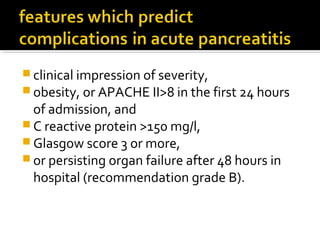
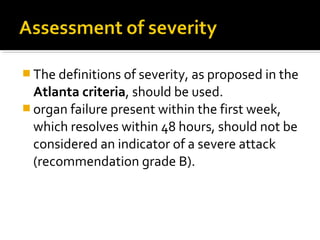
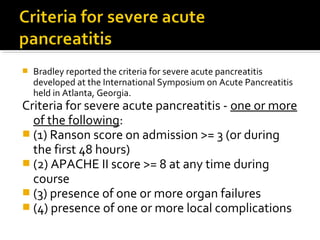
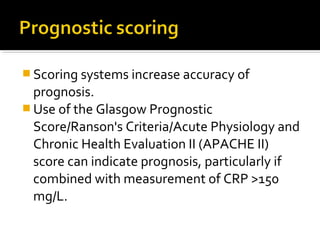
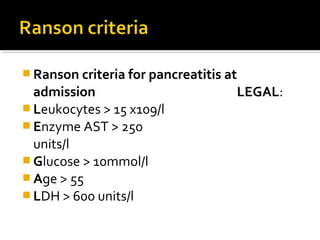
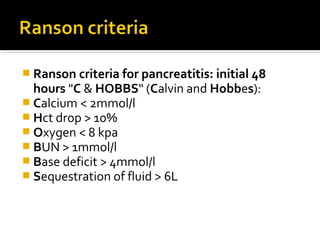
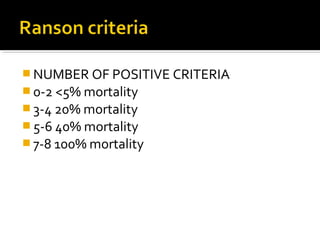
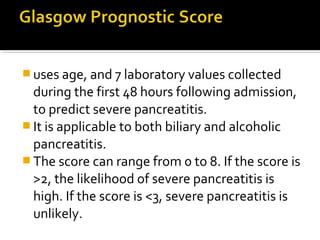
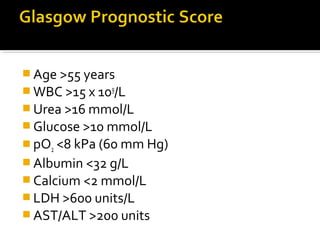
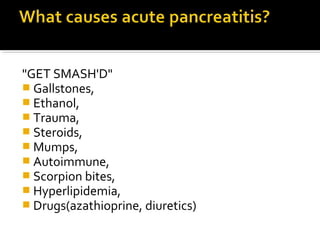
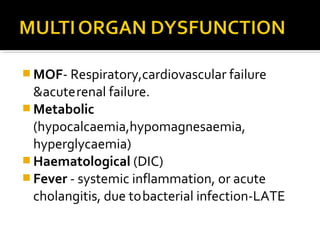
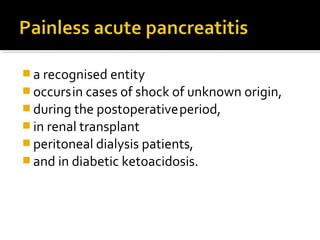
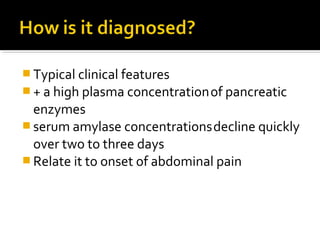
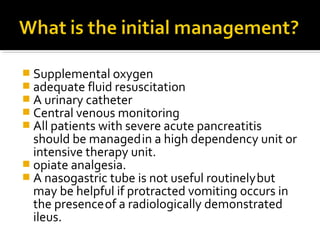
The document discusses acute pancreatitis, including causes, clinical features, diagnosis, severity grading, management, and prognosis. Gallstones and alcohol are the most common causes. Scoring systems like Ranson criteria and APACHE II can help indicate severity and prognosis. Management involves treatment of the underlying cause, supportive care, and monitoring for complications like pancreatic necrosis which may require intervention.

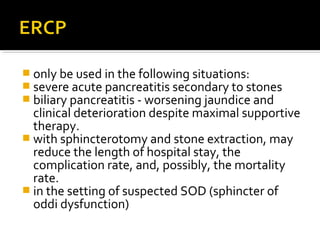
![ imaging of the common bile duct is required.
If the presence of stones in the common bile duct
is confirmed, a cholecystectomy with common
bile duct exploration (either surgical or
postoperatively with endoscopic retrograde
cholangiopancreatography [ERCP]) should be
performed during the same hospitalisation in
mild to moderate disease soon after the attack
resolves.
A longer delay, even of a few weeks, is associated
with a high recurrence (80%) of acute pancreatitis
and re-admission](https://image.slidesharecdn.com/acutepancreatitis-141013042134-conversion-gate01/85/Acute-pancreatitis-27-320.jpg)