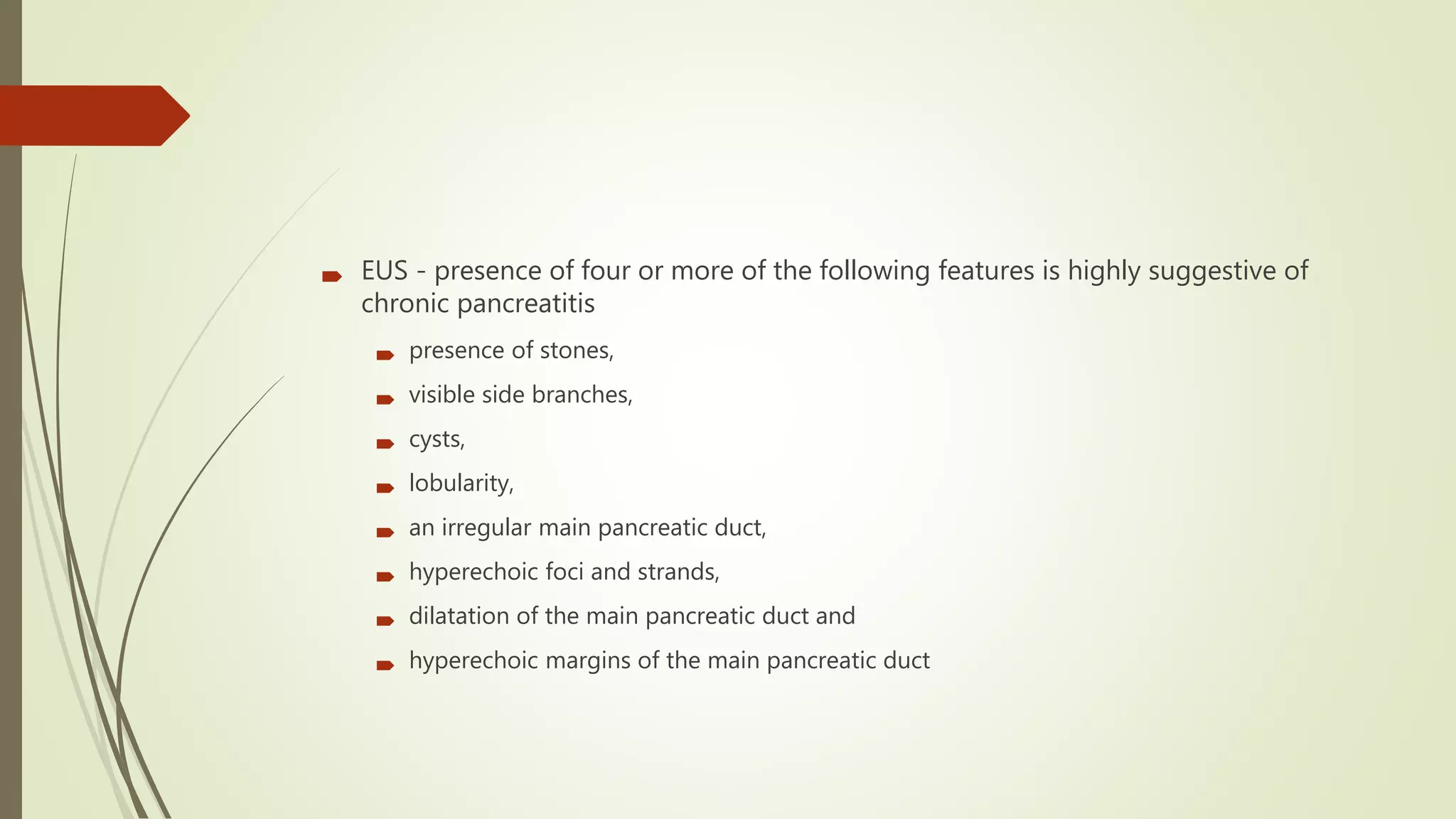
Chronic pancreatitis is a progressive inflammatory disease of the pancreas characterized by irreversible destruction of pancreatic tissue. It commonly causes severe abdominal pain and can lead to exocrine and endocrine insufficiency over time. The most common causes are alcohol consumption and smoking. Diagnosis involves pancreatic function tests, imaging like CT or MRCP to identify changes in the pancreas and pancreatic duct. Treatment focuses on managing pain, treating underlying causes, nutrition support, and in some cases endoscopic or surgical interventions. The prognosis is often poor with declining health and function over time and an increased risk of pancreatic cancer with longstanding disease.