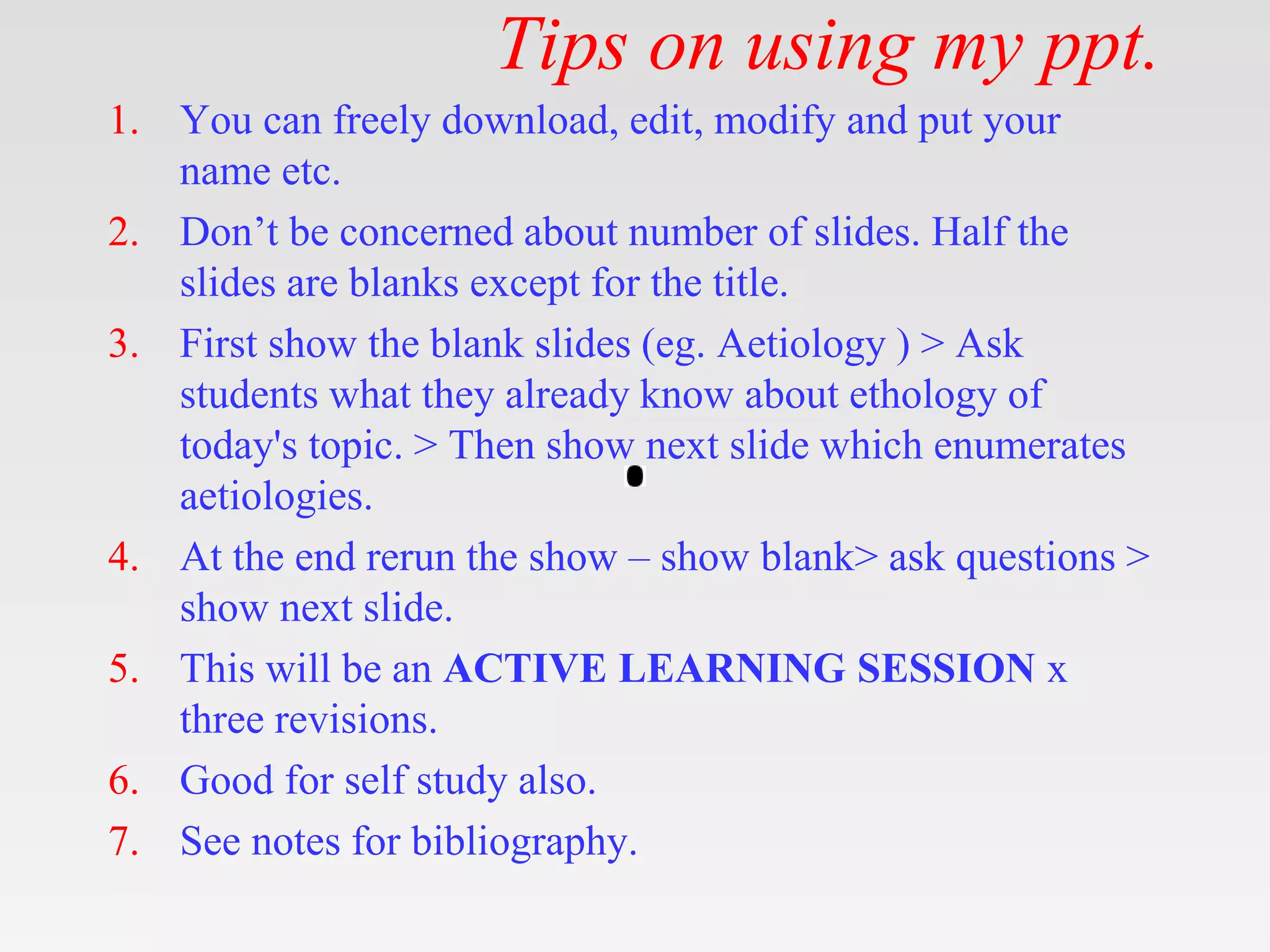
The document provides tips for using a PowerPoint presentation on chronic pancreatitis. It recommends:
1) Allowing free editing and modification of the slides.
2) Noting that half the slides are blank except for the title to allow for active student participation.
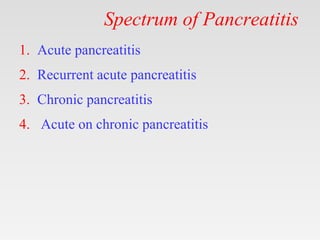
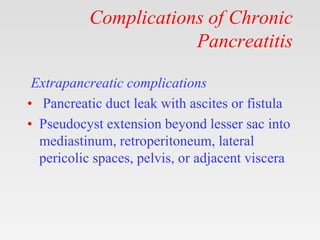
3) Showing blank slides, asking students for input, and then showing slides with content.
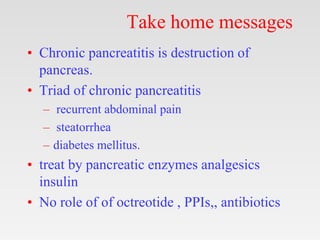
4) Repeating this process of blank slides followed by content slides.
5) This approach facilitates active learning through multiple revisions.