This document discusses acute peritonitis, including:
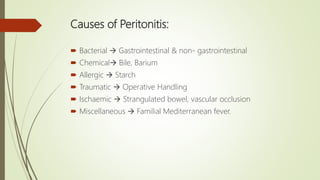
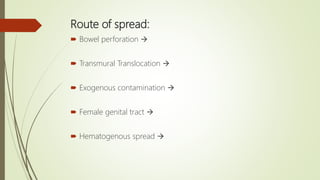
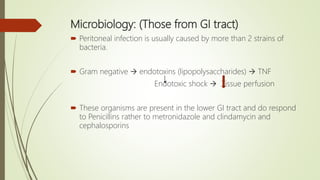
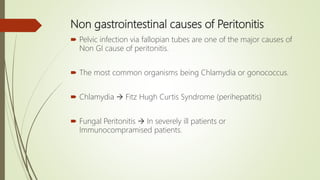
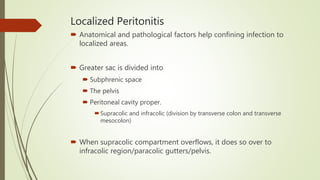
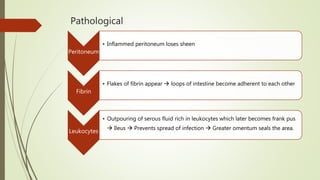
- Peritonitis is defined as inflammation of the peritoneum and can be localized or generalized. It is usually caused by bacterial infection entering through the gastrointestinal tract or other sources.
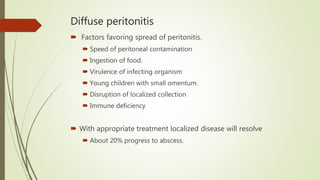
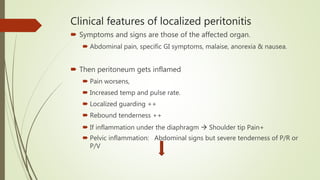
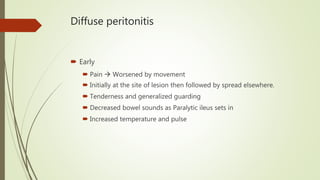
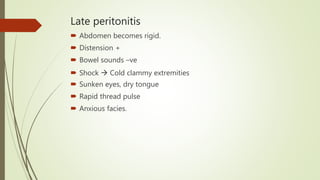
- Symptoms depend on whether it is localized or diffuse. Localized peritonitis causes pain specific to the affected organ, while diffuse peritonitis causes generalized abdominal pain and tenderness.
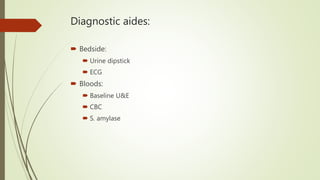
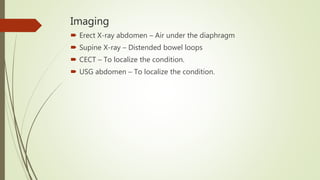
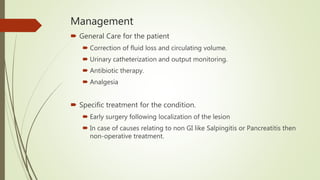
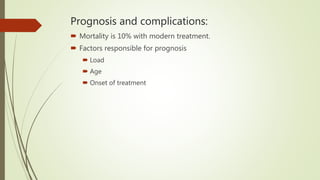
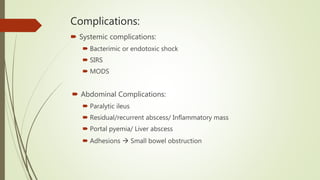
- Treatment involves antibiotics, fluid resuscitation, and sometimes surgery to address the underlying cause and drain any abscesses. Outcomes depend on several factors but mortality is around 10% with prompt treatment. Complications can include shock, bowel obstruction, and residual infections.